Cicatricial Ectropion
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
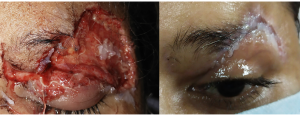
Cicatricial ectropion occurs due to the shortening of the anterior lamella, which comprises of skin and orbicularis. Scarring or shortening of the anterior lamella causes outward rotation of the lid margin.
Etiology
There are various causes of anterior lamellar shortening leading to cicatricial ectropion, some of the important causes of cicatricial ectropion include mechanical, chemical or thermal injury, skin diseases, and excessive skin removal during lower lid blepharoplasty. Tissue thinness and the critical position of structures such as the puncta, canalicular system, and tarsi make even minimal displacement of the lower eyelid border symptomatic. Exposure keratitis with reflex tearing secondary to lagophthalmos and failure of the lacrimal pump mechanism are responsible for symptoms of ocular surface dryness such as grittiness, epiphora, redness and diminution of vision. The common causes of cicatricial ectropion include
- Trauma
- Burns
- Cicatrizing skin tumors
- Medications like dorzolamide, brimonidine[1]
- Allergies
- Skin conditions – ichthyosis
To effectively manage cicatricial ectropion, it is important to have a proper understanding of various phases of wound healing and types of scar.
Pathology
Phases of wound healing
Inflammatory phase: Whenever there is trauma, the inflammatory phase begins which lasts for 4-6 days. The inflammatory phase is characterized by the presence of local edema, erythema, and pain.
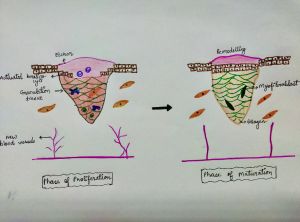
Proliferative phase: The proliferative phase lasts for 4-24 days. The smaller blood vessels begin to proliferate, and granulation tissue fills the wound. Fibroblast lay collagen in the wound bed, causing the granulation tissue to strengthen, and wound edges begin to contract.
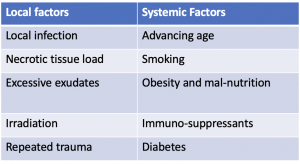
Maturation phase: The maturation phase lasts for 21 days to 2years. Filled in the wound is strengthened and scar tissue is formed. The length of the maturation phase varies. The factors affecting the wound maturation have been summarized in table1
Patho-physiology
The scar is formed as a consequence of wound healing in which the normal skin is replaced by fibrous tissue. An ideal scar is thin and flat, has a color matching with the surrounding skin, and is oriented along the relaxed skin tension lines. An ideal scar does not produce any distortion of the adjacent tissues. A mature scar is flat, light-colored, and does not undergo any further changes in morphology. On the contrary, an immature scar is raised, erythematous, rigid, and painful. An immature scar though eventually matures they are always at a risk of developing a hypertrophic scar.
Hypertrophic Scar vs Keloid
A hypertrophic scar occurs soon after trauma, improves with time, and remains confined to the wound margins. The hypertrophic scar worsens after surgery and consists of thick collagen with the mucoid matrix. Keloid, on the other hand, occurs months after trauma, does not improve with time. The term keloid means “claw-like” due to its appearance and extends beyond the wound margin. Keloids consist of a few thick collagen with the scanty mucoid matrix.
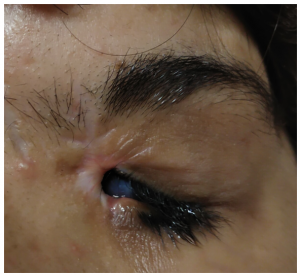
Clinical features
The patients usually present with symptoms of epiphora, redness, tearing, and foreign body. Sensation occurring secondary to exposure to the ocular surface and an inadequate tear film. In extreme cases, the cornea can develop punctate epithelial erosions, ulceration, and permanent vision loss. These can be explained due to inadequate opposition of the lid with the globe.
