Eyelash Ptosis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
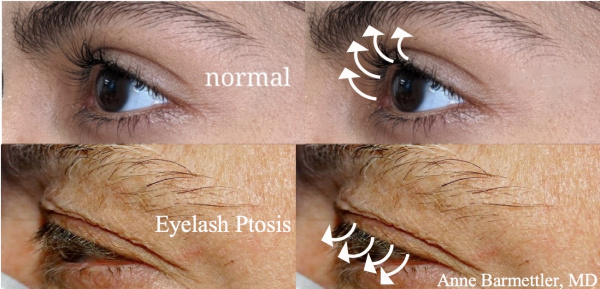
Eyelash ptosis is a condition characterized by the downward angle of the eyelashes of the upper eyelid. Normally, eyelashes project anteriorly and superiorly, but in eyelash ptosis, eyelashes project inferiorly toward the visual axis (see below).
This can result in foreign body sensation, visual field obstruction, and cosmetic complaints.
Normal anatomy: The upper eyelid has between 90 to 160 lashes; the eyelash bulbs are in the orbicularis oculi (called the muscle of Riolan at the eyelid margin) anterior to the tarsus and the body of the lash exits through the eyelid margin, anterior to the meibomian gland orifices. [1][2]
Etiology
Eyelash ptosis can be congenital or acquired, occurring when the integrity of the orbicularis oculi muscle, Riolan’s muscle, tarsal plate or elastin are compromised. Eyelash ptosis has been associated with conditions such as Floppy Eyelid Syndrome, congenital and acquired blepharoptosis, ocular leprosy, congenital lamellar ichthyosis, facial nerve palsy, and prostaglandin analog (PGA) usage.
Floppy Eyelid Syndrome (FES) is a disorder of the upper eyelid defined by papillary conjunctivitis with easy eversion of the upper lid, spontaneous eversion during sleep, discomfort, and a ‘rubbery’ tarsal plate. FES is known to be associated with obesity, obstructive sleep apnea, Down syndrome, and keratoconus. In FES, patients present with both eyelash ptosis and eye lash misalignment. Given that eyelash ptosis is often seen in FES, its presence on physical exam must alert clinicians to examine for concurrent lid laxity.[3]
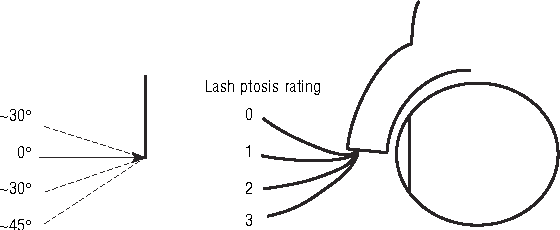
Blepharoptosis refers to the abnormal low-lying position of the upper eyelid margin when the eye is in primary gaze. Congenital causes are primarily due to a local myogenic dysgenesis of the levator palpebrae superiori muscle, while acquired causes are due to the stretching, dehiscence, or disinsertion of the levator aponeurosis. Eyelash ptosis is common in blepharoptosis and, in one study, the prevalence of severe eyelash ptosis was 89.6% in those with blepharoptosis and 6.7% in those without. This grading system was based on the degrees relative to the horizontal relative to the eyelid margin: eyelashes oriented 0° to 30° below the horizontal relative to the eyelid margin were rated as mild while those with an orientation 31° to 45° below the horizontal relative to the eyelid margin were rated at severe.[4]
Leprosy (Hansen’s Disease) is a chronic granulomatous inflammatory disease due to bacterium Mycobacterium leprae. Up to 75% of individuals with leprosy have ocular involvement.[5]Guimarães and Cruz noted eyelash ptosis in 48 out of 74 patients (65%) with long-standing ocular leprosy.[6]
Eyelash ptosis has also been reported in patients with congenital lamellar ichthyosis, a condition which causes extreme drying of the skin.[7]Eyelash ptosis has also been associated with facial nerve palsy. In one study focused on complications after acoustic neuroma resection, 26 out of 62 patients (42%) with facial palsy had eyelash ptosis as a long-term complication.[8]There have also been case reports of eyelash ptosis secondary to trichomegaly following latanoprost (PGA) use (for both IOP lowering and for increased lash growth).[9]
Risk Factors
As described above, eyelash ptosis is often seen in association with multiple other disease states, and therefore, these conditions serve as significant risk factors for the development of eyelash ptosis. For example, obesity and obstructive sleep apnea are associated with FES and can therefore increase one’s risk for eyelash ptosis. Similarly, blepharoptosis, ocular leprosy, congenital lamellar ichthyosis, facial nerve palsy and latanoprost use increase one’s risk for developing eyelash ptosis.
