Brow Ptosis and Repair
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Brow ptosis is decent of the brow and brow fat pad and typically occurs with advancing age or prior trauma. It may also be a result of facial nerve palsy with weak frontalis elevation.
Disease
Brow ptosis occurs secondary to descent of the periorbital soft tissues of the brow and is commonly seen associated with upper eyelid dermatochalasis or ptosis.
Etiology and Pathophysiology
Most cases of brow ptosis occur secondary to involutional changes from descent and deflation of the periorbital soft tissues and soft tissues of the face. Typically, this manifests in the temporal 1/3 of the brow first. The frontalis muscle is responsible for elevating the eye brow. The frontalis is innervated by the frontal branch of the facial nerve. The frontalis muscle is responsible for elevating the medial 2/3 of the brow and with age, collagen laxity, and descent of the periorbital soft tissues, patients develop temporal brow droop.
Brow ptosis may also occur secondary to paralysis or weakness of the frontalis muscle.
- Facial nerve palsy- Bell’s palsy, Acoustic Neuroma, Surgical trauma, Birth trauma, Congenital
- Myasthenia gravis
- Myotonic dystrophy
- Oculopharyngeal muscular dystrophy
Brow ptosis may also occur from involuntary contraction of the orbicularis oculi, pulling the brow down.
- Blepharospasm
- Facial dystonias
Finally, a mechanical etiology may result in descent of the brow
- Neoplasm:
- Basal cell carcinoma
- Squamous cell carcinoma
- Keratoacanthoma
- Melanoma
Diagnosis
History
All patients presenting with droopy upper eyelids or brows should undergo a thorough medical and family history.
- A history of fluctuating symptoms or fatiguability may indicate a history of myasthenia gravis
- A history of slowly progressive onset of symptoms with a positive family history may indicate myotonic dystrophy or oculopharyngeal dystrophy
- A history of trauma may indicate injury to the frontal nerve
- A history, even if remote, of Bell’s palsy may indicate facial nerve weakness or paralysis
- A history of Acoustic Neuroma, head trauma, tumor or stroke may indicate facial nerve paralysis
Physical Examination
All patients should undergo a complete Ophthalmic plastics examination.
- Visual acuity, pupillary examination, extraocular motility
- Cranial nerve examination including facial nerve function; presence or absence of Bell’s phenomenon
- MRD1- height of the upper eyelid margin from the pupillary light reflex
- It should be noted if skin is resting on lashes
- The brow position should be noted with the frontalis relaxed- the position should be noted if the brow is at or below the superior orbital rim
- The presence of prominent dynamic and static rhytids in the forehead should be noted as this may influence incision placement
- The location of the hairline- high or low and whether the patient wears bangs should be noted as this may influence the decision of endoscopic vs. pretricheal forehead lift
- If paralytic brow ptosis is suspected, evaluate for aberrant regeneration, or signs of previous trauma- scarring, etc.
It is important to note that all patients with dermatochalasis and ptosis should be evaluated for concomitant brow ptosis. All patients considering blepharoplasty should be evaluated for brow repositioning surgery and their brow ptosis should be treated concomitantly if necessary.
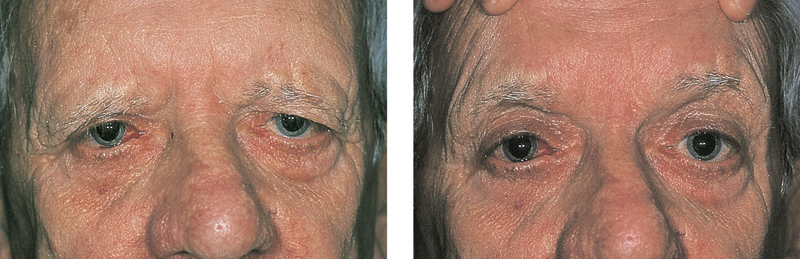
Signs
The normal eyebrow sits at or above the superior orbital rim. Male eyebrows tend to be lower and flatter than female eyebrows. The signs of brow ptosis consist of brows at or below the superior orbital rim. As discussed, patients typically have more temporal brow droop than medial brow droop. Prominent brow ptosis may give the appearance of significant dermatochalasis. If the brow is stabilized and lifted into appropriate position manually, the clinician can differentiate true dermatochalasis from that confounded by brow ptosis.
Clinical diagnosis
Patients may present with a decrease in their peripheral field, with difficulty while reading or with driving. They may complain of tension headache from prolonged frontalis contraction that typically worsens with prolonged activity such as reading or computer work. Patients may note that they see their eyelashes in their central vision.
Diagnostic procedures
Insurance companies require visual field documentation with taped and untaped visual fields to demonstrate peripheral field loss. We prefer to use a Goldman Visual Field. They may also require external photographs in primary position and 45 degrees from the right and left to illustrate the brow resting below the superior orbital rim.
