Morgagnian Cataract
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Morgagnian Cataract is recognized by the following codes as per the International Classification of Diseases (ICD) nomenclature:
ICD - 10
- H25.20 Age-related cataract, morgagnian type, unspecified eye
- H25.21 Age-related cataract, morgagnian type, right eye
- H25.22 Age-related cataract, morgagnian type, left eye
- H25.23 Age-related cataract, morgagnian type, bilateral
Disease
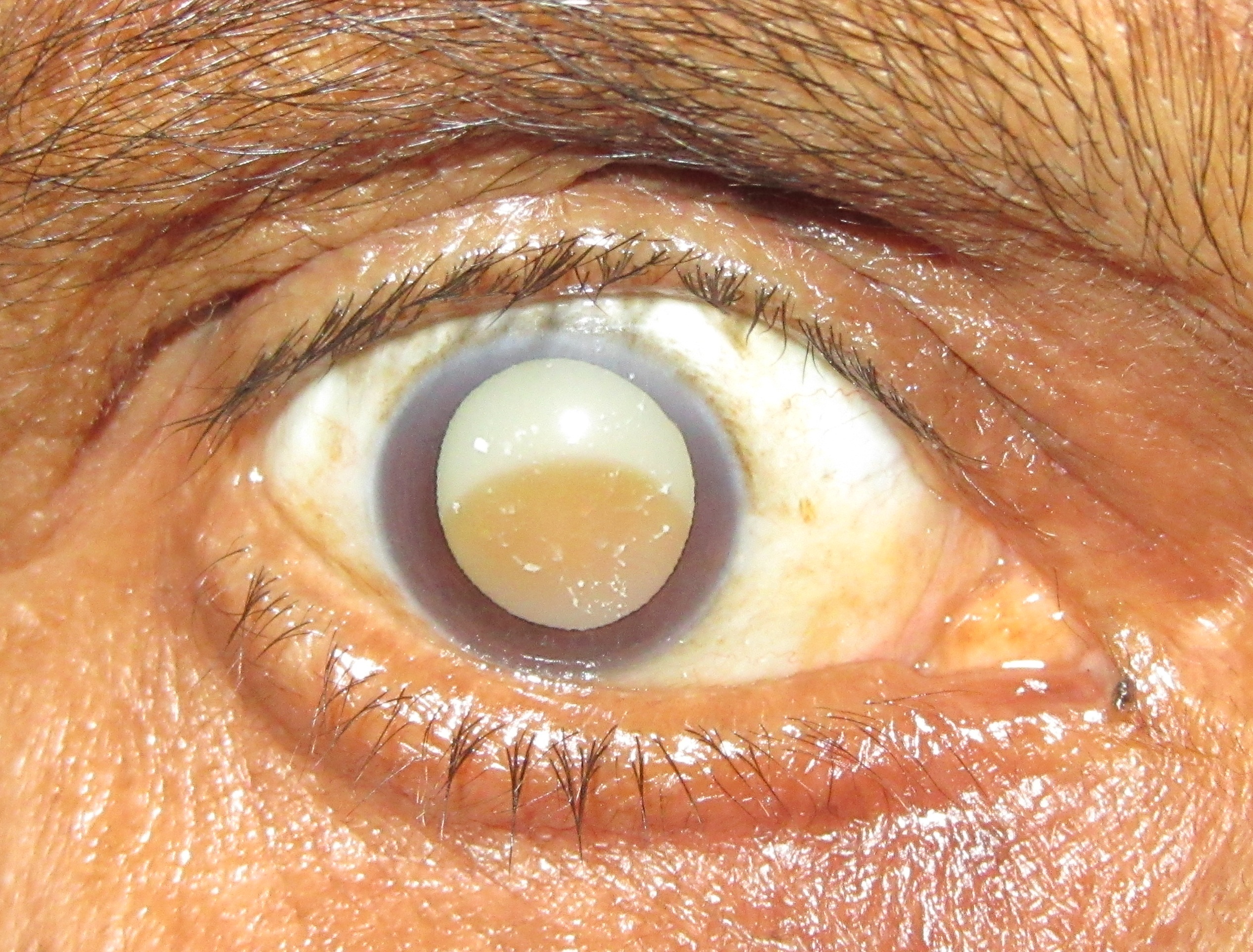
Morgagnian cataract is a form of hypermature cataract formed by liquefaction of the cortex and sinking of the dense nucleus to the bottom of the capsular bag.[1] The name "Morgagnian" derives from Giovanni Battista Morgagni, the 18th century anatomical pathologist.[2]
Epidemiology
In most developed countries cataract surgeries are done as soon as it becomes visually disabling. Morgagnian cataracts are more commonly seen in developing countries due to late presentation.
