Three Step Test for Cyclovertical Muscle Palsy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease
Hypertropia is an ocular disorder characterized by either constant or intermittent upwards deviation of one eye in comparison to the other eye. A hypotropia describes downward deviation of one eye compared to the other. By convention, vertical strabismus is typically labelled by the higher, or hypertropic, eye. The most common type of vertical strabismus is a palsy of the fourth cranial nerve (CN IV), also called the trochlear nerve,[1] which innervates the superior oblique muscle. The trochlear nerve has the longest intracranial course and is the only cranial nerve that exits dorsally from the brainstem. This long course of the trochlear nerve makes it susceptible to acquired injury.[2] The most frequent cause of injury to the trochlear nerve is trauma.[3] One common manifestation of a superior oblique palsy is double vision, which is relieved by tilting the head towards the unaffected side.[2] Tilting the head toward the affected side would worsen double vision by leading to greater separation of the two images seen by the patient.[2] Below, we discuss diagnostic procedures for hypertropia.
Diagnostic procedure
The three-step test, also known as the Parks-Bielschowsky three-step test or the Parks-Helveston three-step test, is a diagnostic test used to identify which muscle is paretic in the case of an acquired hypertropia. This method uses a cover test to measure the amount of deviation in different head positions. It was first described by Bielschowsky in 1935 and later popularized by Marshall M. Parks. This test is most useful in diagnosing superior oblique palsies in clinical practice.[4][5]
The three-step test may also be used to diagnose the less common inferior oblique or vertical rectus muscle palsy and can be used in differentiating DVD from other vertical strabismus. It is designed for the diagnosis of a single paretic vertical muscle and is unreliable when there are multiple paretic muscles or in restrictive strabismus. This test may also help in identifying if a superior rectus palsy is true or simulated in a patient with an inhibitional palsy of the contralateral antagonist.
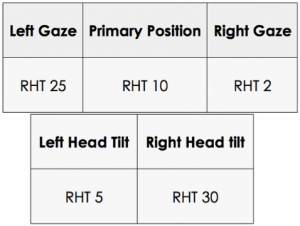
Prisms are used to quantify misalignment of the eyes in primary position, side gazes, and head tilts. Smaller deviations may be quantified using prisms and a Maddox rod or red filter.[6] Using these measurements:
- Determine which eye is hypertropic in primary position.
- The impacted muscle will be a depressor of the higher eye (inferior rectus or superior oblique) or an elevator of the lower eye (superior rectus or inferior oblique)
- Determine whether the hypertropia increases on right or left gaze.
- If worse in left gaze, for a paretic muscle, the superior or inferior oblique muscle in the right eye or the superior or inferior rectus in the left eye is affected
- If worse in right gaze, for a paretic muscle, the superior or inferior oblique muscle in the left eye or superior or inferior rectus muscle in the right eye is affected
- Determine if the hypertropia increases upon left head tilt or right head tilt.
- If worse in right tilt, the right eye intorters (superior oblique and superior rectus) or left eye extorters (inferior oblique and inferior rectus) are affected
- If worse in left tilt, the left eye intorters (superior oblique and superior rectus) or right eye extorters (inferior oblique and inferior rectus) are affected
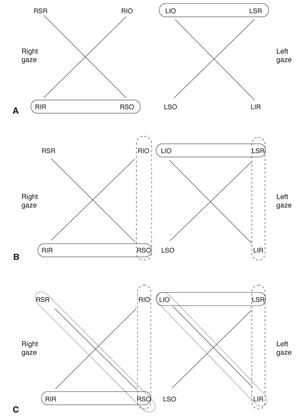
An easy way to isolate the paretic muscle is to draw the field of action for the vertial recti and oblique muscles in each eye. As you go through steps 1-3 above, circle the candidate muscles in each step. The muscle identified as a candidate in all three steps is the paretic muscle, if the deviation is actually due to a muscle paresis. See Figure 2 for an example. Failure to isolate a muscle should raise concern for a skew deviation.
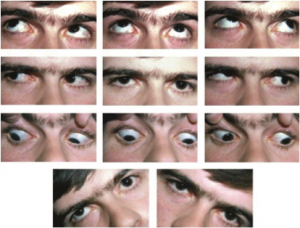
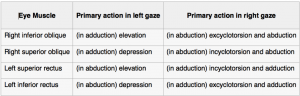
Example Measurements
Step 1. Which eye is hypertropic?
In the patient in Figure 1, the right eye is hypertropic (RHT). When trying to isolate which muscle is paretic in a right hypertropia, it must be either one of the depressors of the right eye or one of the elevators of the left eye. Therefore, we have deduced from step one that the paretic muscle must be one of the following cyclovertical muscles:
- Right superior oblique
- Right inferior rectus
- Left inferior oblique
- Left superior rectus
Step 2. Does the hypertropia increase in right gaze or left gaze?
