Acquired Oculomotor Nerve Palsy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
An acquired oculomotor nerve palsy (OMP) results from damage to the third cranial nerve. It can present in different ways causing somatic extraocular muscle dysfunction (superior, inferior, and medial recti; inferior oblique; and levator palpebrae superioris) and autonomic (pupillary sphincter and ciliary) muscles. [1]
Disease Entity
Partial and complete 3rd nerve palsy
Disease
Clinical findings of an acquired third nerve palsy depend on the affected area of the oculomotor nerve pathway. It can be divided into a partial or complete palsy. A complete third nerve palsy presents with complete ptosis, with the eye positioned downward and outward with the inability to adduct, infraduct, or supraduct, as well as a dilated pupil with sluggish reaction.[2] A partial third nerve palsy may be more common, and can present with variable duction limitation of the affected extraocular muscles and with variable degrees of ptosis and/or pupillary dysfunction. [1]
Etiology
There are many etiologies for oculomotor palsy including a vasculopathic process, trauma, compression (e.g. aneurysm), infiltrative (e.g. leukemia), toxic (e.g. chemotherapy) etc.
Risk Factors
Risk factors may coincide with the potential underlying etiologies listed above and can include diabetes mellitus, hypertension, vasculitis, trauma, infections, tumor, aneurysm etc.
General Pathology
The manifestations may depending on the location of the lesion. In some cases, the precise site of the lesion is clear, whereas in others, the location of the lesion is speculative.[1]
Pathophysiology
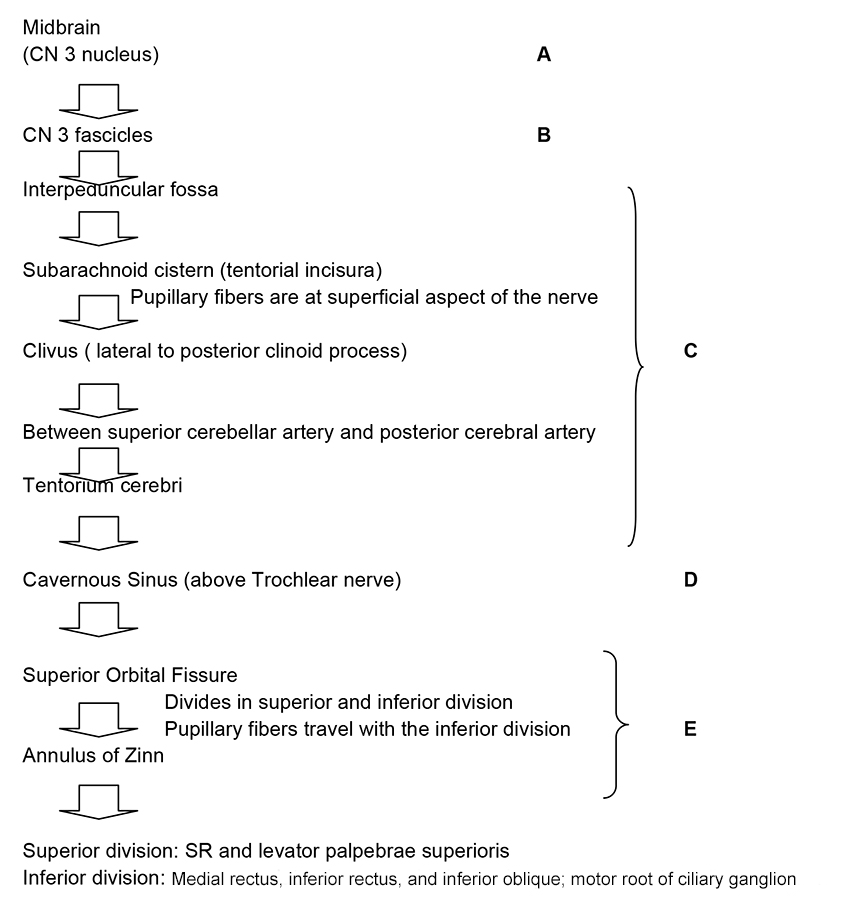
To understand the pathophysiology of the oculomotor nerve palsy it is essential to know its pathway. The following flowchart represents the anatomic course of cranial nerve III with a designated description of clinical manifestations
Lesions of Oculomotor Nucleus (Midbrain)
Usually produce bilateral defects. This is explained by the anatomy of the nucleus. It is divided into subnuclei according to the innervated area. Each of the superior recti (SR) muscles are innervated by the contralateral CN III subnucleus; therefore a nuclear CN III palsy would produce paralysis of the contralateral SR. Both levator palpebrae superioris are innervated by one subnucleus (central caudal nucleus); therefore a central caudal nuclear lesion would produce bilateral ptosis. Patients with damage to the oculomotor nuclear complex need not have ipsilateral pupillary dilation, but when involved, it may indicate dorsal rostral damage.[1] often caused by ischemia, usually from embolic or thrombotic occlusion of small, dorsal perforating branches of the mesencephalic portion of the basilar artery.[1]
Lesions of Oculomotor Nerve Fascicles (Leaving the 3rd nerve nucleus)
Lesions at this level can produce complete or incomplete palsies. The majority of the time it cannot be differentiated from lesion outside of the midbrain. When the lesion is adjacent to the CN III nucleus (midbrain) it can produce several manifestations that have been described according to other neurological manifestations. Lesions at the superior cerebellar peduncle (Nothnagel’s Syndrome) presents with ipsilateral 3rd nerve palsy and cerebellar ataxia. Lesions at the Red Nucleus (Benedikt's Syndrome) are characterized by ipsilateral 3rd nerve palsy and contralateral involuntary movement. Lesions at the Red Nucleus and superior cerebellar peduncle (Claude Syndrome) presents with ipsilateral 3rd nerve palsy, contralateral ataxia, asynergy and tremor. Lesions at the cerebral peduncle (Weber’s Syndrome) produces ipsilateral 3rd nerve palsy and contralateral hemiplegia. It is important to remember that lesions can present a combination of these findings depending on the degree of the insult. In addition, although it is known that CN III separates into superior and inferior rami at the superior orbital fissure, sometimes lesions at the fascicles can produce isolated dysfunction of either the superior and inferior division.[1] The most common causes include ischemic, hemorrhagic, compressive, infiltrative, traumatic, and rarely, infiltrative and demyelinating process.
