Prominent Corneal Nerves
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
The cornea is a highly specialized tissue that must simultaneously maintain a protective barrier for the eye against pathogens and environmental insults and yet provide a transparent and precisely shaped optical structure. Corneal nerves play an important role in stimulating defensive reflexes such as tearing, blinking, and aversion from noxious stimuli. As such, the cornea is a highly innervated structure, with a density of free nerve endings that is 300 to 600 times greater than the skin.[1] Long ciliary nerves are comprised of sensory fibers which penetrate the sclera posteriorly and course through the suprachoroidal space to the corneal limbus. These nerves then travel through the corneal stroma in a radial fashion and ultimately penetrate Bowman’s layer to provide free nerve endings to all levels of the epithelium.[2]
In vivo confocal microscopy (IVCM) allows significantly better analysis of corneal nerves with magnification of up to 800x in vivo as compared to standard slit lamp biomicroscopy with magnification of up to 40x.[3]Confocal microscopy makes conjugate the light rays focused by the condensing lens on the object and the light rays focused by the objective lens. This principle thereby reduces light reflections from outside the focal plane. IVCM does not disrupt the tissue being studied, and thus it is a helpful noninvasive technique, but it is not as readily available in each office as standard slit lamp biomicroscopy. The conditions listed in this synopsis involve prominent corneal nerves that can be seen at the standard slit lamp examination.
The thickest stromal corneal nerves (axon bundles) can be seen with the slit lamp biomicroscope typically in normal patients only in the peripheral one third of the cornea. Enlarged or prominent corneal nerves seen in the central cornea may be an early hallmark of important systemic diseases.[4] Noticing enlarged corneal nerves and investigating their etiology can be lifesaving in certain cases, such as individuals with undiagnosed multiple endocrine neoplasia. Corneal nerves can also become prominent in intrinsic corneal diseases (for reasons that are not fully known but may include increased myelination or degeneration of axons).
Systemic Causes of Prominent Corneal Nerves
Multiple Endocrine Neoplasia Type 2 (MEN 2 or MEN II)- divided into subtypes MEN 2A, MEN 2B, and familial medullary thyroid carcinoma (MTC), all autosomal dominant conditions arising from mutations of the RET gene. MEN 2A and 2B are associated with enlarged corneal nerves.
Multiple Endocrine Neoplasia 2B (MEN 2B)
MEN 2B is an autosomal dominant syndrome with high degree of sporadic occurrence from de novo mutations on the RET (Rearranged during Transfection) protooncogene on chromosome 10. Medullary thyroid cancer occurs in essentially 100% of carriers of the mutation, usually by young adulthood. Other findings include pheochromocytoma in 50% and Marfanoid habitus in 75% of genetically affected individuals. Oral findings include irregular, dome-shaped, pink, sessile mucosal neuromas on the anterior and lateral dorsal surface of the tongue in more than 90% of carriers, arising as early as infancy, and said to be almost pathognomonic for MEN 2B (see mucosal neuroma syndrome below as an exception), as well as mucosal neuromas near the vermilion border of the lips.[5] [6]
Ocular findings consist of prominent corneal nerves seen on slit lamp examination extending to the pupil area in almost 100% of carriers, seen as young as 2 years of age, mucosal neuromas of the eyelid margin creating a pink, undulating thickening and eversion of the eyelid margin, and dry eye (in 67% of carriers). Aqueous tear deficiency or inability to cry due to autonomic deficiency may be early signs of MEN. Young infants may also show diminished psychogenic or emotional crying due to temporary incomplete development of crying reflexes.[7]
Recognition of the prominent corneal nerves and mucosal neuromas on eyelids, tongue, and lips should prompt referral for MEN 2B workup (genetic and endocrine testing). It is recommended that patients who are carriers for MEN 2B have a prophylactic thyroidectomy to prevent medullary thyroid carcinoma, a surgery which can be lifesaving. A number of case reports document individuals referred by their ophthalmologists for testing for MEN in a setting of prominent corneal nerves who proved to have medullary thyroid carcinoma in situ, which was successfully removed before metastasis.[8] When faced with prominent corneal nerves in an otherwise normal cornea, one of the prime questions, to paraphrase Shakespeare, is “2B or not 2B?”
