Blepharoptosis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
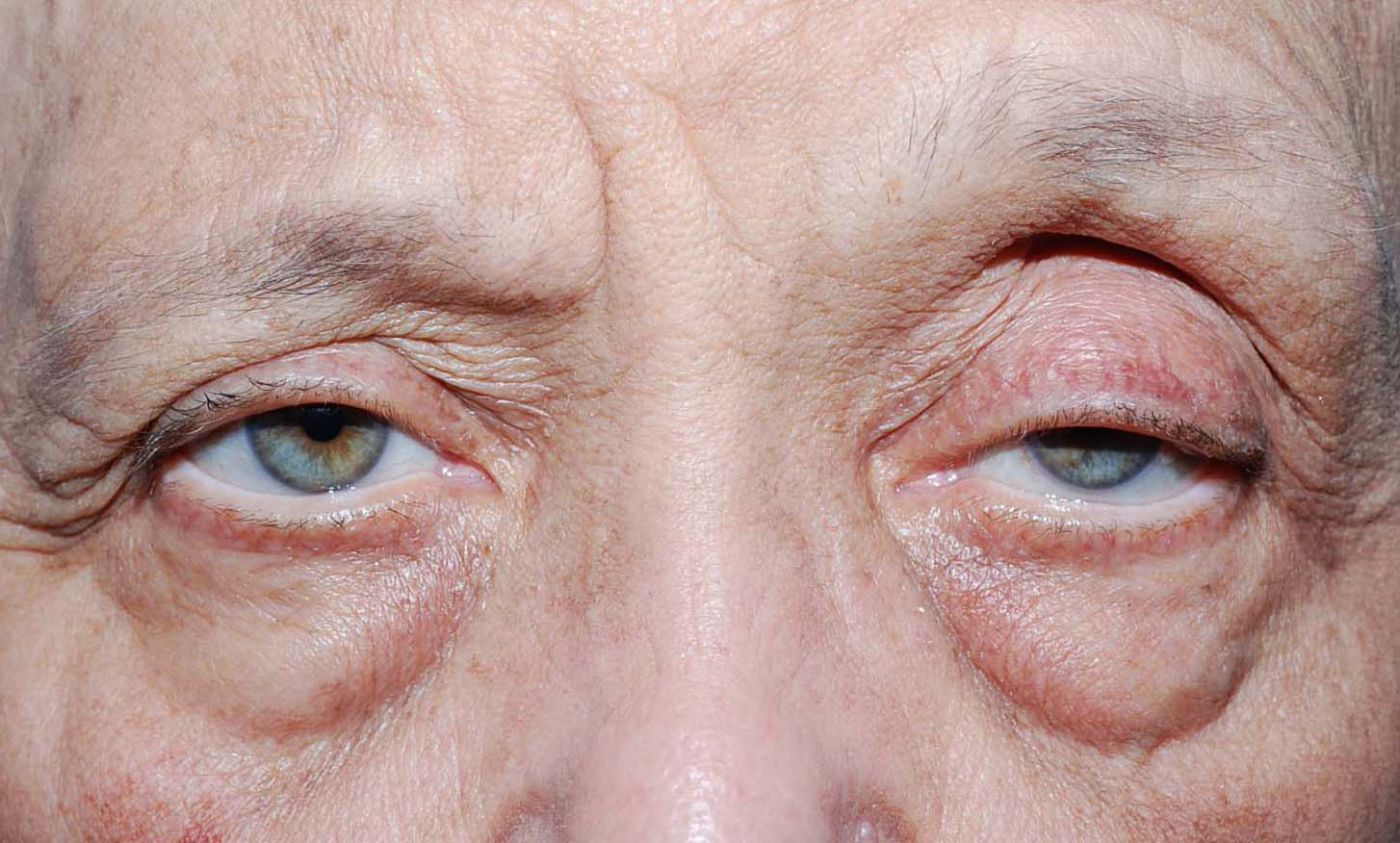
Droopy upper eyelid or ptosis presents with substantial blockage of the upper part of field of vision, risk of amblyopia among young children, and an aging change in facial appearance.
Disease Entity
Disease
Blepharoptosis is an abnormal low-lying upper eyelid margin with the eye in primary gaze. Normally, the upper lid covers 1.0-2.0mm of the superior part of the cornea. Skin redundancy of the upper lid, or dermatochalasis, is a separate finding, and may occur in conjunction with blepharoptosis. Dermatochalasis and brow ptosis should be distinguished from blepharoptosis as the surgical management differs.
Etiology
Blepharoptosis can be congenital or acquired.
Congenital ptosis usually results from isolated localized myogenic dysgenesis of the levator palpebrae superioris. A very small number of congenital blepharoptosis may result from genetic or chromosomal defects, and neurologic dysfunction.