Clinical evaluation
The complete ocular examination must be performed to plan for further surgical management, this includes: The extent of scar, and appearance of scar: The scar color, texture and thickness, and scar maturity must be examined.
Lid position examination
Grading of cicatricial ectropion
- Grade I- Punctal eversion or a part of posterior lid margin not apposed to the globe.
- Grade II- Whole length of the posterior lid margin not apposed to the globe
- Grade III- Palpebral conjunctiva visible.
- Grade IV- Fornix is visible
Besides this, one should measure, the horizontal and vertical height of palpebral fissure, lagophthalmos, and amount of lid retraction. A complete anterior segment examination must be done to look for ocular surface, corneal opacity, and corneal vascularization, as lagophthalmos can lead to poor ocular surface and exposure keratopathy. Tear film break up time and Schirmer’s test helps to evaluate the ocular surface.
Primary prevention
The time taken by scar to mature and regain 70-80 % tensile strength is 6 –12 months.[2] Adjunct treatments during this period help in scar maturation and prevents the formation of hypertrophic scar. Immature scars are prone to hypertrophy and give poor results after scar revision. If used in the early post-traumatic period, certain agents may minimize ugly scar formation and cosmetically acceptable outcomes in the long run. These adjunct treatments include scar massage, silicone gel, intra-lesional injection of steroids, and antimetabolites.
Non-Surgical Management of periocular scars
Scar massage
Scar massage hastens wound healing, decreases itching, redness, and pain associated with an immature scar, and shortens the time required for scar maturation. Massage causes mechanical disruption of fibroblast fibers, increasing the pliability of the wound, leading to a softer scar. Scar massage should be started as soon as possible and should be continued 2–3 times a day till 6–8 weeks after the trauma or surgery. [3]
Pressure therapy
Pressure therapy is the standard of care for burn scars worldwide. Compression of the scar is believed to aggravate the hypoxic condition of the scar tissue. Thus, increasing degeneration of fibroblasts and collagen as well as a decrease in the collagen synthesis.[4]
Silicone gel
Silicone gel provides a hydrating environment for the epidermal layer, decreases capillary activity, vascularity, and the metabolism of the scar tissue, resulting in reduced collagen deposition.[5] Silicone gel can be applied in the form of silicone gel sheets or in the form of topical silicone gel. In a study performed by Kim et on 30 patients, similar results were observed by using silicone gel topical application as well as by silicone gel sheet application.[6]
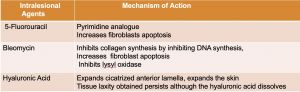
Intra-lesional steroids
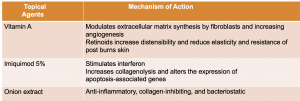
Intra-lesional steroid injections inhibit keratinocyte proliferation, inflammatory compounds and have an anti-angiogenic effect. The dose and regimens vary between 1 to 40 mg/ml at 2–6 weeks’ intervals.[7] The success rate is 40% and 100% for keloids.[8] Whereas, the recurrence rates vary between 9% and 50%.[9] [10] Other agents used for intra-lesional (table 2) and topical application have been summarized in table 3.
Role of Hyaluronic acid (HA) fillers
HA injections act as temporary volumizers and are only a short-term treatment option for eyelid ectropion. Mechanical stretching caused by HA injections is believed to induce fibroblasts to produce new collagen. HA injections correct the eyelid ectropion by dually lifting the eyelid back into a neutral position and by mechanically expanding the lid tissue to promote neo-collagen genesis. 0.2 ml injection of HA subcutaneously followed by an additional 0.3ml injection of HA has been reported as an option in the management of cicatricial ectropion.[11]
Non-ablative laser resurfacing
Non-ablative fractional laser resurfacing is performed with a fractional non-ablative laser, consisting of an active erbium glass rod attached to a xenon flash, emitting at a wavelength of 1540 nm. The patient is made to wear protective metal eye shields before starting the procedure. The non-ablative laser has a unique thermal pattern with columns of thermal damage at specific depths and its effect stimulates a therapeutic wound healing response with heat shock proteins, myofibroblasts, and an increased collagen III production and thereby, raises the potential for texture re-modelling.[12]
Autologous Fat graft for Cicatricial Ectropion
In the recent times with the increasing use of less invasive techniques for fat harvesting like lip-suction, the autologous fat grafts for the correction of scars and cicatricial ectropion is being considered as a promising and less expensive alternative to the fillers. Adipose tissue contains the stored fat and a reserve of mesenchymal stem cells, that can multiply indefinitely, because of this property they are able to replace cells that have been atrophied, stem cells also offer the hope for restoration of full mechanical and biological properties.[13] The autologous adipose tissue is processed and harvested according to S.R.Coleman's technique. The technique has been widely used for first and second degree burn scars.
