Drug-Induced Corneal Complications
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Drug-induced corneal complications can be categorized by histological layer:
- Epithelial
- Stromal
- Endothelial
Drug classes include:
- anti-biotic
- anti-malarial
- anti-inflammatory
- anti-psychotic
- anti-arrhythmic
- anti-estrogenic
Pathogenesis
While topically administered drugs have a direct effect on corneal layers, systemically-administered drugs reach the cornea via the tear film, aqueous humor, and limbal vasculature and cause complications. Pathology is caused by deposition or direct cytotoxicity. Manifestation of corneal disease may foreshadow that of retinal disease.[1]
Epithelial
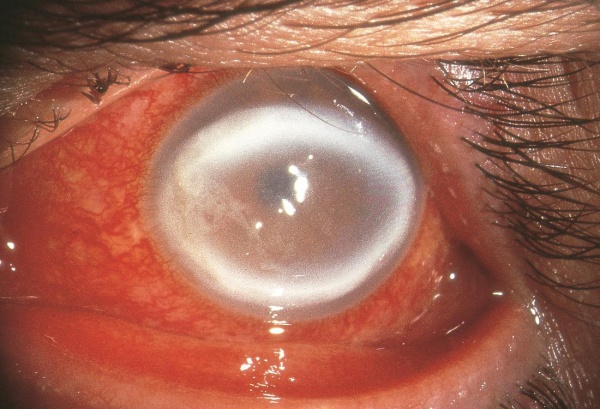
Vortex keratopathy (Cornea verticillata/whorl keratopathy/Fleischer vortex)
Drugs associated with vortex keratopathy:
- Amiodarone (class III antiarrhythmic drug)
- Effects 98% of patients on doses 200-300 mg a day or greater.[2]
- bilaterally with whorled, golden-brown deposits on the cornea
- In vivo confocal microscopy has shown hyperreflective cells in the epithelial layer of the cornea in patients taking amiodarone.
- Cornea clears 3-20 months after cessation.[2]
- Aminoquinolones (chloroquine, hydroxychloroquine, amodiaquine, quinacrine, tafenoquine)
- Presents weeks to months after starting medication. Occurs in 93% of patients on tafenoquine[2].
- This drug also causes maculopathy.[2]
- Atovaquone
- Clofazimine
- Gentamicin (Subconjunctival)
- Gold
- Ibuprofen
- Indomethacin
- Mepacrine
- Monobenzone (topical skin ointment)
- Naproxen
- Perhexiline maleate
- Associated with papilledema.[3]
- Phenothiazines
- Uncommon, more likely to develop stromal deposits.[2]
- Suramin
- 33% of patients on high doses.[2]
- Tamoxifen
- Tilorone hydrochloride
- Associated with retinal toxicity (maculopathy, peripheral retina pigmentation, arteriolar narrowing, peripheral visual field defect).[3]
Epithelial cysts
Cytarabine can cause degeneration of basal epithelial cells resulting in the formation of microcysts.[1] Resolution occurs 4 weeks after stopping drug.[2]
Topical Anesthetic Abuse Keratopathy
Topical anesthetics prevent migration and division of epithelial cells, damage microvilli, and disrupt cellular-adherence.[2]
Netarsudil-associated Corneal Epithelial Edema
Rho-associated protein kinase inhibitor used for reduction of elevated intraocular pressure can cause bullae in the corneal epithelium and often presents in a reticular pattern. Etiology remains unclear, but a change in the structure of corneal epithelial cells (CEC) and arrangements of cytoskeleton has been suggested in some studies. Usually, epithelial edema is been reported to resolve within 2-4 weeks of discontinuation of this medication. [4]
Stromal
Corneal stromal deposition can occur via the aqueous humor, limbal vasculature, and tear film. Deposits may be pigmented, refractile, or crystalline.[1]
- Clofazimine
- Gold (chrysiasis)
- Immunoglobulins (exogenous)
- Indomethacin
- Phenothiazines
- Corneal deposits typically appear after deposition in the anterior lens capsule.[2]
- Retinoids (Isoretinoin)
- Fine, diffuse gray deposits in the superficial stroma centrally and peripherally.[1]
- Silver (Argyrosis)
Pigmentary deposition
Phenothiazines (chlorpromazine, thioridazine)
Chrysiasis
Systemic administration of gold salts can result in gold deposits predominantly in the posterior stroma. Deposits can disappear within months of cessation or persist for years . The deposits are both intracellular and extracellular and are not associated with inflammation.[1]
Crystalline deposition
Typically seen in paraglobulinemia, can also be seen with exogenous immunoglobin administration.[1] Appears as mid-stromal crystalline deposits in an annular pattern in the midperiphery.[1]
Endothelial
Endothelial deposits
Stellate, refractile endothelial deposits are associated with rifabutin.[1] Pathogenesis is attributed to high lipid solubility. It accumulates in aqueous humor and undergoes trans-endothelial transport.[2]
Deposition Chart
Depositional disease categorized by corneal layer.[2]
| Epithelial | Stromal | Endothelial |
|---|---|---|
| Amiodarone | Chlorpromazine | Chlorpromazine |
| Suramin | Rifabutin | Rifabutin |
| Chlorpromazine | Gold | |
| Tamoxifen | Indomethacin | |
| Gold | Clofazimine | |
| Clarithromycin | Isotretinoin | |
| Vandetanib | Vandetanib | |
| Osimertinib | ||
| Cytarabine | ||
| Belantamab mafodotin | ||
| Fluoroquinolones | ||
| Antimalarial | ||
| NSAIDs |
See Also
Drug-induced Acute Angle Closure Glaucoma
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Hollander DA, Aldave AJ. Drug-induced corneal complications. Curr Opin Ophthalmol. 2004 Dec;15(6):541-8. doi: 10.1097/01.icu.0000143688.45232.15. PMID: 15523201.
- ↑ Jump up to: 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Sahyoun J, Sabeti S, Robert M. Drug-induced corneal deposits: an up-to-date review. BMJ Open Ophthalmology 2022;7:e000943. doi: 10.1136/bmjophth-2021-000943
- ↑ Jump up to: 3.0 3.1 Raizman MB, Hamrah P, Holland EJ, Kim T, Mah FS, Rapuano CJ, Ulrich RG. Drug-induced corneal epithelial changes. Surv Ophthalmol. 2017 May-Jun;62(3):286-301. doi: 10.1016/j.survophthal.2016.11.008. Epub 2016 Nov 24. PMID: 27890620.
- ↑ Wisely CE, Liu KC, Gupta D, Carlson AN, Asrani SG, Kim T. Reticular Bullous Epithelial Edema in Corneas Treated with Netarsudil: A Case Series. Am J Ophthalmol. 2020;217:20-26.