Laboratory test
Not applicable
Differential diagnosis
The differential diagnosis for brow ptosis includes dermatochalasis, upper eyelid ptosis, facial nerve palsy or mechanical ptosis secondary to mass.
Management
General treatment
The treatment of brow ptosis is surgical.
Surgery
Several approaches have been utilized in the treatment of brow ptosis. All patients to avoid Aspirin for at least 10-14 days prior to the scheduled surgery. Non-steroidal anti-inflammatory agents and platelet inhibitors (ie. Plavix, Aggrenox, Pletal) should be avoid for at least 5-7 days prior to surgery.
Procedures that lift the temporal portion of the brow:
Direct temporal browplasty
Patients with a predominant temporal droop may be treated with temporal direct browplasty with incision placement over the lateral 2/3 of the brow hairs. This procedure is optimally used in patients with a static or dynamic rhytid that may be used to camoflauge the incision line over the lateral 2/3 of the brow.
Indirect (Internal) browpexy
An alternative procedure that has waxed and waned in popularity and insurance coverage is the indirect browpexy. This procedure is performed through an eyelid crease incision and is performed simultaneously to an upper eyelid blepharoplasty. Preseptal dissection is performed to the superior orbital rim where the periosteum is exposed. The brow fat pad is sutured, with absorbable or nonabsorbable sutures, to the periosteum approximately 1 centimeter above the superior orbital rim. Alternatively, dissolvable implants have been used in the past (such as Endotines) through this approach to secure the brow fat pad to the frontal bone.
Temporal brow lift (endoscopic or open)
If only the temporal portion of the brows needs elevation and the patient desires cosmesis with an incision hidden within the hair, a temporal brow lift may be considered. This procedure has been described by Massry et. al. Temporal incisions are made posterior to the hairline extending approximately 2-4cm in length, and dissection is carried out in the same manner as the endoscopic brow lift (see below for details). The central incisions associated with a full endoscopic brow lift are not made in this approach. There is a risk of facial nerve injury with this approach.
Procedures that lift the entire brow:
Direct browplasty
Patients with temporal and medial brow ptosis and static rhytids that would allow incision camouflage would benefit from complete direct brow plasty across the entire length of the brow with more lift performed temporally than medially. Careful dissection over the medial 1/3 of the brow is necessary to avoid injury to the superior orbital neurovascular bundle.
Mid forehead lift
Patients with prominent static and dynamic rhytids may benefit from a median forehead lift. Using a similar technique to the direct browplasty, the mid forehead lift utilizes the existing rhytids to camouflage the incision line. However, this may not be an acceptable scar for some patients and should be discussed with the patient prior to surgery.
Pretricheal/Posttricheal forehead lift
The coronal forehead lift is an optimal procedure for patients that prefer to minimize scarring at the brow or on the forehead with a relatively long forehead. In this procedure, the surgeon places the incision line at the hairline or behind the hairline for more of a concealed incision. The incision can be beveled to minimize visibility and avoid damage to the hair follicles. Patients must be warned that they will experience numbness of the scalp because the neurovascular bundles are sacrificed with this procedure.
Endoscopic forehead lift
Patients wishing to avoid visible scarring and require a complete brow lift benefit from an Endoscopic forehead lift. Five incision are made perpendicular to the brow, one incision centrally, one incision corresponding to the lateral 2/3 of the brow on each side and one incision corresponding centered in line with the ala, lateral canthus and tail of the brow. Dissection is carried out in the subperiosteal plane and just anterior to the deep temporalis fascia. An endoscope is used to allow direct visualization at the superior orbital neurovascular bundles and 1 centimeter above the temporal brow in the location of the sentinel vein and facial nerve. Patients undergoing endoscopic forehead lift may experience temporary numbness and tingling of the forehead, secondary to stretching of the neurovascular bundle as well as potential permanent or temporary damage to the facial nerve resulting in a paralytic brow.
Surgical follow up
Permanent monofilament sutures are typically used for wound closure of all browplasty incisions that are visible on the forehead or pretricheal region. Surgical staples may be used for closure of the endoscopic forehead lift wounds. Patients undergoing forehead lift procedures typically wear a head wrap to prevent hematoma formation. Patients are seen in follow-up for suture and staple removal at 1 week and again 4-6 weeks after surgery. Blood thinning medications may be restarted 1 day postoperatively.
Complications
Surgical complications are relatively uncommon however, include bleeding, numbness and tingling, injury to the facial nerve resulting in paralytic brow ptosis, infection and postoperative asymmetry.
Prognosis
The prognosis for successful treatment with surgical management is excellent. The patient’s expectations regarding incision location and postoperative recovery should be explored in order to ensure patient satisfaction.
Additional Resources
- ASOPRS Information on Eyebrow and Forehead Lift
- Boyd K, DeAngelis KD. Ptosis. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/ptosis-list. Accessed March 27, 2019.
References
- Nerad, JA. Techniques in Ophthalmic Plastic Surgery pp. 140-150, 177-187 Elsevier 2009