Surgical management
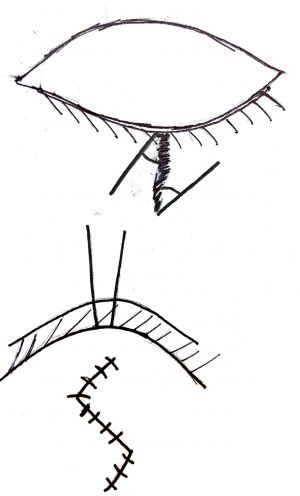
Z plasty
Z plasty transposes the triangles and redistributes the tension on the wound by changing the direction of the central limb.
Geometric principle of Z plasty: A central axis of the Z will rotate 90°.75% increase in length occurs along the line of the central limb and a decrease in length in the perpendicular direction, as a result, the linear scar becomes nonlinear.
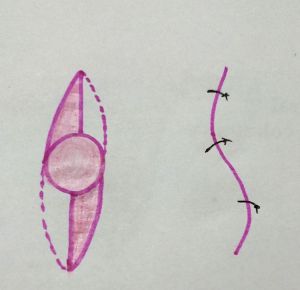
S plasty
S plasty is indicated in oval contracted scars, and a large triangular flap transposition is performed. The rounding of flap ends promotes better survival.
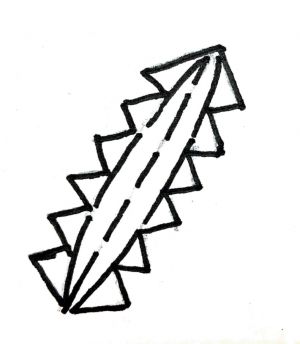
W plasty
The principle of W plasty is to reduce the visibility of scar as the visibility of an irregular broken line is less due to insignificant light reflection . Difficult for the eyes to follow as compared to a straight scar. Series of consecutive triangles are made on one side of the scar with its mirror image on the other side.
Skin graft
History
The word plastic surgery takes its origin from the Greek word plastin, which means to be able to mold. Plastic surgery is a branch of general surgery which is reconstructive and aims to repair the defects or malformations with the restoration of function and improvement in appearance. Skin grafting is a commonly performed procedure in reconstructive oculoplastic surgery. In simple terms, skin graft means reconstructing a skin defect by placing the skin from anywhere in the body. The history of skin graft dates back to 2500-3000 years back when the grafts were initially used to cover the defects caused by the nose amputation. The ancient Indian method included the subcutaneous fat also, along with the skin graft, taken from the gluteal region. The significant development in skin grafting procedures took place in the 19th century. Reverdin introduced the concept of pinch graft, which hastened the healing of granulated wounds by small bits of transplanted skin. Thiersch introduced a split-thickness graft, wherein an epidermis sheet was used to cover the defect. Wolfe later used a full-thickness graft to cover a lower lid defect. [14]
Anatomy of Skin
The skin of the eyelid is essential for cosmesis as well as for functional causes. The skin of the eyelid is different as it lacks appendages, and is thin.
Epidermis
The epidermis is a thin, semi-transparent layer that provides a significant barrier function. The epidermis also includes melanocytes, Langerhans cells, Merkel cells, and nerve endings. Skin adnexal structures, including hair follicles, sweat glands, and sebaceous glands, are epidermal derivatives that invaginate into the dermis.
