Lens Induced Glaucomas
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Lens induced glaucoma
Introduction
Lens-induced glaucoma may occur as either secondary angle-closure or open-angle glaucoma. The angle-closure can be caused by lens swelling (phacomorphic glaucoma) or lens dislocation (ectopia lentis). The open-angle glaucomas include glaucoma related to: leakage of lens proteins through the capsule of a mature or hypermature cataract (phacolytic glaucoma), obstruction of the trabecular meshwork following cataract extraction, capsulotomy, or ocular trauma by liberated fragments of lens material (lens-particle glaucoma), and hypersensitivity to own lens protein following surgery or penetrating trauma (phacoantigenic glaucoma). The pathophysiology, diagnosis and treatment of these different lens-induced glaucomas will be reviewed in this article [1] [2] [3] [4].
Lens induced secondary angle-closure glaucoma
Phacomorphic Glaucoma
Pathophysiology
Phacomorphic glaucoma is a lens-induced secondary angle-closure glaucoma that may occur as a result of mature cataract formation. Narrowing of the angle can occur slowly with formation of the cataract by pushing the iris forward or acutely precipitated by an intumescent cataractous lens leading to obstruction of aqueous flow between the border of the pupil and the anterior capsule of the lens (pupillary block) [1][4][5]
Diagnosis
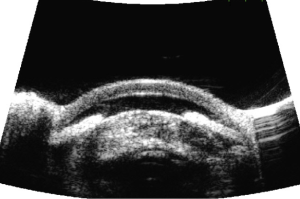
Phacomorphic Glaucoma is diagnosed by the presence of eye pain, history of decreased vision, evidence of mature cataract formation (slit lamp exam), angle closure (gonioscopy), and elevated intraocular pressure (applanation tonometry) in the affected eye. Distinguishing factors between primary angle-closure and phacomorphic angle-closure are presence of an intumescent cataractous lens and presence of cell and flare. Axial length measurement (usually short in phacomorphic) and records of the refraction may also be helpful in distinguishing between the two conditions .[2][4][5][6] In primary angle-closure the fellow eye has shallow anterior chamber, but in phacomorphic glaucoma the fellow eye usually has normal anterior chamber depth or pseudophakia. Ultrasound biomicroscopy (UBM) can assist in the diagnosis and may show a dense cataractous lens causing mass effect on the iris with anterior bowing and closed angles (Figure 1).
Management
Initial treatment of phacomorphic glaucoma is to lower the intraocular pressure with medical therapy such as topical beta blockers, carbonic anhydrase inhibitors and hyperosmotic agents such as oral glycerin or intravenous mannitol. Parasympathomimetic agents should be used with caution since they can precipitate pupillary block. If the intraocular pressure is not controlled with medical therapy alone, a laser iridotomy is usually performed, other options include corneal depression with a Zeiss 4-mirror lens. If the fellow eye is also predispose to angle closure glaucoma, prophylactic laser iridotomy should be performed. Definitive treatment consists of cataract extraction and often clinicians will begin planning for surgery at diagnosis. [4] [5][7] [8][6]
Glaucoma induced by Lens-dislocation
Pathophysiology
Secondary angle-closure glaucoma may occur if the lens is displaced from its normal anatomical position (Ectopia lentis). Forward displacement of the lens may result in narrowing of the anterior chamber angle and pupillary block causing secondary angle-closure. Ectopia lentis may be present as an isolated clinical entity secondary to trauma or associated with systemic disorders such as Weill-Marchesani syndrome, Marfan's syndrome, homocystinuria, among others. The biochemical defects in these conditions result in defective lens fibers (zonular fibers that suspend the lens in position), often causing subluxation/dislocation of the lens, thus increasing the risk of secondary angle-closure [1][6][9] [10] [11] [12] [13]
Diagnosis
The clinical presentation of Ectopia lentis varies according to the individual state of the lens but when dislocation of the lens results in angle-closure and pupillary block, patients usually present with a painful eye, decreased visual acuity, and history of difficulties with accommodation and near vision. Diagnosis is made by the presence of a dislocated/subluxated lens, angle-closure, and intraocular pressure elevation in the affected eye [2][6][9].
Management
The management of glaucoma induced by ectopia lentis depends on the degree of lens dislocation and the presence of pupillary block. In cases of partial subluxation without pupillary block, conservative treatment with intraocular pressure monitoring could be followed. If pupillary block is present, 2 laser iridotomies 180 degrees apart should be created, to avoid simultaneous blockage by the lens. When total anterior dislocation occurs, removal of the lens is the definitive treatment [2][6][9].