Lesions in the Subarachnoid space
This space is defined as the area traveled by the oculomotor nerve between the ventral surfaces of the midbrain to the entrance of the cavernous sinus, also known as the interpeduncular fossa. Oculomotor nerve damage in this area can produce varied presentations. CN III palsy with fixed dilated pupil, it is important to recall that pupillary fibers occupy a peripheral location and receive more collateral blood supply that the main trunk of the nerve.[1] This is why they are susceptible to compression (e.g. aneurysm). The most common known etiology is a posterior communicating artery aneurysm. This is a medical emergency. CN III palsy without pupil involvement, as mentioned above pupillary fibers occupy a peripheral location and receive more collateral blood supply than the main trunk of the nerve.[1] For this reason, they are less susceptible to ischemia.. This is why in most of the cases patients have diabetes mellitus, systemic hypertension, atherosclerosis and in some cases migraine. Nevertheless, compressive masses or aneurysm can also cause it. On the course to the cavernous sinus the CN III rests on the edge of the tentorium cerebelli. The edge of the uncal portion overlies the tentorium. For this reason, in the setting of increased intracranial pressure this brain section can herniate producing displacement of the midbrain compressing the ipsilateral oculomotor nerve. This causes ipsilateral ophthalmoplegia and mydriasis. The most common cause of uncal herniation is intracranial hemorrhages.
Lesions within the Cavernous Sinus and Superior Orbital Fissure
Lesions at these zones can produce an isolated CN III palsy, but it is most commonly associated with other cranial nerves dysfunctions. Differentiating between lesions at the cavernous sinus versus the superior orbital fissure can be challenging and sometimes the literature describes it as sphenocavernous syndrome. It presents as paresis of the oculomotor, trochlear and abducens nerves with the associated maxillary division of trigeminal nerve, producing pain. This can be caused by primary (direct invasion) or secondary (intracranial/intraorbital lesion compressing these areas) lesions. The most common cause is a tumor (e.g. meningiomas). Tolosa Hunt Syndrome is another pathology within the cavernous sinus and superior orbital fissure that presents with painful ophthalmoplegia. It is described as an idiopathic granulomatous inflammation. This is a diagnosis of exclusion, therefore tumors, metastasis or aneurysm must be ruled out with neuroimaging. Although tumors are the most common causes of lesions in this area, vascular processes can also produce damage. Cavernous sinus thrombosis, carotid cavernous fistulas, syphilis, vasculitis, and/or autoimmune connective tissue diseases (e.g. systemic lupus erythematosus) can produce pain typical of cavernous sinus syndrome.[1]
Lesions within the Orbit
Lesions within the orbit are associated with visual loss, ophthalmoplegia, and proptosis. Third nerve ophthalmoplegia can be associated with trochlear and abducens nerve palsies. It is important to remember that at the orbit the oculomotor nerve divides into superior and inferior division. This can cause partial oculomotor nerve palsies. Most common etiologies: trauma, masses, inflammation, and/or infiltrative processes.