Multiple Endocrine Neoplasia 2A (MEN 2A)
MEN 2A has a high incidence of medullary thyroid carcinoma (95%) and pheochromocytoma (50%), but unlike MEN 2B, MEN 2A has a high frequency of parathyroid tumors (20-30%) and does not manifest mucosal neuromas or Marfanoid body habitus. Prominent corneal nerves have been described in MEN 2A, but not as frequently or as prominently as in MEN 2B.[9] The lack of easily visible mucosal neuromas makes the diagnosis of MEN 2A less obvious initially than that of MEN 2B, but MEN 2A should also be considered in individuals with prominent corneal nerves and otherwise normal corneas, and prophylactic thyroidectomy done if a diagnosis of MEN 2A confirmed.
Mucosal Neuroma Syndrome (MNS)
Multiple cases have been reported of mucosal neuroma syndrome (MNS), which consists of prominent corneal nerves and mucosal neuromas, but with no genetic defect on the RET gene and no associated endocrine tumors.[10]
Refsum disease
Corneal nerves may be prominent in Refsum disease, which is an autosomal recessive disorder caused by mutations in the PHYH and PEX7 gene.[11] Phytanic acid, a fatty acid acquired through dietary intake, accumulates abnormally in tissues, causing retinitis pigmentosa and nyctalopia, often starting in childhood, along with anosmia, and later in life ataxia, hearing loss, ichthyosis, and cardiac arrhythmia. Treatment involves dietary restriction of phytanic acid.
Riley-Day syndrome (Familial Dysautonomia)
Riley-Day syndrome or familial dysautonomia may be associated with prominent corneal nerves. The autosomal recessive syndrome with genetic locus on chromosome 9q31 affects primarily patients of Ashkenazi Jewish ancestry with congenital and progressive sensory and autonomic neuropathy ultimately leading to a reduced lifespan. Cardinal diagnostic findings include absence of emotional overflow tearing, absence of fungiform papillae on the tongue, absence of skin flare after intradermal histamine injection, diminished or absent deep tendon reflexes, and as above, Ashkenazi Jewish ancestry. Additional effects include diminished pain and temperature sensation, excessive sweating and salivation, blotching of skin, arterial hypertension, spinal deformities, ataxia, difficulty swallowing, and aspiration. Ophthalmic problems include alacrima, absent corneal reflexes, superficial keratitis, and optic atrophy that often starts at the end of the first decade of life.[12]
Neurofibromatosis Type 1 (NF 1)
NF 1 is an autosomal dominant disease carried on chromosome 17q11.2. Half of cases represent new mutations. Severity is highly variable, and morbidity may occur from optic pathway gliomas, spinal cord and peripheral nerve neurofibromas, scoliosis, and neurologic impairment. In addition to almost universal presence of café-au-lait spots and iris Lisch nodules, enlarged corneal nerves have been reported in various series in 0.5%, 6%, and 22% of patients.[13] [14]
Leprosy (Hansen’s Disease)
Leprosy is an infectious disease caused by Mycobacterium leprae which is rare in the U.S. but endemic in Asia, Africa, and Latina America. The incubation period may be as long as 8-10 years, causing granulomatous lesions of skin, organs, and sensory and motor nerves. Keratitis and uveitis may occur; however, enlarged, beaded corneal nerves, especially seen in the superotemporal cornea, may be an early finding of disease.[4]
Lipoid Proteinosis
Lipoid proteinosis, also called hyalinosis cutis et mucosae, is a rare autosomal recessive disorder carried on chromosome 1q21. Hyaline deposits occur on skin, mucous membranes, and viscera, beginning in early childhood. A hoarse cry may be noted in early infancy due to laryngeal involvement. Moniliform blepharosis, or bead-like papules along the eyelid margins, is a highly characteristic finding which helps in recognition of the diagnosis but may be noted in only about 50% of affected individuals. In a study by Al-Faky et al., prominent corneal nerves were seen with the slit lamp overlying the pupil margin or pupil axis in 7 of 7 lipoid proteinosis patients as young as 5 years of age, indicating that prominent corneal nerves may be a particularly useful aid in diagnosis of lipoid proteinosis.[15]
Ichthyosis
Ichthyosis is a heterogeneous group of hereditary diseases in which symmetrically distributed visible scales occur on the skin starting in infancy or childhood. Inheritance may be autosomal dominant, autosomal recessive, or X-linked. Punctate deep stromal opacities may occur throughout the cornea. Ichthyosis is often found on lists of etiologies for enlarged corneal nerves. Refsum disease (see above) is one cause of ichthyosis that is associated with prominent corneal nerves. In other types of ichthyosis, corneal nerves may occasionally become prominent. In a study by Jay et al., one of 62 patients were found to have “unusually prominent” corneal nerves.[16]
Prominent Corneal Nerves Due to Intrinsic Corneal Disease
Prominent corneal nerves may accompany corneal disease, including keratoconus, Fuch’s endothelial corneal dystrophy, posterior polymorphous corneal dystrophy (PPMD), Acanthamoeba keratitis, and herpes simplex and herpes zoster keratitis.