Lens induced open-angle glaucoma
Phacolytic Glaucoma
Pathophysiology
Phacolytic glaucoma is caused by an inflammatory process caused by the leakage of lens material through the capsule of a mature cataract. The released lens material is composed of altered lens protein, macrophages, and other inflammatory cells that lead to trabecular meshwork obstruction and precipitate glaucoma. [1] [2] [3] [4] [14] [15] [16] The American Academy of Ophthalmology's Pathology Atlas contains a virtual microscopy image of Phacolytic Glaucoma[17].
Diagnosis
The typical presentation of phacolytic glaucoma is a painful eye with photophobia, decreased vision, and severe conjunctival hyperemia, often in an older patient with a history of poor vision. Diagnosis is usually made by the presence of prominent cell or white material/particles in the anterior chamber, flare reaction WITHOUT keratic precipitates (distinguishing this entity from phacoantigenic glaucoma), corneal edema, increased intraocular pressure, and evidence of a mature cataract. Pseudohypopyon may also be present (lens protein deposits layering in the inferior angle). Gonioscopy reveals an open anterior chamber angle. [1] [2] [3] [4][6][14]
Management
Patients with phacolytic glaucoma should be treated initially with topical cycloplegia, topical steroids, and aqueous suppressants. The immediate goal of therapy is to reduce the inflammation and to reduce the intraocular pressure. Cataract extraction is the definitive treatment for phacolytic glaucoma.[1] [2] [3] [4][6][14]
Lens-Particle Glaucoma
Pathophysiology
Lens particle glaucoma, in contrast to phacolytic glaucoma, is secondary to a "disruption of the lens capsule", which may occur after cataract surgery, penetrating lens injury, or laser posterior capsulotomy. The disrupted lens releases lens particle material in the anterior chamber leading to the obstruction of the aqueous outflow [1] [2] [3][6]
Diagnosis
The presentation is usually delayed for a few weeks after the precipitating event, but it may occur months or years later. A history of surgery or trauma is an important element in making an accurate diagnosis. Clinical findings include elevated intraocular pressure and evidence of cortical lens material in the anterior chamber. Other possible signs are corneal edema, synechiae, and cell/flare reaction in the anterior chamber. [2] [3][6][18] [19] [20]
Management
Medical therapy is initially aimed to control the intraocular pressure, topical steroids may be given to reduce inflammation, and mydriatics to prevent synechiae formation. If the lens particle/material does not resorb, there is a large amount of lens material in the anterior chamber and the intraocular pressure cannot be controlled, surgical removal of the lens is undertaken [1] [2] [3][18] [19] [20]
Phacoantigenic Glaucoma (formerly known as Phacoanaphylaxis)
Pathophysiology
Phacoantigenic glaucoma is a granulomatous inflammatory reaction directed against own lens antigens after surgery or penetrating trauma, leading to obstruction of the trabecular meshwork and increased intraocular pressure. It is important to mention that phacoanaphylaxis is not the correct name of this condition since it is not an allergy. The mechanism causing the reaction seems to be an Arthus-type immune complex reaction mediated by IgG and the complement system. [1][3][6][21] [22] [23] [24] [25]
Diagnosis
Phacoantigenic glaucoma usually occurs between one and fourteen days after cataract surgery or trauma. Clinical findings include keratic precipitates, anterior chamber cell/flare reaction, synechiae and residual lens material. Less common is the presence of glaucomatous optic neuropathy [1][3][6]
Management
Initial therapy is to control the intraocular pressure with IOP-lowering medications and to reduce the inflammation with topical steroids. If medical treatment is unsuccessful, surgical removal of residual lens material is indicated once inflammation is under control. [1] [2] [3][6][23]
References
- ↑ Jump up to: 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Ellant JP, Obstbaum SA. Lens-induced glaucoma. Doc Ophthalmol. 1992;81(3):317-38.
- ↑ Jump up to: 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Epstein DL. Diagnosis and management of lens-induced glaucoma. Ophthalmology. 1982 Mar;89(3):227-30.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Richter C, Epstein DL. Lens-induced open-angle glaucoma. In: Ritch R, Shields MB, Krupin T, eds. The Glaucomas. 2nd ed. St Louis: Mosby; 1996.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Kanski J, Brad Bowling. Lens-related glaucoma. In: kanski J, Brad Bowling, eds. Clinical Ophthalmology: A systematic approach. 7th ed. Elsevier Saunders; 2011.