Other causes of congenital blepharoptosis include:
- Blepharophimosis syndrome which is characterized by short palpebral fissures, congenital ptosis, epicanthus inversus, and telecanthus.
- Congenital third cranial nerve palsy.
- Congenital Horner's syndrome which is characterized by mild ptosis, miosis, anhidrosis, and heterochromia.
- Marcus Gunn jaw-winking syndrome which results from misdirected innervations to the ipsilateral levator muscle by the motor nerve to the external pterygoid muscle. Patients have lid elevation with mastication or with movement of the jaw to the opposite side.
Acquired blepharoptosis:
Most cases of acquired blepharoptosis are of aponeurotic type. Aponeurotic blepharoptosis may result from stretching, dehiscence, or disinsertion of the levator aponeurosis. Aponeurotic blepharoptosis is commonly known as involutional ptosis in patients in which the anatomic changes are age-related.
Myogenic, neurogenic, traumatic, mechanical are less frequent causes of acquired blepharoptosis:
- Myogenic blepharoptosis can be found in myasthenia gravis, chronic progressive external ophthalmoplegia, oculopharyngeal muscular dystrophy, and myotonic dystrophy.
- Neurogenic blepharoptosis may result from third nerve palsy, Horner's syndrome.
- Traumatic blepharoptosis may follow an eyelid laceration with transection of the upper eyelid elevators or disruption of the neural pathway.
- Mechanical ptosis can result from the presence of eyelid mass, such as neurofibroma or hemangioma, chalazion, or cicatrization secondary to inflammation or surgery.
Pathophysiology
Levator palpebrae superioris and Muller muscle are the upper eyelid elevator muscles.
The levator palpebrae superioris originates from orbital apex and continues anteriorly. At Whitnall's ligament, it changes direction and travels inferiorly as an aponeurosis. . The aponeurosis inserts into the anterior aspect of the tarsal plate. It also sends attachments to the skin, forming the upper eyelid crease. The levator palpebrae superioris is a striated muscle that is innervated by the superior division of the oculomotor nerve. This muscle is the major elevator of the upper eyelid.
The Muller muscle, a sympathetically innervated smooth muscle, has its origins from the undersurface of the levator superioris. Approximately 12 mm long, it inserts superiorly on the tarsal border and elevates the upper eyelid by approximately 2 mm.
Blepharoptosis results from dysfunction of one or both upper eyelid elevator muscles.
Diagnosis
History
Patients usually present with a complaint of the involved eye being small, having a tired appearance, causing limitation of the field of vision, and headache.
Acquired blepharoptosis can occur at any age, but it is commonly seen in older adults. Congenital blepharoptosis presents from birth. There is no racial or gender predilection in blepharoptosis.
More details are needed in regards to the onset of ptosis, alleviating or aggravating factors, family history of ptosis, recent botulinum injection, and history of trauma or ocular surgery. The history usually provides very good clue for the etiology of the blepharoptosis.
It is important to ask about any anticoagulant use or bleeding, a family history of malignant hyperthermia, and cardiac disorders to avoid potential complications during surgery.
Signs
Visual acuity and refractive error should be documented. Eyebrow position and presence of extra eyelid skin need to be noted. Careful external examination along with palpation of the eyelids and the orbital rim should be performed. A lid mass can cause extra weight in the lid, resulting in mechanical blepharoptosis. Before using topical eye drops, the following measurements need to be done:
- The palpebral fissure, which is the distance between the upper and lower eyelid in vertical alignment with the center of the pupil.
- The marginal reflex distance-1 (MRD-1), which is the distance between the center of the pupillary light reflex and the upper eyelid margin with the eye in primary gaze.
- The marginal reflex distance-2 (MRD-2), which is the distance between the center of the pupillary light reflex and the lower eyelid margin with the eye in primary gaze.
- Levator function, which is the distance the eyelid travel from downgaze to upgaze while the frontalis muscle is held inactive at the brow. A measurement of greater than 10 mm is considered excellent, whereas 0-5 mm is considered poor.
- Presence of eyelid crease and its height.
In patients with unilateral blepharoptosis, the involved eyelid should be lifted manually and the contralateral eyelid observed for any masked blepharoptosis or Hering phenomenon.
Patients should be examined for proptosis or enophthalmos, lagophthalmos, and presence or absence of Bell phenomenon.
Ocular motility must be evaluated as some patients may have limited ocular motility such as in myasthenia gravis and chronic progressive external ophthalmoplegia. Patients with congenital blepharoptosis need to be examined for presence of Marcus Gunn jaw-winking syndrome. The pupillary size and the iris color differences between the eyes should be examined for congenital Horner's syndrome.
It is very important to examine for presence of dry eye with fluorescein stain to examine the cornea, tear meniscus, and tear break-up time to determine if surgical intervention is safe.