Risk Factors
It is commonly an age related acquired condition. However, factors that increase the risk of cataract formation, such as chronic sunlight exposure, uncontrolled diabetes, intra-ocular inflammation, or steroid use, can be associated risk factors.
Pathophysiology
It appears that the Morgagnian cataract is a special form of cortico-nuclear cataract. It is assumed that the process of fibre dissolution, which is encountered in cortical cataracts in general, is sped up and occurs en masse in the Morgagnian cataract.[3] Histopathologically, accumulation of eosinophilic fluid between lens cells with displacement and degeneration of bordering cells characterize cortical cataracts. Spherical droplets or globules of released protein from the breakdown of cortical cell walls are called Morgagnian globules. These globules may accumulate and may eventually replace the entire cortex and result in a mature Morgagnian cataract. The central dense nucleus at this point would become gravity dependent often displaced inferiorly to the lower equatorial region of the lens within the capsular bag. [4]
Diagnosis
Morgagnian cataract is a clinical diagnosis.
Signs
- Decreased visual acuity - gradually progressive and painless
- Dense nucleus floating freely in the liquified cortex
- Triangle sign - Slit lamp examination with a narrow-slit beam angled at 60° with a magnification of 16x-20x focused above the nucleus shows a triangular area bounded anteriorly and posteriorly by the anterior and posterior lens capsule and the base of the triangle formed by the lens nucleus. This finding is named because of the triangular space formed by the anterior and posterior lens capsule and the nucleus below. [5]
- Flecks of calcium deposits in the anterior capsule may be seen.
- Absence of red fundus glow in retinoscopy
Symptoms
- Blurring of vision and glare may be early signs of developing cataract
- Morgagnian cataracts will typically present with profound visual loss (hand-motions or light-perception)
Complications
- Morgagnian cataract may undergo spontaneous rupture into anterior chamber causing inflammatory reaction, which is known as phacoanaphylactic uveitis.
- Spontaneous rupture of lens capsule may cause secondary glaucoma.[6]
- It may also be complicated with phacolytic glaucoma when the lens protein leaks through an intact capsule and clog the trabecular meshwork obstructing the aqueous outflow.
Preoperative workup
- Assessment of visual potential by checking accurate light projections and swinging flashlight test to detect a relative afferent pupillary defect.
- B-scan ultrasound study for posterior segment evaluation to rule out complicated co-existing intraocular diseases.
- Measurements of the corneal refractive power and immersion A-scan to determine the power of the IOL required.
Differential diagnosis
- Inferiorly subluxated cataractous lens - The triangle sign can be helpful in making the correct diagnosis. A clear transparent space is observed above the cataractous lens in both the scenarios and can lead to confusion when examined under diffuse illumination with a slit lamp. The triangle sign is present in the cases of Morgagnian cataract with resorbed cortex due to the presence of the intact zonules and the capsular bag whereas it is absent in the cases of the inferiorly subluxated cataractous lens due to loss of zonules.
- White cataract
- Traumatic cataract
Management
Surgical removal of the cataractous lens followed by intraocular lens implantation is the treatment modality of choice.