- ↑ Jump up to: 5.0 5.1 5.2 Sowka J. Phacomorphic glaucoma: case and review. Optometry. 2006 Dec;77(12):586-9.
- ↑ Jump up to: 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Papaconstantinou D, Georgalas I, Kourtis N, Krassas A, Diagourtas A, Koutsandrea C, Georgopoulos G. Lens-induced glaucoma in the elderly. Clin Interv Aging. 2009;4:331-6.
- ↑ Lee JW, Lai JS, Yick DW, Yuen CY. Argon laser peripheral iridoplasty versus systemic intraocular pressure-lowering medications as immediate management for acute phacomorphic angle closure. Clin Ophthalmol. 2013;7:63-9.
- ↑ Lee SJ, Lee CK, Kim WS. Long-term therapeutic efficacy of phacoemulsification with intraocular lens implantation in patients with phacomorphic glaucoma. J Cataract Refract Surg. 2010 May;36(5):783
- ↑ Jump up to: 9.0 9.1 9.2 Jarret WH. Dislocation of the lens. Arch Ophthalmol. 1967; 78: 289-296.
- ↑ Dureau P. Pathophysiology of zonular diseases. Curr Opin Ophthalmol. 2008 Jan;19(1):27-30.
- ↑ Izquierdo NJ, Traboulsi EI, Enger C, Maumenee IH. Glaucoma in the Marfan syndrome. Trans Am Ophthalmol Soc. 1992;90:111-7; discussion 118-22.
- ↑ Chu BS. Weill-Marchesani syndrome and secondary glaucoma associated with ectopia lentis. Clin Exp Optom. 2006 Mar;89(2):95-9.
- ↑ Elkington AR, Freedman SS, Jay B, Wright P. Anterior dislocation of the lens in homocystinuria. Br J Ophthalmol. 1973 May;57(5):325-9.
- ↑ Jump up to: 14.0 14.1 14.2 Flocks M, Littwin CS, Zimmerman LE. Phacolytic glaucoma: a clinicopathological study of 138 cases of glaucoma associated with hypermature cataract. Arch Ophthalmol. 1955;54:37–45.
- ↑ Yanoff M, Scheie HG. Cytology of human lens aspirate. Its relationship to phacolytic glaucoma and phacoanaphylactic endophthalmitis. Arch Ophthalmic. 1968;80:166–170.
- ↑ Epstein DL, Jedziniak J, Grant WM. Identification of heavy molecular weight soluble protein in aqueous humor in human phacolytic glaucoma. Invest Ophthalmol Vis Sci. 1978;17:398–402.
- ↑ Ocular Pathology Atlas. American Academy of Ophthalmology Web site. https://www.aao.org/resident-course/pathology-atlas. Published 2016. Accessed January 4, 2017.
- ↑ Jump up to: 18.0 18.1 Kee C, Lee S. Lens particle glaucoma occurring 15 years after cataract surgery. Korean J Ophthalmol. 2001 Dec;15(2):137-9.
- ↑ Jump up to: 19.0 19.1 Jain SS, Rao P, Nayak P, Kothari K. Posterior capsular dehiscence following blunt injury causing delayed onset lens particle glaucoma. Indian J Ophthalmol. 2004 Dec;52(4):325-7.
- ↑ Jump up to: 20.0 20.1 Kim TH, Kim SJ, Kim E, Chung IY, Park JM, Yoo JM, Song JK, Seo SW. Spontaneous anterior lens capsular dehiscence causing lens particle glaucoma. Yonsei Med J. 2009 Jun 30;50(3):452-4.
- ↑ Marak GE, Font RL, Alepa FP. Experimental lens-induced granulomatous endophthalmitis. Mod Probl Ophthalmol. 1976;16: 75–79.
- ↑ Thach AB, Marak GE Jr, McLean IW, Green WR. Phacoanaphylactic endophthalmitis: a clinicopathologic review. Int Ophthalmol. 1991;15:271–279.
- ↑ Jump up to: 23.0 23.1 Riise P. Endophthalmitis phacoanaphylactica. Am J Ophthalmol. 1965;60:911–915.
- ↑ Easom HA, Zimmerman LE. Sympathetic ophthalmia and bilateral phacoanaphylaxis. Arch Ophthalmol. 1964;72:9–15.
- ↑ Allen JC. Sympathetic uveitis and phacoanaphylaxis. Am J Ophthalmol. 1967;63:280–283.