Dermoid Cyst
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Dermoid cyst
ICD10: D31.60
Disease
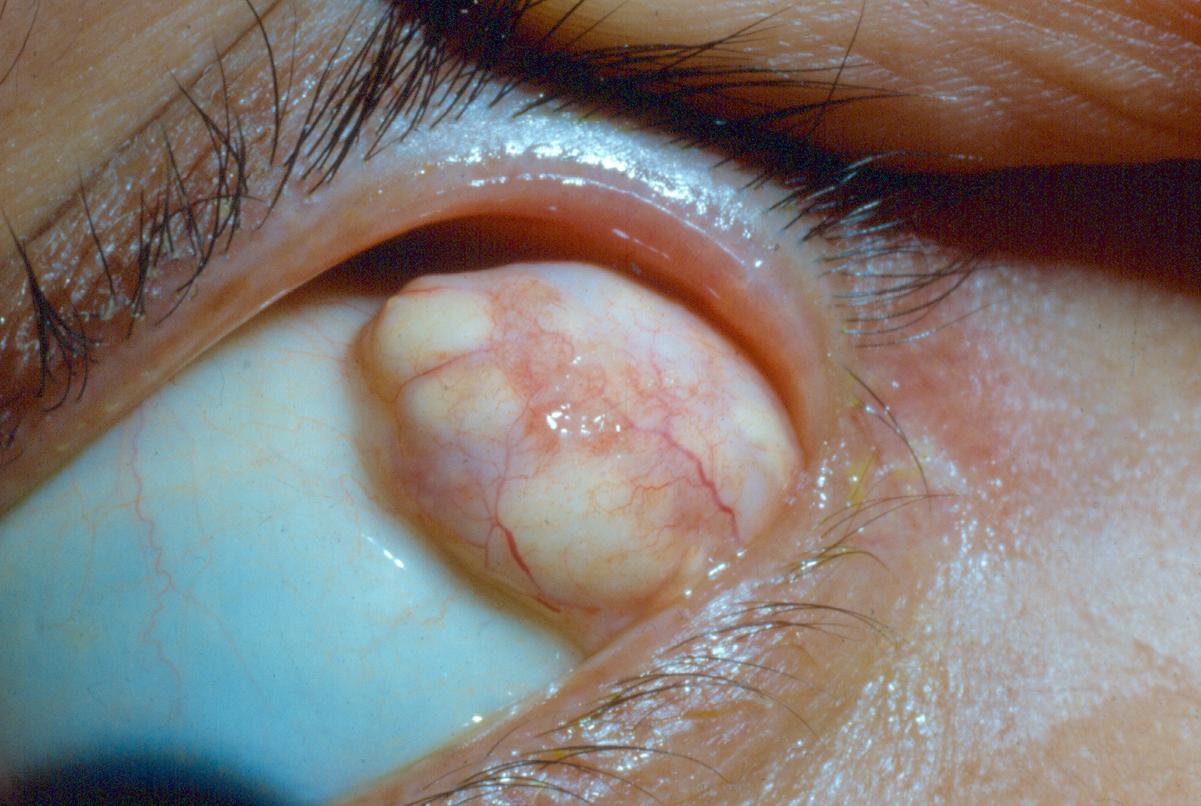
A dermoid cyst is a congenital choristoma of the orbit. A choristoma is a benign tumor consisting of histologically normal cells occurring in an abnormal location. Dermoid cysts consist of keratinized epithelium and adnexal structures such as hair follicles, sweat glands, and sebaceous glands. They slowly enlarge with age. Dermoid cysts are often cited as one of the most common orbital tumors in children, accounting for 46% of childhood orbital neoplasms.[2][3][4] They make up 3-9% of all orbital masses.[5]
Etiology
When fetal suture lines close during embryogenesis, embryonic epithelial nests may become entrapped and form a cyst.[2] The most commonly involved suture is the frontozygomatic suture, although they may also occur at the frontoethmoidal or frontomaxillary sutures.[3][6]
General Pathology
Dermoid cysts are composed of keratinized stratified squamous epithelium with dermal appendages and adnexal structures, including hair follicles, sebaceous glands, sweat glands, smooth muscle, and fibroadipose tissue. The lumen contains keratin and hair.[3][6] Cysts that are only lined with epithelium without adnexal elements are termed epidermoid cysts.[2][4]
Diagnosis
Superficial dermoide are easily diagnosed clinically due to characteristic location at the suture lines and firm consistency. Imaging modalities may also assist in some cases. More details are presented below.