Surgery
- Extracapsular Cataract extraction (ECCE), Small incision cataract surgery (SICS) or phacoemulsification can be performed for cataract extraction. This is followed by intraocular lens implantation (posterior chamber intraocular lens (PCIOL )/ anterior chamber intraocular lens (ACIOL)
- Intraocular lens scaffold technique has been described to prevent posterior capsule rupture for phacoemulsification of a Morgagnian cataract. This technique uses the IOL as a scaffold to prevent the vulnerable posterior capsule from rupturing during nuclear emulsification in Morgagnian cataract. The technique prevents rupture of the floppy posterior capsule by providing a constant support to it. The scaffold provides stable inflation of the capsular bag and prevents inadvertent emulsification. Concurrently, it prevents dehiscence of weak zonular fibers by minimizing the stress on the zonular apparatus.[7]
Surgical challenges
- Creation of a continuous curvilinear capsulorhexis is challenging due to an often fibrous anterior capsule and increased intralenticular pressure. Increased intralenticular pressure may result in an Argentinian flag sign and radialized capsular tear with vitreous loss.
- The surgical view may be poor due to lack of red reflex or due to the liquified cortical material in the anterior chamber.
- The posterior capsule is often floppy during nuclear removal, which often requires high energy to remove due to density. This can predispose to posterior capsule rent or rupture.
- Liquified cortex is often easily removed from the capsular bag once phacoemulsification is started, leaving a small dense and mobile nuclear material behind for phacoemulsification. Viscoelastic injected into the capsular bag can be used to stabilize the mobile nucleus and prevent anterior prolapse of the posterior capsule during surgery.
- Rarely, a Morgagnian cataract may be associated with an isolated posterior capsular opening without any history of trauma.[8]
Surgical Complications
- Uncontrolled radial tear of anterior capsule
- Posterior capsular rent
- Nuclear material dropped into the vitreous through loss of capsular integrity
- Endothelial cell damage from excessive phacoemulsification energy
Prognosis
- Patients should be counseled about the increased risk of complications and the possible need of more than one surgery to achieve the best visual outcome.
- Preoperative assessment for projection of light and relative afferent pupillary defect are important prognostic factors.
- Patients should also be cautioned about possible binocular diplopia post cataract removal if morgagnian cataract was longstanding and may have lead to loss of fusion.
References
- ↑ Basic Clinical Science Course (BCSC) of the American Academy of Ophthalmology. Section 11. 2014 - 2015.
- ↑ Rozenbaum I. The Faces Behind the Eponyms. Arch Ophthalmol. 2008;126(6):846. doi:10.1001/archophthalmol.2007.63
- ↑ Bron AJ, Habgood JO. Morgagnian cataract. Trans Ophthalmol Soc U K. 1976 Jul;96(2):265-77.
- ↑ Roger F. Steinert. Cataract surgery 3rd edition. Chapter 1, The pathology of cataracts. CA, USA: Elsevier Inc.; 2010
- ↑ Deshmukh S, Bhattacharjee H, Gupta K. “Triangle sign”in Morgagnian cataract. Indian J Ophthalmol 2019;67:137.
- ↑ KAUFMAN SI. Morgagnian cataracts and their complications: with report of a case of spontaneous rupture of the lens capsule causing secondary glaucoma. Archives of Ophthalmology. 1933 Jan 1;9(1):56-63.
- ↑ Parkash RO, Mahajan S, Parkash TO, Nayak V. Intraocular lens scaffold technique to prevent posterior capsule rupture in cases of Morgagnian cataract. Journal of Cataract & Refractive Surgery. 2017 Jan 1;43(1):8-11.
- ↑ Takamura Y, Oishi N, Kubo E, Tsuzuki S, Akagi Y. Morgagnian cataract with an isolated posterior capsular opening. Archives of Ophthalmology. 2003 Oct 1;121(10):1487-8.