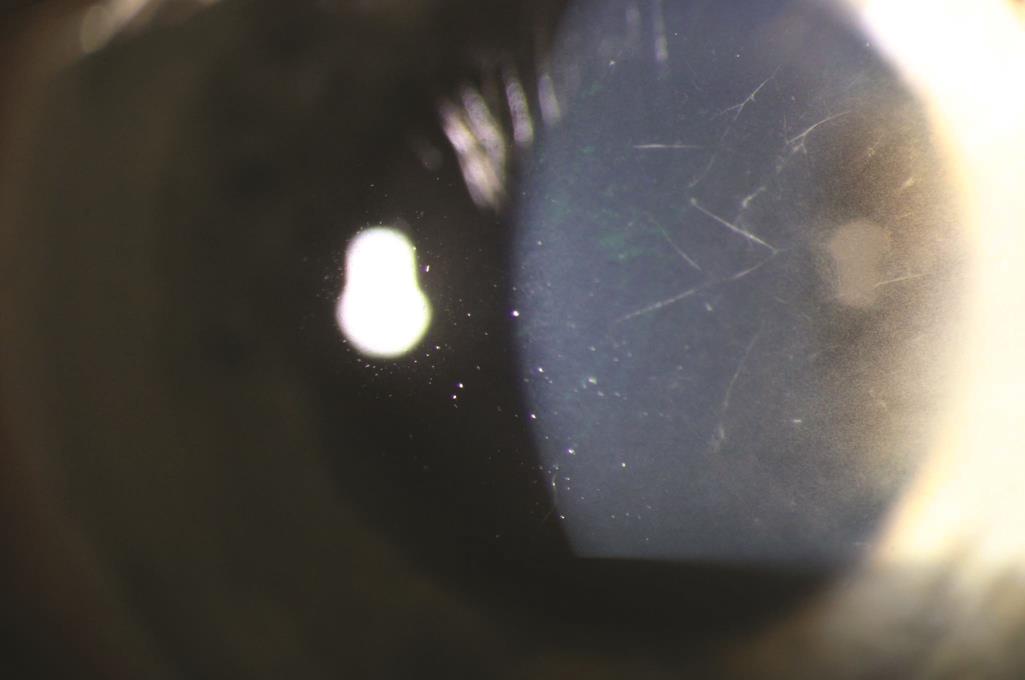
Radial keratoneuritis in Acanthamoeba keratitis
Acanthamoeba keratitis is a relatively rare but serious form of corneal infection usually associated with contact lens wear, especially extended wear use of contact lenses, cleaning contact lenses with tap water, and exposure of contact lenses to bath water or hot tub water. Acanthamoeba are free-living protozoa found in air, soil, dust, drinking water, and sea water. When the organisms invade the cornea, severe pain and photophobia typically occur, out of proportion to what would typically be expected in other conditions causing corneal infiltrates. Slit lamp examination may reveal epithelial pseudodendrites, multifocal stromal infiltrates, a surrounding Wessely immune ring (ring-shaped opacity), and radial keratoneuritis.[17]
The radial keratoneuritis consists of infiltrates surrounding corneal nerves, creating multiple, linear, branching stromal opacities starting in the paracentral cornea and extending toward the limbus. The cause of the perineural infiltration is not known but may occur due to a predilection for the organism to spread more easily adjacent to the corneal nerves. Radial keratoneuritis may occur in more than half of Acanthamoeba keratitis cases within the first month, but the findings diminish in frequency after that.[18] Since only a few nerves may be involved, a careful search of the cornea is recommended to detect the perineural infiltration. Although radial keratoneuritis is a classic finding of Acanthamoeba keratitis, it is not entirely pathognomonic, as it has been reported to occur in Pseudomonas keratitis as well. Ultimate diagnosis of Acanthamoeba keratitis may require in vivo confocal microscopy (IVCM) to visualize protozoal cysts, PCR or culture analysis of corneal scrapings, or histologic examination of surgical specimens.[19] Extended topical and sometimes surgical therapy is needed to eradicate the Acanthamoeba.
