Wolfring Gland Ductal Cyst
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Wolfring gland ductal cysts (WGDCs) are benign cystic lesions of the eyelid. They are not uncommon in countries where trachoma has been endemic. WGDC represents a clinical diagnostic challenge with a high possibility of misdiagnosis. Certain clinical and histologic clues help guide the diagnosis. Complete surgical excision with intact wall remains the recommended treatment modality.
Disease Entity
Disease
Wolfring gland ductal cyst (WGDC) refers to cystic dilatation of the duct of the accessory lacrimal glands of Wolfring[1]. Wolfring glands are located in the deep conjunctival stroma along the proximal tarsal border in the upper eyelid, and to a lesser extent in the lower eyelid. WGDC is also known as Wolfring dacryops[1], ductal cyst of the accessory lacrimal gland of Wolfring, Wolfring ductal cysts, and accessory lacrimal gland ductal cyst. WGDC usually affects young adults or middle-aged individuals.[2]
Etiology
The exact etiology remains unclear.
Risk Factors
WGDC has been reported to be linked with conditions causing chronic conjunctival inflammation and cicatrization. Most reported case series come from Saudi Arabia and Egypt, showing a significant association with trachomatous scarring (100% in Weatherhead's series and 79.2% in Diab's series).[1][2] This association might explain why WGDCs are relatively rare in Western countries.
General Pathology
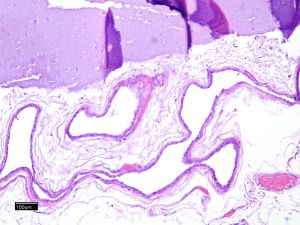
Grossly, WGDC appears smooth, thin walled with telangiectatic blood vessels on the surface, and often contains clear fluid. Histologically, it is lined by a double-layered nonkeratinizing epithelium with occasional inflammatory and goblet cells, and commonly having a serpinginous cavity.[3] Lacrimal glandular acini are typically absent.[1][2] This can be attributed to the limited amount of glandular tissue in accessory lacrimal gland lesions compared to main lacrimal gland lesions that can be overlooked without meticulous tissue sampling and sectioning or due to the careful surgical separation of the cyst from surrounding tissues, including lacrimal glandular tissue.
Pathophysiology
The pathogenesis of WGDC is still debatable and likely multifactorial. Conjunctival cicatrization appears to play a significant role in the formation of dacryops. However, the original hypothesis of cicatricial ductular blockage with secondary build up of secretory pressure, as the sole mechanism of dacryops formation has been challenged experimentally.[4] Some authors suggest that there is a concurrent IgA hypersecretion into the cyst by activated plasma cells, leading to an osmotic effect.[1][5] Others have proposed dysfunction of the periductular neural plexus.[3]
Diagnosis
WGDC can be diagnostically challenging with a high possibility of misdiagnosis due to its different presentations and similarities with other cystic lesions.[6] Diagnosis is typically made on clinical basis alone. Histopathological examination helps differentiate WGDC from other cystic conditions.[3]
History
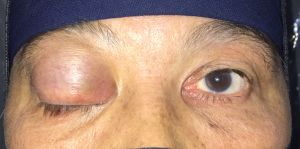
Patients are usually presenting with slowly progressive painless eyelid mass.[2] Small lesions are often asymptomatic.[7]
Physical examination
Exam reveals an immobile bluish grey translucent subconjunctival cyst associated with the proximal tarsal border.[1][2] [7][8]A dense fibrotic band along the proximal tarsal border is typically seen in the area of the cyst on complete lid eversion.[2] These lesions more frequently appear in the upper eyelid medially or centromedially, likely because more Wolfring glands exist in this location. The cyst tends to grow insidiously; however, a rapid increase in size may occur and should raise the suspicion of cyst complications such as hemorrhage or infection.[2] Signs of chronic trachoma or other cicatrizing conjunctival diseases may be present.[1]
Signs
- Eyelid mass
- Subconjunctival cyst
- Conjunctival scarring
- Transverse fibrotic band along the proximal tarsal border
- Mechanical ptosis, globe dystopia
Symptoms
- Painless eyelid swelling
- Droopy eyelid
- Chronic eye irritation
Diagnostic clues
Certain clinical and histologic clues help differentiate WGDCs from other similar conditions.[1][2]
- Subconjunctival location in the central or centromedial fornix.