In this patient, the hypertropia increases in left gaze. Understanding the field of action of each cyclovertical muscle is critical for further deduction of which muscle could be paretic in step two. The field of action of an extraocular muscle is the direction in which the muscle’s primary action is the greatest. In each of the cardinal positions of gaze, there is always one muscle in each eye which is the prime mover. When measuring a deviation in side gazes for step two of the three-step test, the examiner is attempting to isolate specific muscles which are the prime movers in those gazes.
In this example patient, the right hypertropia increases in left gaze. Therefore, the paretic muscle must be either (1) one of the muscles whose primary action is elevating the left eye on left gaze, or (2) one of the muscles whose primary action is depressing the right eye in left gaze.
The right inferior oblique and the left superior rectus both have a primary action of elevation in left gaze. Therefore, one of these muscles could be the paretic muscle. Likewise, the right superior oblique and the left inferior rectus have a primary action of depression in left gaze and could be paretic.
Because the right inferior oblique and the left inferior rectus did not meet Step 1, they can be eliminated from the list of possible paretic muscles. This leaves the right superior oblique and the left superior rectus as the two cyclovertical muscles left which meet criteria for both steps 1 and 2.
Step 3. Does the hypertropia increase in right head tilt or left head tilt?
Step three is the final step in determining which of the two remaining muscles is paretic. In this example, the right hypertropia is worse in left gaze.
If the deviation increases on right head tilt and decreases on left head tilt, as it does in this example patient, then the right superior oblique is implicated as the paretic culprit. The reason for this is because the right superior oblique and right superior rectus muscles work together to incyclotort the right eye in right head tilt. Usually they offset each other in terms of vertical movement, because the superior oblique depresses and the superior rectus elevates. However, in the case of the paretic right superior oblique, the elevating action of the right superior rectus is unopposed and causes an increase in the right hypertropia when the patient tilts his or her head to the right. The deviation is decreased or absent when the head is tilted towards the unaffected eye (the left side in this example) because the superior oblique muscle is not stimulated in the affected eye, but it is stimulated in the unaffected eye.[7]
During head tilt to the right, the otolith system sends impulses to the extraocular muscles that assist in torsion, because the eyes need to adjust to the right head tilting by a compensatory rotation to the left around the anteroposterior (Y) axis. On right head tilt, the left eye excyclotorts due to the actions of the left inferior oblique and the left inferior rectus. Likewise, the right eye incyclotorts due to the actions of the right superior oblique and the right superior rectus.[8]
Since the right superior oblique is paretic and unable to counteract the elevation and adduction actions of the right superior rectus in the right head tilt, the right eye moves upward.
Upon head tilt to the left side, the right hypertropia in this example decreases significantly. In some patients, the right hypertropia may be completely eliminated in left head tilt. When the head is tilted to the left, the cyclorotation of both eyes to the right (incyclotorsion of the left eye and excyclotorsion of the right eye) do not require the right superior oblique. Therefore, this example of a right hypertropia which increases in left gaze and right head tilt is a positive three-step test for a right superior oblique palsy.[9]
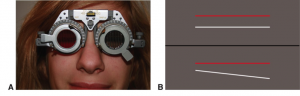
Step 4. Double maddox rod
A fourth step can be added to 3-step test to quantitate the torsional component of trochlear nerve palsy by using the subjective Red-Glass or Double Maddox rod. The Maddox rod is a lens with serial prisms aligned evenly to convert a point of light into a line 90 degrees away from the meridian of the prims. In a double maddox rod test, two lenses of different color are used.
In a patient with no devation, if the prisms are placed vertically, the patient will see a horizontal line. A patient with hypertropia will see a line below the source of light. If the eye is excyclotorted, the patient will see a slanted line with the lower end towards the excyclotorsion.