Pathophysiology
Eyelashes lack arrector pili muscles, small muscles attached to most mammalian hair follicles which upon contraction, cause the hair to stand on end. Eyelash position is instead dependent upon support from the surrounding structures such as the orbicularis oculi, its insertion into the eyelid margin (muscle of Riolan), and the tarsal plate. Anatomic changes within the upper eyelid structures are believed to be the cause of eyelash ptosis.[10]
In the case of FES, research has indicated that patients have decreased amounts of elastic fibers or elastin within the eyelid skin and tarsal plate as compared to control subjects. In one particular study, immunohistochemistry staining indicated an increase in matrix metalloproteases, enzymes capable of degrading extracellular matrix, and subsequent decrease in elastin. The decreased elastin content and increased eyelid laxity is the hypothesized cause of eyelash ptosis if FES.[11]Similarly, in congenital and acquired blepharoptosis, laxity of the anterior lamellar structures and or connective tissue malformation contribute to eyelash ptosis. In facial nerve palsy, the loss of muscle tone to the pretarsal orbicularis and Riolan muscle have been cited as the causes of eyelash ptosis. Eyelash ptosis secondary to trichomegaly following latanoprostuse is thought to be due to the increased weight of the lashes which overwhelm the supporting structures.[12]
Diagnosis
History
Review of all ocular, systemic, and topical medications should be performed with special attention to prostaglandins (both those used for IOP lowering and those used for lash growth)
Exam
Workup includes visual acuity, pupillary exam, extraocular motility, cranial nerve exam with special attention for facial nerve weakness, margin to reflex distance 1 (MRD1), levator function, and orbicularis oculi muscle strength. Eyelid margin position must be carefully examined to rule out pseudo-lash ptosis secondary to cicatricial entropion.[12]The eyelashes should be examined for contour, angle, direction, and length.
Eyelash ptosis can be graded with the Lash Ptosis Rating (LPR) system (see below) based off of the angular displacement that occurs as the eyelash extends anteriorly in primary gaze (chin parallel to the ground).
An LPR of 0 indicates the natural position of a non-ptotic eyelash and relative to the eyelid margin, will have lashes which are oriented at 0º to greater than 30º above the horizontal meridian. Eyelashes oriented 0º-30º below the horizontal are rated as an LPR of 1. Eyelashes oriented 30º-45º below the horizontal meridian are rated as 2, and eyelashes oriented at greater than 45º below are rated as a LPR of 3. Documenting the degree of eyelash ptosis separately for each eye should take care to note variability between the two sides. This is important as severity may require differing surgical repair techniques or even different etiolologies.[4][12]
Symptoms
If the eyelash ptosis is severe enough to obscure the line of sight, visual obstruction may be present. Eyelash projection can also project towards the globe, causing irritation and foreign body sensation. Finally, eyelash ptosis can cause cosmetic complaints.
Management
Treatment begins with addressing the underlying cause, if possible, and may also include both conservative and surgical treatment. For example, the use of CPAP nightly in FES, has been shown to decrease floppiness and may lessen the likelihood of surgical repair (typically via pentagonal wedge resection of the excess horizontal laxity).[13] Additionally, weight loss due to bariatric surgery has been associated with improved eyelid laxity, as measured by medial canthal tendon laxity.[14]
Conservative Therapy
Discontinuing PGA analog use can be considered. In the case of FES, nocturnal eye shields can be considered.[15]
Epilation can be performed, however, patients should be warned that eyelashes will grow back in 6-12 weeks. Other procedures, such as electrocautery of hair bulb can be performed, but this results in permanent removal of the eyelids.[16]
Surgery
Anterior lamellar repositioning is one surgical approach to correct eyelash ptosis. The upper lid crease is marked along the skin crease and skin excised as in a routine blepharoplasty. Sometimes this alone is sufficient. If additional upward rotation is desired, the lower skin incision can be fixated at a higher location, as in a crease formation surgery. This is typically done by fixating the orbicularis oculi muscle from the inferior edge of the defect to the levator muscle at the desired height of a future eyelid crease.