- Attachment to the nonmarginal border of the tarsus.
- Transverse fibrotic band along the tarsal border in the area of the cyst.
- Lack of tenderness.
- The double-layered epithelial lining of the cyst with a serpiginous cavity.
Differential diagnosis
Simple dacryops (palpebral lobe dacryops)- the swelling is mobile and located in the superolateral fornix with a possibility of spontaneous and intermittent disappearance.[9]
Krause gland ductal cysts- anatomically located within the fornices and lack fixation to the tarsal plate.[10]
Periorbital dermoid cysts- painless subcutaneous mass along the suture lines, located in the superotemporal or superonasal orbit in a younger age group, not visible through the conjunctiva, commonly associated with underlying bony changes[11], lined by a keratinizing epithelium with adnexal structures, its cavity is filled with keratin and sebaceous fluid.[12][13]
Subconjunctival cysticercosis- painful, yellowish, nodular subconjunctival mass with surrounding conjunctival injection. Orbital cysticercosis- frequently occurs in relation to extraocular muscles with possibility of ocular motility restriction. The cyst has two-layer lining with a scolex can be identified inside the cyst. B scan ultrasonography, CT scan, and MRI are helpful in confirming the diagnosis.[14]
Intratarsal keratinous cyst- firm, well-circumscribed and non-tender, protrudes visibly under the tarsal conjunctiva with anterior tarsal fixation, and lined by stratified squamous epithelium with an inner eosinophilic undulating cuticle and filled with keratin.[15][16]
Conjunctival inclusion cyst- results from the entrapment of conjunctival epithelial tissue within the substantia propria, there may be a history of trauma or surgery, lack of fixation to the tarsal plate, and lined by multilaminar nonkeratinizing squamous epithelium.[6]
Management
Management options include either observation or surgical intervention, depending on the size of the cyst and the patient's complaints. Small asymptomatic lesions can be safely monitored with serial eye exams.
Surgery
Different treatment modalities, such as excision, simple aspiration, marsupialization, or needling, have been described for WGDCs.
1- Complete surgical removal with an intact wall remains the mainstay treatment and can be performed either through the conjunctiva or skin. A recent retrospective study has shown more favorable outcomes with the transcutaneous approach.[1][2]
2- Simple needle aspiration is generally not recommended as cysts readily refill after the procedure.
3- Marsupialization entails excising a part of the cyst roof through a conjunctival incision and leaving the wound to heal spontaneously. The procedure does not require meticulous dissection of the cyst wall, however the risk of recurrence remains a concern.[17][18]
Complications
Cysts can develop chronic inflammation or infection with abscess formation or fistulization. Patients having infected cysts often present with painful eyelid swelling and redness.[19] The surrounding conjunctiva shows injection and chemosis with the presence of whitish opacification inside the cyst. Infections require management with systemic antibiotics prior to surgical treatment. Bleeding into a cyst can occur and the cyst becomes chocolate colored with rapid increase in size. [2]A large WGDC in a child can induce significant refractive error or cause progressive significant ptosis with a potential risk of amblyopia.[7]
Prognosis
The prognosis is excellent.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Weatherhead RG, Wolfring Dacryops. Ophthalmology. 1992;99(10):1575–81.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Diab MM, Allen RC, Mohammed KK, Saif ATS. Clinical characteristics and surgical outcomes of transcutaneous versus transconjunctival excision of Wolfring gland ductal cysts. BMC Ophthalmol. 2024;24(1):164.
- ↑ 3.0 3.1 3.2 Jakobiec FA, Zakka FR, Perry LP. The cytologic composition of dacryops: an immunohistochemical investigation of 15 lesions compared to the normal lacrimal gland. Am J Ophthalmol. 2013;155(2).
- ↑ Bullock JD, Fleishman JA, Rosset JS. Lacrimal ductal cysts. Ophthalmology. 1986;93(10):1355–60.
