Topical Anesthetic Abuse Keratopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
History
Carl Koller was the first to use local, topical, ophthalmic anesthesia. In 1884, he was a junior intern at the Vienna Clinic of Ophthalmology and after reading Sigmund Freud's paper "Ueber Coca" and swallowing cocaine, he came to the realization that the same substance that numbed his tongue might numb his eye. Based on this idea, he developed an aqueous solution of cocaine that was tested first on an animal's cornea and then, on himself and a friend.[1]
Disease
Topical anesthetic abuse is one of the most frequent and destructive forms of self-induced ocular injury. It can be iatrogenic, since these agents are occasionally supplied by primary care physicians, emergency room physicians, optometrists, and ophthalmologists. Also, topical anesthetic abuse may present as part of addictive behavior, going as extreme as applying cocaine powder directly in the eye. In addition, some of these patients may be associated in some way to the medical profession, with easy access to the agent and/or present psychiatric illness.
Today, the most common topical anesthetics used are tetracaine, lidocaine, proparacaine, and oxybuprocaine.
Mechanism of action
Topical anesthetics can be classified as amide or ester compounds depending on their molecular composition. These compounds block sodium channels inside the nerve cells, reducing influx. Consequently, threshold potential can not be reached and action potential is prevented, stopping neural conduction along axons and dendrites.[2]
Risk Factors
- Addictive behavior
- Easy access to medication
- Availability of over-the-counter medication
- Psychiatric illness
- Topical anesthetic prescription after refractive surgery
Local effects on the corneal surface
Anesthetic agents inhibit the intrinsic characteristics of epithelial cells to migrate and divide, damaging vinculin and actin filaments through a calmodulin-mediated mechanism.[3]
Morphological changes seen by electron microscopy include loss of microvilli, anesthetic deposits on microvilli and/or cell membranes and increased desquamation. Animal models have shown a reduced number of desmosomes and an increased tendency for cell rupture. Some authors have also reported similar morphological alterations to the corneal stroma and endothelium as well.[4]
Preservatives in topical anesthetics, such as benzalkonium chloride, may also contribute to ocular surface toxicity.

Clinical features
The first clinical sign usually is an epithelial defect over a non-inflammatory stroma.[6]
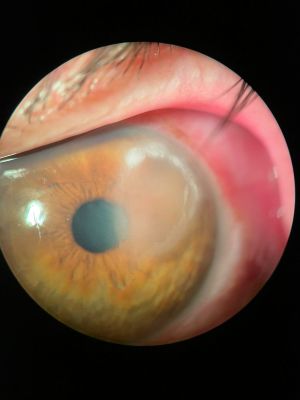
In the setting of abuse, topical anesthetics have been associated with persistent epithelial defects, conjunctival injection, stromal edema, stromal infiltrates (classic ring infiltrates), Descemet membrane folds, endothelial damage and ocular inflammation with possible hypopyon. Corneal damage, if persistent, may incur the need of a keratoplasty with the risk of vision loss.
Diagnosis
Early diagnosis of topical anesthetic abuse, more often than not, leads to better outcomes. A high index of suspicion is recommended, especially noting that these patients are frequently treated as Acanthamoeba keratitis. And similar to the latter, patients that have topical anesthetic abuse keratopathy report pain that is disproportionate to clinical findings, comparable slit-lamp findings and a non-responsiveness to antibiotics.
Since these patients commonly present with corneal infiltrates and ocular inflammation, infectious keratitis must be ruled out with appropriate corneal scrapings, culture and empiric antibiotics.
Differential diagnosis
- Acanthamoeba keratitis
- Bacterial keratitis
- Fungal keratitis
- Herpetic keratitis
Management
- It is of paramount importance to stop topical anesthetic use and other eye drops if any to stop toxicity to the ocular surface.
- Alternatives to subdue pain are oral analgesics and/or regional anesthesia (peribulbar, retrobulbar, sub-Tenon's injections).
- Evaluate hospitalization.
- Discard concomitant infectious keratitis.
- Evaluate the need for psychiatric consult.
- Topical steroids are rarely necessary, and may cause further corneal thinning.
- Education for primary care physicians, optometrists and pharmacists concerning the toxicity of these drops and their abuse potential is a key element of primary prevention.
Additional Resources
- Krachmer JH, Mannis MJ, Holland EJ. Cornea. Philadelphia: Elsevier; 2017.
References
- ↑ Goerig, M., Bacon, D., & van Zundert, A. (2012). Carl Koller, Cocaine, and Local Anesthesia. Regional Anesthesia and Pain Medicine, 37(3), 318–324. doi:10.1097/aap.0b013e31825051f3
- ↑ McGee H, Fraunfelder F. Toxicities of topical ophthalmic anesthetics. Expert Opin Drug Safe 2007;6(6):637-40
- ↑ Rosenwasser GO, Holland S, Pflugfelder SC, et al. Topical anesthetic abuse. Ophthalmology 1990; 97: 967-975.
- ↑ Risco JM, Millar LC. Ultrastructural alterations in the endothelium in a patient with topical anesthetic abuse keratopathy. Ophthalmology. 1992;99(4):629–633.
- ↑ 2020 American Academy of Ophthalmology. Image courtesy of Kirk R. Wilhelmus, MD. From https://www.aao.org/image/topical-anesthetic-overuse.
- ↑ Pharmakakis, N. M., Katsimpris, J. M., Melachrinou, M. P., & Koliopoulos, J. X. (2002). Corneal Complications following Abuse of Topical Anesthetics. European Journal of Ophthalmology, 12(5), 373–378. doi:10.1177/112067210201200505