References
- ↑ Hegarty DM, Hermes SM, Yang K, Aicher SA. Select noxious stimuli induce changes on corneal nerve morphology. J Comp Neurol. 2017;525(8):2019-2031. doi:10.1002/cne.24191
- ↑ Shaheen BS, Bakir M, Jain S. Corneal nerves in health and disease. Surv Ophthalmol. 2014;59(3):263-285. doi:10.1016/j.survophthal.2013.09.002
- ↑ Cruzat A, Qazi Y, Hamrah P. In Vivo Confocal Microscopy of Corneal Nerves in Health and Disease. Ocul Surf. 2017;15(1):15-47. doi:10.1016/j.jtos.2016.09.004
- ↑ 4.0 4.1 Kim SK, Dohlman CH. Causes of Enlarged Corneal Nerves. Int Ophthalmol Clin. 2001;41(1):13-23.
- ↑ Javadi MA, Rezaei Kanavi M, Faramarzi A, Feizi S, Azizi F, Javadi F. Confocal scan imaging and impression cytology of the cornea in a case of multiple endocrine neoplasia type-2b. J Ophthalmic Vis Res. 2012;7(2):176-179.
- ↑ Morrison PJ, Nevin NC. Multiple endocrine neoplasia type 2B (mucosal neuroma syndrome, Wagenmann-Froboese syndrome). J Med Genet. 1996;33(9):779-782. doi:10.1136/jmg.33.9.779
- ↑ Brauckhoff M, Machens A, Hess S, et al. Premonitory symptoms preceding metastatic medullary thyroid cancer in MEN 2B: An exploratory analysis. Surgery. 2008;144(6):1044-1053. doi:10.1016/j.surg.2008.08.028
- ↑ Chamney S, O'Neill M, George S. Prominent corneal nerves. J Pediatr. 2014;165(3):636. doi:10.1016/j.jpeds.2014.05.025
- ↑ Kinoshita S, Tanaka F, Ohashi Y, Ikeda M, Takai S. Incidence of prominent corneal nerves in multiple endocrine neoplasia type 2A. Am J Ophthalmol. 1991;111(3):307-311. doi:10.1016/s0002-9394(14)72314-1
- ↑ Lekhanont K, Sontichai V, Bunnapradist P. Prominent corneal nerves, conjunctival neuromas, and dry eye in a patient without MEN2B. Can J Ophthalmol. 2019;54(6):e313-e317. doi:10.1016/j.jcjo.2019.02.008
- ↑ Jansen GA, Waterham HR, Wanders RJ. Molecular basis of Refsum disease: sequence variations in phytanoyl-CoA hydroxylase (PHYH) and the PTS2 receptor (PEX7). Hum Mutat. 2004;23(3):209-218. doi:10.1002/humu.10315
- ↑ Dietrich P, Dragatsis I. Familial Dysautonomia: Mechanisms and Models. Genet Mol Biol. 2016;39(4):497-514. doi:10.1590/1678-4685-GMB-2015-0335
- ↑ Arigon V, Binaghi M, Sabouret C, Zeller J, Revuz J, Soubrane G, Wolkenstein P. (2002). Usefulness of Systematic Ophthalmologic Investigations in Neurofibromatosis 1: A Cross-Sectional Study of 211 Patients. Eur J Ophthalmol. 2002;12(5):413-418. doi.org/10.1177/112067210201200512
- ↑ Huson S, Jones D, Beck L. Ophthalmic manifestations of neurofibromatosis. Br J Ophthalmol. 1987;71(3):235-238. doi:10.1136/bjo.71.3.235
- ↑ Al-Faky YH, Bosley TM, Al-Turki T, Salih MA, Abu-Amero KK, Alsuhaibani AH. Prominent corneal nerves: a novel sign of lipoid proteinosis. Br J Ophthalmol. 2012;96(7):935-940. doi:10.1136/bjophthalmol-2012-301617
- ↑ Jay B, Blach RK, Wells RS. Ocular manifestations of ichthyosis. Br J Ophthalmol. 1968;52(3):217-226. doi:10.1136/bjo.52.3.217
- ↑ Alfawaz A. Radial keratoneuritis as a presenting sign in acanthamoeba keratitis. Middle East Afr J Ophthalmol. 2011;18(3):252-255. doi:10.4103/0974-9233.84062
- ↑ Bacon AS, Frazer DG, Dart JK, Matheson M, Ficker LA, Wright P. A review of 72 consecutive cases of Acanthamoeba keratitis, 1984-1992. Eye (Lond). 1993;7 (Pt 6):719-725. doi:10.1038/eye.1993.168
- ↑ Szentmáry N, Daas L, Shi L, et al. Acanthamoeba keratitis - Clinical signs, differential diagnosis and treatment. J Curr Ophthalmol. 2018;31(1):16-23. Published 2018 Oct 19. doi:10.1016/j.joco.2018.09.008