Dermis
The depth of dermis, amount of elastin, and presence of appendages vary in different areas of the body. Therefore, making the fine, elastic skin of the eyelid more vulnerable to injury. Skin vascularity is derived from a run through underlying muscles or fascial septal layers. If a skin graft is not done, the wound healing occurs by secondary intention with contracture and fibrosis.
Types of skin graft
Split thickness skin graft
Split thickness skin grafts are also known as Thiersch grafts, and can be used to cover wounds of all sizes. The split-thickness skin graft is composed of epidermis and partial thickness of the dermis. It can be thin (0.005-0.012 inch), medium (0.012-0.018 inch), or thick (0.018-0.030 inch) split-thickness skin graft.
Full-thickness graft
Full-thickness skin grafts are commonly used in reconstructive procedures of the eyelid and periorbital scars and deformities. Full-thickness grafts incorporate full-thickness epidermis, dermis, and also fat. The fat is trimmed unless planned for a composite graft. Advantages of full-thickness skin graft over split-thickness graft are that the former resembles normal skin in color, thickness, and texture and has a lesser secondary contraction. Disadvantages over split-thickness graft are more primary contraction, donor site morbidity, limited donor tissue, and poorer survival especially over ischemic or avascular beds such as extensive acute burns, bone, etc.
Indications of eyelid skin graft
Full-thickness skin graft
- Anterior lamellar reconstruction in reconstructive procedures for congenital coloboma, post-traumatic or post-surgical coloboma, etc.
- Scar revision surgery in the eyelid or periorbital area.
- Cicatricial ectropion, cicatricial retraction
Split thickness skin graft
- Reconstruction of the exenterated socket.
- Reconstruction of repeatedly failed anophthalmic contracted socket
- Extensive burn patients
Surgical procedure for harvesting full-thickness graft
Donor site
The ideal donor site for full-thickness skin grafting in the eyelid is ipsilateral or contralateral eyelid skin. Removal of skin from a normal eyelid is generally associated with functional and/ or cosmetic deformity of the donor's eyelid, especially in younger patients so is not preferred. Moreover, the amount of skin that can be harvested is limited (~ 1.5cm wide and 4 cm long in older patients). Common donor sites for full-thickness skin grafting procedures are the post-auricular area (cephaloauricular area), the inner side of the upper arm, the lower abdomen, and the inner side of the thigh. The choice of donor site should be such that the donor site scar is hidden. As eyelid skin lacks hair follicles, the graft is usually harvested from the retro-auricular skin, supraclavicular area, abdomen, and inner aspect of the upper limb. The choice of donor site also depends on the patent’s age, size of graft required, and presence of any scars on the donor site. Therefore, post-auricular skin is the second-best and most popular donor site as is similar in thickness, color with minimal hair so resembles eyelid skin, easily accessible with a hidden scar.
Disadvantages are harvesting of a large graft can pull the ear close to the skull. The common donor site for split-thickness skin graft is the upper thigh and lower abdominal wall.
Surgical procedure for harvesting full-thickness skin graft:
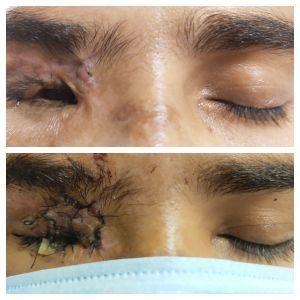
a. The recipient bed is prepared after the removal of scar tissues. The size of the defect at the recipient site is measured by placing a sterile piece of paper over the defect and outlining using a marker pen. The piece of paper is then cut along the markings of the pen. Alternatively, maximum and minimum dimensions can be measured, the graft is usually spindle-shaped.