Sympathomimetic eyedrops can be used to stimulate the Muller muscle. If a good response is observed, the ptosis may be repaired by Muller muscle–conjunctival resection.
Diagnostic procedures
Clinical examination is enough in majority of patients. Visual field is usually requested to show the impact of the blepharoptosis peripheral field of vision. In few patients laboratory and imaging studies are needed to find out the cause of the blepharoptosis. If myasthenia gravis is suspected, an ice pack test can be performed in the office wherein eyelid elevation yields a positive result.
Laboratory test
- Serum assay for acetylcholine receptor antibodies and an edrophonium chloride (Tensilon) test or single-fiber electromyography may be ordered for patients suspected to have myasthenia gravis
- In patients with chronic progressive external ophthalmoplegia, an electrocardiogram, electroretinogram, electromyography, and mitochondrial assay should be considered.
Diagnostic Imaging
- Patients having neurologic deficits along with blepharoptosis should undergo imaging of the brain and orbits.
- Patients suspected to have inflammatory or infiltrative orbital process as a cause of blepharoptosis should also have orbital imaging.
- In acquired Horner's syndrome, imaging of the head and neck is required, preferably an MRI.
Differential diagnosis
- Pseudoptosis, which may result from microphthalmos, enophthalmos, anophthalmos, or contralateral eyelid retraction.
- Blepharochalasis
- Brow ptosis
- Dermatochalasis
- Old facial nerve palsy resulting in narrow palpebral fissure
Management
Management of blepharoptosis is primarily surgical. Observation is only required in mild cases of congenital ptosis if no signs of amblyopia, strabismus, and abnormal head posture are present. If there is risk for amblyopia, strabismus, and substantial abnormal head posture, surgery is done as soon as possible. Blepharoptosis surgical correction can be done at any time for improving the field of vision or for cosmesis.
If blepharoptosis represents a sign of systemic disease such as myasthenia gravis and Kearns-Sayre disease, the patient should be referred to the appropriate physician for further management.
External photographic documentation is good to obtain especially before attempting surgical correction.
Medical therapy
Patients with myasthenia gravis may improve with medical treatment. Sympathomimetic topical eye drops such as apraclonidine and phenylephrine provide short temporary lift of the upper eyelid in some patients. Use of topical oxymetazoline hydrochloride (0.1%) for blepharoptosis received FDA approval in July 2020, which can last between 6 to 10 hours with each instillation.
Surgery
Surgical correction of congenital ptosis can be done at any age depending on the severity of the disease and early intervention is required if there is a risk for development of amblyopia or significant abnormal head position. Different surgical techniques are available for blepharoptosis correction. Depending on treatment goals, the underlying diagnosis, surgeon preference, and the degree of levator function, the appropriate technique is chosen. Patients should be made aware that symmetry is not easy to achieve. Great care must be taken for patients with dry eyes, decreased corneal sensation, absent Bell phenomenon, double elevator palsy, or progressive external ophthalmoplegia to avoid exposure keratopathy postoperatively. If the patient has strabismus and blepharoptosis, strabismus needs to be corrected first.
Muller muscle–conjunctival resection
This technique is appropriate for patients with mild to moderate aponeurotic blepharoptosis (these patients have very good levator function). This surgery does not work well for patients with congenital blepharoptosis. Good response to sympathomimetic topical eye drops provides a good indicator for the success of this type of surgery. This technique has the least chance of changing the eyelid contour compared with the other surgical techniques.
The surgery is done from the conjunctival side where the conjunctiva and the Muller muscle are marked (around 4mm of conjunctiva for 1mm correction of blepharoptosis from the tip of the upper tarsus), the marked conjunctiva and the Muller muscle area is clamped. Suture is passed under the clamp in continuous manner and externalized through the skin at both ends of the marked area, then, tissues above the clamp are resected.
Fasanella-Servat ptosis correction is similar in technique. However, it involves resection of conjunctiva, Muller muscle, as well as part of the upper tarsus. Including part of the tarsal plate in the resection creates a more powerful elevation. Care should be taken to avoid excessive removal of tarsus that could affect the integrity of the eyelid structure.
Levator advancement or resection
This technique involves shortening of the levator aponeurosis according to the severity of blepharoptosis. It works for patients with good and fair levator function (>5mm).
The surgery is done through an eyelid crease incision. The orbital septum is opened and preaponeroutic fat is retracted away from the levator aponeurosis. Once the muscle is identified, the levator aponeurosis is disinserted from the tarsus and dissection may be continued between levator aponeurosis and Muller muscle. Levator aponeurosis is then advanced and/or resected, and fixed temporarily with 1 to 3 sutures to the tarsus with partial thickness bites. The amount of advancement and/or resection depends on the degree of blepharoptosis. If the patient is awake, the lid height and contour are examined at this stage. Once a good height and contour are achieved, the tarsal lamellar bites are then tightened permanently. The skin is closed with incorporating part of the levator aponeurosis to reform the crease.