History
Patients with superficial dermoids are usually children presenting with a slowly progressive, nontender mass near the lateral eyebrow.[7]
Older children and adults may present with diplopia or proptosis.[4]
Physical Examination
A superficial cyst usually presents as a smooth, painless mass in the superotemporal quadrant, but it may also be found in the superonasal quadrant. It may appear mobile or affixed to bone. If the cyst leaks or ruptures with extrusion of oil and keratin into adjacent tissues, granulomatous inflammation may be present.[2] They are more common than deep cysts and usually become apparently during the first decade of life. If large, they may cause mechanical ptosis.[5]
Deeper orbital cysts may be partially palpable or non-palpable. They are usually diagnosed in older children or adults.[3] Deep cysts may cause progressive proptosis, strabismus or diplopia.[4]
Signs
- Palpable mass
- Ptosis
- Proptosis
- Strabismus
- Pulsating proptosis with mastication[7]
- Globe displacement[5]
- Restriction in extraocular movements
- Inflammation
- Orbitocutaneous Fistula
Symptoms
- Diplopia if present within the orbit, but can often be asymptomatic .
Clinical Diagnosis
Dermoids, especially if superficial, may be diagnosed through physical exam.
Diagnostic procedures
If a deeper cyst is suspected, a computed tomography (CT) or magnetic resonance imaging (MRI) is indicated. It is described as a well-circumscribed lesion with a hyperdense wall and hypodense contents. Bony remodeling is present in 85% of cases.[2] Computed tomography can also rule out a dumbbell configuration, with part of the lesion in the orbit and part in the temporal fossa, connected through a bony defect at the suture line.[3][4]
Differential diagnosis
Medial lesions in infants may be confused with congenital encephaloceles, dacryoceles, and mucoceles.[3] Differential diagnosis of lateral lesions includes lacrimal tumors.[5]
Management
General treatment
Small, asymptomatic cysts may not require treatment. They may stabilize or even decrease in size over years.[7] However, some surgeons opt for early excision to avoid the risk of traumatic rupture in the future.[2]
Surgery
The mainstay of treatment is surgical.[8] For superficial lesions, an incision in the eyebrow, upper eyelid crease or directly over the lesion is often used.[9] For deep lesions, anterior, lateral, or combined orbitotomy is indicated. If possible, the surgeon attempts to remove the cyst in total without rupture.[2][3][4][5]
Complications
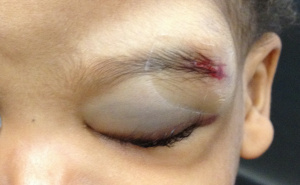
Various amounts of ecchymosis is common after surgical removal. Rarely it is massive like in the figure presented here. If the cyst ruptures during surgery, a lipogranulomatous inflammatory reaction may occur. This can be mitigated by copious irrigation at the time of surgery. Cysts extending through bony sutures often cannot be removed without rupture.[2] If incompletely removed, cysts may recur or lead to abscess formation. They inflammation from remaining dermoid tissue may also result in an orbitocutaneous fistula.[3][4]
Prognosis
Prognosis is excellent following successful early surgical intervention.[4]
Additional Resources
- American Academy of Ophthalmology. Eye Muscles. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/eye-muscles-list. Accessed November 17, 2022.
- Boyd K, DeAngelis KD, Turbert D. Ptosis. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/ptosis-list. Accessed November 17, 2022.
- Boyd K, Puente MA Jr, Turbert D. Strabismus (Crossed Eyes). American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/strabismus-in-children-2. Accessed November 17, 2022.
- Puente MA Jr, Lipsky SN, Turbert D. Adult Strabismus. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/strabismus-list. Accessed November 17, 2022.
References
- ↑ American Academy of Ophthalmology. Dermoid cyst of orbit. https://www.aao.org/image/dermoid-cyst-of-orbit-2 Accessed October 30, 2017.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Basic Clinical and Science Course. Pediatric Ophthalmology and Strabismus. 2013-14. Section 6 pg 343-344.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Basic Clinical and Science Course. Orbit, Eyelids, and Lacrimal System. 2013-14. Section 7 pg 36-37.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Cavazza S, Laffi GL, Lodi L, Gasparrini, Tassinari G. Orbital Dermoid Cyst of Childhood: Clinical Pathologic Findings, Classification and Management. Int Ophthalmol. 2011;31(3):93-97.
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 Sherman RP, Rootman J, Lapointe JS. Orbital dermoids: clinical presentation and management. Br J Ophthalmol. 1984;68: 642-652.
- ↑ Jump up to: 6.0 6.1 Basic Clinical and Science Course. Ophthalmic Pathology and Intraocular Tumors. 2013-14. Section 4 pg 229-230.
- ↑ Jump up to: 7.0 7.1 7.2 Shields J and Shields C. Orbital Cysts of Childhood – Classification, Clinical Features and Management. Surv Ophthalmol. 2004;49(3): 281-299.
- ↑ Yen KG, Yen MT. Current trends in the surgical management of orbital dermoid cysts among pediatric ophthalmologists. J Pediatr Ophthalmol Strabismus. 2006 Nov-Dec;43(6):337-40; quiz 363-4. doi: 10.3928/01913913-20061101-02. PMID: 17162969.
- ↑ Yen MT, Yen KG. The eyelid crease incision for dermoid cysts of the eyebrow in pediatric patients. Ann Plast Surg. 2006 Apr;56(4):465. doi: 10.1097/01.sap.0000202830.74630.ba. PMID: 16557090.