b. The paper is placed over the donor site and the size is marked using a marker pen. The donor site is anaesthetized by injecting 2% lidocaine with adrenaline in the subcutaneous plane. An incision is made over the skin using a no. 15 scalpel blade,1-2mm away from the markings (slightly over-sized graft to take care of primary contraction except eyelid skin graft which is kept the same size as recipient defect) and the graft is removed using blunt forceps and Wescott scissors. The depth of the dissection should be subcutaneous avoiding taking fat in it. The graft is kept moist in a bowl of saline.
c. The donor site is closed using 6-0 polyglactin sutures for subcutaneous tissue closure, to reduce the dead space (to avoid hematoma or fluid accumulation), and 4-0 silk sutures for skin closure. Undermining of skin edges helps enclosure.
d. The harvested skin graft should de-fatted using scissors for better take. Thicker the graft more will be the chances of necrosis.
e. The graft should be placed over the recipient bed and sutured using 6-0 silk sutures or fibrin glue.[14] [15]
f. To increase the chances of taking of the graft, it should be sutured to the bed using 2-3 quilting 6-0 silk sutures. Few stab incisions should be put in the graft to allow drainage of fluids and to prevent hematoma formation. A rolled piece of sterile gauze with ointment is placed over the graft to stabilize the graft and prevent fluid/ blood accumulation beneath the graft. Suture tarsorrhaphy helps in stabilizing the eyelid.
g. A pressure bandage is done, that is opened after 48-72 hours. The bandage should be gently removed after soaking it with saline. Suture removal is usually done 5 – 7days after surgery. The topical antibiotic ointment helps in keeping the graft moist. Alternate sutures can be removed first if healing is doubtful. Tarsorrhaphy can be removed in 2 weeks.
Steps of graft take
Phase of Imbibition
The skin graft passively absorbs oxygen and nutrients from the recipient bed by diffusion from plasma. The graft is pale or white during this period. This phase usually lasts for the first 48 hours. Thereafter, the color of the graft begins to change from white to a blotchy blue and then, slowly to a healthy pink color in patches during the inoculation and revascularization phase.[16]
Phase of inosculation
After 48 hours the fine anastomotic capillary connections are made, leading to the phase of inosculation. The capillary ingrowth, aids in the healing process by promoting fibroblast maturation. The graft is usually pink in this phase.
Phase of Re-vascularisation
The exact mechanism of re-vascularisation is not known and several hypotheses exist for re-vascularisation. The neovascularisation theory suggests new vessel ingrowth into the graft from the recipient wound bed. The exact mechanism of re-vascularisation is not known and several hypotheses exist for re-vascularisation. The neovascularisation theory suggests new vessel ingrowth into the graft from the recipient wound bed.
Complications of skin graft
Primary contracture
Primary contracture is the immediate reduction in the size of a skin graft after it has been harvested, caused by passive recoil of elastin fibers in the dermis. As Full-thickness skin grafts have a greater amount of dermis, primary contracture is more significant in full-thickness skin graft than a split-thickness skin graft.
Secondary contracture
Secondary graft contracture is the shrinkage of graft which occurs with time over the wound bed and is caused by the myo-fibroblast. Secondary graft contracture is more commonly seen with split-thickness skin grafts.
Donor site morbidity
Donor site wound dehiscence is the usual complications seen when large grafts are harvested, hence in the post-operative period it is essential to regularly examine the donor site.
Graft failure and graft necrosis
The graft in its initial stages retrieves its nutrition from the donor site by the process of imbibition, however, if the graft is separated from the wound bed due to accumulation of fluid, hematoma, seroma, and exudates there is an increased risk of graft failure. The collections of fluid beneath the graft can be avoided by placing the stab incisions on the graft. Similarly, the opposition of the graft with the wound bed can be assured by placing the anchoring sutures. Graft infection increases the oxidative stress on the graft as well as disrupts the wound bed with abscess formation. Porcelain white graft or overlying black eschar is seen 1-2 weeks after grafting suggests impending graft failure. Failed grafts can act as dressings over the wound which can later heal by secondary intention.
References
- ↑ Hegde V, Robinson R, Dean F, Mulvihill HA, Ahluwalia H. Drug-induced ectropion: what is best practice? Ophthalmology. 2007 Feb;114(2):362-6.