Frontalis suspension
This procedure is performed for patients with poor (<4 mm) or absent levator function. Many autogeneic and allogeneic materials are available be used as a sling. Fascia lata and frontalis muscle flaps, preserved (tissue bank) fascia lata, autogenous temporalis fascia, Gore-Tex suture, frozen dura mater, silicone, and Alloderm have been used. Autogeneous fascia lata was found to give the most favorable surgical result. The sling connects the eye lid with eye brow, and with the elevation of the eyebrow, the eye opens. Following surgery, patients may need several months to be able close their eyelids during sleep. Significant lubrication is needed during this period.
For patients with unilateral severe blepharoptosis, bilateral frontalis sling provide the best cosmetic outcome. However, it is often difficult to persuade the parents and the patient to perform surgery on the normal contralateral levator muscle.
For patients with Marcus Gunn jaw-winking syndrome, the surgical correction technique of jaw-winking blepharoptosis is controversial. If the jaw-winking is insignificant, blepharoptosis correction alone (with levator advancement or frontalis sling) depending on the severity of the ptosis and levator function may be enough. If the jaw-winking is significant, extirpation of the levator muscle and placement of frontalis sling may be needed.
Surgical follow up
The surgical correction of blepharoptosis is generally done as an outpatient procedure. While the patient is awake, apply cold compresses to the eyelids for 20 minutes every 1-2 hours for 2-3 days to decrease swelling and bruising. A topical antibiotic ointment (with or without a steroid) is given for the patients to be applied on the eye and the incision site twice daily for 5-7 days. For patients who are expected to have postoperative lagophthalmos, excessive lubrication is needed. Patients usually are seen 1 to 2 weeks following surgery. The patients are evaluated for signs of exposure keratopathy, infection, granuloma formation, and overcorrection and undercorrection. Patients with amblyopia need to continue amblyopia treatment.
Complications
Congenital ptosis may lead to amblyopia secondary to deprivation or uncorrected astigmatism. Acquired blepharoptosis results in decreased field of vision and frontal headaches. Blepharoptosis causes significant psychosocial effects and may lead to poor performance in school and at work.
Surgical correction of blepharoptosis may be complicated by bleeding, infection, edema, undercorrection or overcorrection of the ptosis, eyelid asymmetry, granuloma formation, corneal foreign body sensation, and exposure keratopathy. Majority of these complications can be managed easily if discovered early and the appropriate treatment provided.
Prognosis
Good results are usually achieved by the medical and surgical approaches availabe for managing blepharoptosis. Recurrence over time is not uncommon. More than one surgery may be needed to achieve this result, especially in congenital ptosis.
Additional Resources
- Boyd K, DeAngelis KD. Ptosis. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/ptosis-list. Accessed March 22, 2019.
References
- Baldwin HC, Manners RM. Congenital blepharoptosis: a literature review of the histology of levator palpebrae superioris muscle. Ophthal Plast Reconstr Surg. 2002;18:301-7
- Sakol PJ, Mannor G, Massaro BM. Congenital and acquired blepharoptosis. Curr Opin Ophthalmol. 1999;10:335-9.
- Cetinkaya A, Brannan PA. Ptosis repair options and algorithm. Curr Opin Ophthalmol. 2008;19:428-34.
- Small RG. The surgical treatment of unilateral severe congenital blepharoptosis: the controversy continues. Ophthal Plast Reconstr Surg. 2000;16:81-2.
- Baroody M, Holds JB, Vick VL. Advances in the diagnosis and treatment of ptosis. Curr Opin Ophthalmol. 2005;16:351-5.
- Frueh BR, Musch DC, McDonald HM. Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology. 2004;111:2158-63.
- Baldwin HC, Manners RM. Congenital blepharoptosis: a literature review of the histology of levator palpebrae superioris muscle. Ophthal Plast Reconstr Surg. 2002;18:301-7.
- Lee MJ, Oh JY, Choung HK, Kim NJ, Sung MS, Khwarg SI. Frontalis sling operation using silicone rod compared with preserved fascia lata for congenital ptosis a three-year follow-up study. Ophthalmology. 2009;116:123-9.
- Dallalzadeh LO, Park KS, Korn BS, Kikkawa DO, Liu CY. Minimal Dissection Direct Frontalis Muscle Advancement Flap for Congenital Ptosis Repair. J Craniofac Surg. 2021 Oct 1;32(7):2358-2361. doi: 10.1097/SCS.0000000000007761. PMID: 34054081.