- ↑ Lam K, Brownstein S, Jordan DR, Jastrzebski A. Dacryops: a series of 5 cases and a proposed pathogenesis. JAMA Ophthalmol. 2013;131(7):929-932. doi:10.1001/jamaophthalmol.2013.1885
- ↑ 6.0 6.1 Alsarhani WK, Al-Sharif EM, Al-Faky YH, Alkatan HM, Maktabi AM, Alsuhaibani AH. Dacryops and clinical diagnostic challenges. Can J Ophthalmol. 2022;57(6):388–93.
- ↑ 7.0 7.1 7.2 Fung SE, Men CJ, Korn BS, Kikkawa DO, Liu CY. Wolfring dacryops: a case of acquired ptosis in a child. Plast Aesthet Res. 2020;7.
- ↑ Feijó ED, Alencastro Landim G, De Melo Dias M, Alves De Souza BA, Murillo Limongi R, Matayoshi S. Giant bilateral cysts of the Accessory Lacrimal glands of Wolfring in a child. Ophthalmic Plast Reconstr Surg. 2020;36(1):e4–6
- ↑ Ozgonul C, Uysal Y, Ayyildiz O, Kucukevcilioglu M. Clinical features and management of dacryops. Orbit. 2018;37(4):262-265. doi:10.1080/01676830.2017.1423081
- ↑ Alsulaiman HM, Fatani DR, Al Sheikh O, et al. Krause's accessory lacrimal gland dacryops - case report and literature review. Orbit. 2020;39(6):441-445. doi:10.1080/01676830.2019.1704796
- ↑ Sathananthan N, Moseley IF, Rose GE, et al. The frequency and clinical significance of bone involvement in outer canthus dermoid cysts. Br J Ophthalmol 1993;77:789–94.
- ↑ Pushker N, Meel R, Kumar A, Kashyap S, Sen S, Bajaj MS. Orbital and periorbital dermoid/epidermoid cyst: a series of 280 cases and a brief review. Can J Ophthalmol. 2020;55(2):167-171. doi:10.1016/j.jcjo.2019.08.005
- ↑ Diab MM, Allen RC, Abdel Ghafar AE, Elessawy KB. Comparison of three surgical techniques for internal angular dermoid cysts: a randomized controlled trial [published correction appears in Eye (Lond). 2022 Jan 19;:]. Eye (Lond). 2022;36(12):[[1]]. doi:10.1038/s41433-021-01851-0
- ↑ Rath S, Honavar SG, Naik M, et al. Orbital cysticercosis: clinical manifestations, diagnosis, management, and outcome. Ophthalmology. 2010;117(3):600-605.e1. doi:10.1016/j.ophtha.2009.07.030
- ↑ Jakobiec FA, Mehta M, Iwamoto M, Hatton MP, Thakker M, Fay A. Intratarsal keratinous cysts of the Meibomian gland: distinctive clinicopathologic and immunohistochemical features in 6 cases. Am J Ophthalmol. 2010;149(1):82-94. doi:10.1016/j.ajo.2009.07.033
- ↑ AlRubaian A, Alkatan HM, Al-Faky YH, Alsuhaibani AH. Clinical features differentiating intratarsal keratinous cyst from chalazion. Int Ophthalmol. 2020;40(8):2041-2045. doi:10.1007/s10792-020-01380-x
- ↑ Salam A, Barrett AW, Malhotra R, Olver J. Marsupialization for lacrimal ductular cysts (dacryops): a case series. Ophthalmic Plast Reconstr Surg. 2012;28(1):57-62. doi:10.1097/IOP.0b013e31822ddda7
- ↑ Tanaboonyawat S, Idowu OO, Copperman TS, Vagefi MR, Kersten RC. Dacryops - A review. Orbit. 2020;39(2):128-134. doi:10.1080/01676830.2019.1608564
- ↑ Kurup SP, Lissner GS. Characterization of dacryops infections. Ophthalmic Plast Reconstr Surg. 2015;31(1):58-62. doi:10.1097/IOP.0000000000000198