The examiner or patient then turns the knob of the Maddox lens until the two lines are parallel. The magnitude of cyclotropia and the direction of deviation is measured by the displacement of the scratch mark on the Maddox rod from the 90-degree mark on the trial frame. More than 10 degree of excyclotorsion suggests bilateral trochlear nerve palsies.[9]
One of the pitfalls of the Red-glass and Double Maddox Rod tests is that they are subjective and results are variable according to the examiner. To address the challenges of issuing these tests at the bedside, researchers have developed a computerized red glass test for quantifying and localizing diplopia.[10]
Step 5. Upright-supine test
Wong et al recommended adding a fifth step to the 3- step test called upright-supine test.[11] This test is used to differentiate skew deviation, a vertical misalignment with or without head tilt or fundus torsion of supranuclear origin (brainstem or cerebellum) from other causes of vertical strabismus. In this study, participants fixated on a single-letter opto-type in 12-point font that was located meters away in the mid-saggital plane at eye level. Prisms with increased power were then placed over the deviated eye and the cover was placed over each eye in an alternating fashion. The highest prism strength with no refixation movement was recorded in prism diopters. This test was then repeated for each participant in the supine position. A positive upright-supine test result was defined as a 50% or greater decrease in the vertical deviation measured from the upright to supine position. There was no significant difference between the upright and supine positions for patients with trochlear nerve palsies, restrictive strabismus, or other causes of vertical strabismus. There was a statistically significant decrease for patients with skew deviation. This step can be added after the 3 step test and after the fourth step described above in order to differentiate between skew deviation and other causes of vertical strabismus.[11]
Sensitivity of the Three Step Test
While the Parks 3 step test is the standard for diagnosis of a cyclovertical muscle palsy, recent studies have questioned the sensitivity of this test in identifying which muscle is paretic. One study sought to analyze the sensitivity of the 3 step test in identifying a superior oblique palsy by analyzing 50 patients with confirmed evidence of superior oblique atrophy on MRI. The study found that the test failed to detect 30 percent of cases of superior oblique palsy.[12] In their study, often only 2 of the 3 steps were positive. A different study analyzed the sensitivity of the test in identifying a superior oblique palsy based on the presence or absence of the trochlear nerve confirmed by MRI. Because the absence of the trochlear nerve confirms a superior oblique palsy, the sensitivity of the test should be evaluated according to those parameters. Of the 166 patients studied, results found that the three step test had a sensitivity of 75% in diagnosing unilateral superior oblique palsy regardless of the presence of the trochlear nerve.[13]
Another study found that a positive three step test does not necessarily mean that the patient has a cyclovertical muscle palsy. Many other causes of vertical strabismus can result in a positive three step test, including contracture of the vertical recti, paresis of more than one vertical muscle, dissociated vertical divergence, previous vertical muscle surgery, skew deviation, myasthenia gravis, and small nonparalytic vertical deviations associated with horizontal strabismus.[14] While the three step test remains the gold standard, given the broad differential for vertical strabismus, further imaging may be required to identify a cyclovertical muscle palsy.[12]
References
- ↑ Tollefson MM, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood hypertropia: a population-based study. Ophthalmology. 2006;113:1142.
- ↑ 2.0 2.1 2.2 Yeung, Pauline HN; Lam, Andrew KC (10 September 1998). "Fourth nerve palsy with monovision". Clinical and Experimental Optometry. 81 (5): 206–209. doi:10.1111/j.1444-0938.1998.tb06737.x
- ↑ Younge BR, Sutula F. Analysis of trochlear nerve palsies. Diagnosis, etiology, and treatment. Mayo Clin Proc. 1977; 52(1):11-18. PMID: 609280
- ↑ Bielschowsky, A: Lecture on motor anomalies of the eyes: II. Paralysis of individual eye muscles. Arch. Ophthal. (Chicago) 1935, 13:33-59.
- ↑ Bielschowsky, A: Disturbances of the vertical motor muscles of the eye. Arch. Ophthal. (Chicago) 1938. 20: 175-200.
- ↑ "Head Tilt Test." Head Tilt Test. Orbis Telemedicine, 2014. Web. 08 May 2015. <http://telemedicine.orbis.org/bins/content_page.asp?cid=735-2858-4397-2804-3110-3021-3037>.
- ↑ Simonsz HJ, Crone RA. Bielschowsky head-tilt test––I. Ocular counterrolling and Bielschowsky head-tilt test in 23 cases of superior oblique palsy. Vision Res. 1985;25(12):1977-82.
- ↑ Pansell T, Ygge J, Schworm HD. Conjugacy of Torsional Eye Movements in Response to a Head Tilt Paradigm. Investigative Ophthalmology & Visual Science. 2003;44:2557.
- ↑ 9.0 9.1 Spector RH. Vertical diplopia. Survey of Ophthalmology. UNITED STATES: Elsevier Inc; 1993;38:31-62.
- ↑ Yoo HS, Park E, Rhiu S, et al. A computerized red glass test for quantifying diplopia. BMC Ophthalmology. 2017;17:71. doi:10.1186/s12886-017-0465-8.
- ↑ 11.0 11.1 Wong AM, Colpa L, Chandrakumar M. Ability of an upright-supine test to differentiate skew deviation from other vertical strabismus causes. Arch Ophthalmol. 2011 Dec;129(12):1570-5.
- ↑ 12.0 12.1 Manchandia AM, Demer JL. Sensitivity of the three-step test in diagnosis of superior oblique palsy. Journal of AAPOS. 2014;18(6):567-571. doi:10.1016/j.jaapos.2014.08.007.
- ↑ Lee JE, Yang HK, Kim JH, Hwang JM. Diagnostic Utility of the Three-Step Test According to the Presence of the Trochlear Nerve in Superior Oblique Palsy. J Clin Neurol. 2018 Jan;14(1):66 -72.
- ↑ Kushner BJ. Errors in the three-step test in the diagnosis of vertical strabismus. Ophthalmology. 1989;96:127-132.