- ↑ Ireton JE, Unger JG, Rohrich RJ. The role of wound healing and its everyday application in plastic surgery: a practical perspective and systematic review. Plast Reconstr Surg Glob Open. 2013;1(1):e10-e19.
- ↑ Ault P, Plaza A, Paratz J. Scar massage for hypertrophic burns scarring-A systematic review. Burns. 2018 Feb;44(1):24-38. doi: 10.1016/j.burns.2017.05.006. Epub 2017 Jun 29.
- ↑ Zhang, Hao MBa,∗; Wang, Hao-yan MMb; Wang, Da-li MBc; Zhang, Xiao-dong MBa Effect of pressure therapy for treatment of hypertrophic scar, Medicine: June 2019 - Volume 98 - Issue 26 - p e16263 doi: 10.1097/MD.0000000000016263
- ↑ O'Brien L, Jones DJ. Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst Rev. 2013;2013(9):CD003826. Published 2013 Sep 12. doi:10.1002/14651858.CD003826.
- ↑ Kim SM, Choi JS, Lee JH, Kim YJ, Jun YJ. Prevention of postsurgical scars: comparsion of efficacy and convenience between silicone gel sheet and topical silicone gel. J Korean Med Sci. 2014;29 Suppl 3(Suppl 3):S249-S253. doi:10.3346/jkms.2014.29.S3.S249
- ↑ Srivastava S, Patil AN, Prakash C, Kumari H. Comparison of Intralesional Triamcinolone Acetonide, 5-Fluorouracil, and Their Combination for the Treatment of Keloids. Adv Wound Care (New Rochelle). 2017;6(11):393-400. doi:10.1089/wound.2017.0741
- ↑ Trisliana Perdanasari A, Lazzeri D, Su W, et al. Recent developments in the use of intralesional injections keloid treatment. Arch Plast Surg. 2014;41(6):620-629. doi:10.5999/aps.2014.41.6.620
- ↑ Niessen FB, Spauwen PH, Schalkwijk J, et al. On the nature of hypertrophic scars and keloids: a review. Plast Reconstr Surg. 1999;104:1435–1458. [PubMed] [Google Scholar]
- ↑ Morelli Coppola M, Salzillo R, Segreto F, Persichetti P. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387-396. Published 2018 Jul 24. doi:10.2147/CCID.S133672
- ↑ Longinotti C. The use of hyaluronic acid based dressings to treat burns: A review. Burns Trauma. 2014;2(4):162-168. Published 2014 Oct 25. doi:10.4103/2321-3868.142398
- ↑ Verhaeghe E, Ongenae K, Bostoen J, Lambert J. Nonablative fractional laser resurfacing for the treatment of hypertrophic scars: a randomized controlled trial. Dermatol Surg. 2013 Mar;39(3 Pt 1):426-34. doi: 10.1111/dsu.12059. Epub 2012 Dec 26. PMID: 23279702.
- ↑ Caviggioli F, Klinger F, Villani F, Fossati C, Vinci V, Klinger M. Correction of cicatricial ectropion by autologous fat graft. Aesthetic Plast Surg. 2008 May;32(3):555-7. doi: 10.1007/s00266-008-9117-y. PMID: 18293030.
- ↑ 14.0 14.1 Davis JS. ADDRESS OF THE PRESIDENT: THE STORY OF PLASTIC SURGERY. Ann Surg. 1941 May;113(5):641-56. doi: 10.1097/00000658-194105000-00001. PMID: 17857763; PMCID: PMC1385923.
- ↑ Paw E, Vangaveti V, Zonta M, Heal C, Gunnarsson R. Effectiveness of fibrin glue in skin graft survival: A systematic review and meta-analysis. Ann Med Surg (Lond). 2020 Jun 12;56:48-55.
- ↑ Fox SA. Ophthalmic Plastic Surgery. Fourth Edition, Grune & Stratton, Inc. 1970.