If horizontal laxity exists, the procedure begins by creating a lateral tarsal strip of the upper eyelid. The lateral anterior lamella is excised off of the lateral tarsal strip. Dissection is carried through to the anterior orbital rim. Double armed 5-0 vicryl or prolene is used to make partial thickness passes through the tarsal strip and through the periosteum of the lateral orbital rim. The lateral canthus is then reformed.
Mild to moderate overcorrection is recommended as in the postoperative period the eyelash angle typically drops slightly.[12]
Prognosis
The overall prognosis is dependent on one’s ability to adequately manage and treat the underlying condition. With the exception of FES, which is a chronic progressive condition, typically requiring multiple surgeries, most patients with eyelash ptosis will be satisfied with their postoperative results.
References
- ↑ Patel BC, Abdul W, Joos ZP. Anatomy, Head and Neck, Eyelash. [Updated 2019 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537278/
- ↑ Aumond, Sarah, and Etty Bitton. “The Eyelash Follicle Features and Anomalies: Review.” Journal of Optometry, vol. 11, no. 4, 2018, pp. 211 222.,doi:10.1016/j.optom.2018.05.003.
- ↑ Ezra, Daniel G., et al. “Floppy Eyelid Syndrome: Stretching the Limits.” Survey of Ophthalmology, vol. 55, no. 1, 2010, pp. 35–46., doi:10.1016/j.survophthal.2009.02.025.
- ↑ Jump up to: 4.0 4.1 Malik, K. J., Lee, M. S., Park, D. J. J., & Harrison, A. R.(2007). Lash ptosis in congenital and acquired blepharoptosis. Archives of Ophthalmology, 125(12), 1613-1615. https://doi.org/10.1001/archopht.125.12.1613
- ↑ Grzybowski A, Nita M, Virmond M. Ocular leprosy. Clin Dermatol. 2015 Jan-Feb. 33 (1):79-89.
- ↑ Guimarães FC, Cruz AA. Eyelid changes in long-standing leprosy. Ophthal Plast Reconstr Surg1998;14 (4) 239- 243
- ↑ Singh AJ, Atkinson PL. Ocular manifestations of congenital lamellar ichthyosis. Eur J Ophthalmol2005;15 (1) 118- 122
- ↑ Mulhern MG, Aduriz-Lorenzo PM, Rawluk D, et al. Ocular complications of acoustic neuroma surgery. Br J Ophthalmol1999;83 (12) 1389- 1392
- ↑ Casson RJ, Selva D. Lash ptosis caused by latanoprost. Am J Ophthalmol2005;139 (5) 932- 933
- ↑ Langford JD, Linberg JV. A new physical finding in floppy eyelid syndrome Ophthalmology, 105 (1) (1998), pp. 165-169
- ↑ Schlötzer-Schrehardt U, Stojkovic M, Hofmann-Rummelt C, Cursiefen C, Kruse FE, Holbach LM. The pathogenesis of floppy eyelid syndrome: involvement of matrix metalloproteinases in elastic fiber degradation Ophthalmology, 112 (4) (2005), pp. 694-704
- ↑ Jump up to: 12.0 12.1 12.2 12.3 Zaldívar R.A., Lee M.S., Harrison A.R. (2011) Lash Ptosis. In: Cohen A., Weinberg D. (eds) Evaluation and Management of Blepharoptosis. Springer, New York, NY
- ↑ Porta R, Comini L, Barbano L, Bianchi L, Vitacca M. A case of obstructive sleep apnea syndrome associated with floppy eyelid syndrome: positive effect of CPAP therapy. Monaldi archives for chest disease = Archivio Monaldi per le malattie del torace87 1 (2017): 766 .
- ↑ Hawn VS, Cheng T, Raval N, Shrivastava A, Moon JY, Barmettler A. Ocular and eyelid changes associated with rapid weight loss after bariatric surgery: A prospective cohort analysis. Clin Exp Ophthalmol. 2023 Sep-Oct;51(7):728-730. doi: 10.1111/ceo.14266. Epub 2023 Jul 6.
- ↑ Moore MB, Harrington J, McCulley JP. Floppy eyelid syndrome. Management including surgery. Ophthalmology 1986; 93:184-8.
- ↑ Nakamoto, Deanne, and Robert Bernardino. “The Annoying Lash in the Eye: A Review of Trichiasis.” Review of Ophthalmology, 21 Nov. 2007 www.reviewofophthalmology.com/article/the-annoying-lash-in-the-eye-a-review-of-trichiasis.