Primary Prevention
Although there are many risk factors, some of them can be controlled to minimize the risk of acquiring oculomotor nerve palsy. It is encouraged to maintain blood pressure and glycemic control which are the most common causes of vasculopathic third nerve palsy.
Diagnosis
Acquired oculomotor nerve palsy is a clinical diagnosis.
History
The most common ocular manifestations are diplopia and ptosis. In addition, depending on affected section of the third cranial nerve track it can also produce other neurologic manifestations as involuntary movements, hemiplegia, and altered mental status.
Physical Examination
Consist on complete ophthalmic exam including visual acuity, ductions and versions, levator function, pupils reaction to light and to accommodation. In addition, general physical and/or neurological evaluation should be consider.
Signs
The presenting signs depend on the affected area of 3rd nerve track. In some cases, the precise site of the lesion is clear, whereas in others, the location of the lesion is speculative. It can present in different ways causing somatic extraocular muscle dysfunction (superior, inferior, and medial recti; inferior oblique; and levator palpebrae superioris) and autonomic (pupillary sphincter and ciliary) muscles.[2]
Symptoms
Symptoms depend on the location of the lesion. The most common ocular complaint is diplopia secondary to somatic extraocular muscle dysfunction, but pain and ptosis can also me present.
Clinical Diagnosis
Diagnosis is made by physical examination.
Diagnostic procedures
Acquired oculomotor nerve palsy can be secondary to many etiologies. Nevertheless, neuroimaging is usually done if intracranial pathology is suspected. In a conscious patient presenting with ophthalmoplegia, ptosis and mydriasis a compressive etiology, as an intracranial aneurysm, must be ruled out. If an intracranial aneurysm is suspected, a computed tomography angiography (CTA) and/or magnetic resonance imaging (MRI and MRA) should be performed, with a 90% sensitivity in aneurysms of 3mm or greater in diameter, although the gold standard is digital subtraction angiography (DSA).
Laboratory test
If a patient presents with complete oculomotor nerve palsy without pupil involvement it is most likely to be related to an ischemic process, but compression and inflammation should also be considered. Evaluation and management will vary according to patient’s systemic illnesses, age, and associated symptoms. Nevertheless, basic workup is recommended. This may include the following: vital signs (e.g. blood pressure), complete blood count (CBC), sedimentation rate (ESR), C-reactive protein (CRP) comprehensive metabolic panel (CMP). Covid-19 testing may also be indicated. Central nervous system imaging (MRI or CT) and angiographic studies (MRA, CTA or catheter angiogram) can be used to rule out acute intracranial pathology, especially if ophthalmoplegia is associated with pain. [1] .
Differential diagnosis
- Myasthenia Gravis
- Thyroid associated orbitopathy
- Internuclear ophthalmoplegia
- Chronic progressive external ophthalmoplegia
- Orbital pseudotumor
- Giant cell arteritis
Management
Acquired oculomotor nerve palsy evaluation depends on signs and symptoms, patient’s age and systemic diseases. Management depends on the presented scenarios. In a conscious patient presenting with ophthalmoplegia, ptosis and mydriasis a compressive etiology, as an intracranial aneurysm, must be ruled out. On the other hand if a patient presents with complete oculomotor nerve palsy without pupil involvement it is most likely to be related to an ischemic process, but compression and inflammation should also be considered. The majority of complete or incomplete CN III palsies without pupil involvement are secondary to an ischemic process. These patients observe an improvement after the first 4 weeks with full resolution in 12 weeks of the insult.[3] Those patients that are left with a residual deficit can consider prisms or strabismus surgery after 6 months of stability. In these cases the main goal of strabismus surgery is to provide alignment in primary and reading position.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Miller, N and Newman, N. Clinical neuro-ophthalmology 5th edition. P. 1194-1223
- ↑ Jump up to: 2.0 2.1 American Academy of Ophthalmology. Basic and Clinical Science Course. Section 5: Neuro-Ophthalmology, Chapter 8 The patient with diplopia. P.228-229 2010-2011.
- ↑ Capo, H., M.D., Warren, F., M.D., Kupersmith, M. , M.D. Evolution of Oculomotor Nerve Palsies. Journal of Clincal Neuro-ophathalmology (12)1:21-25, 1992.
- Kline, Lanning B. Neuro-Opthalmology. 6th edition. P. 95-105
- Kaiser, Peter. MD., Friedman, Neil. MD., Pineda, Roberto. MD. Third cranial nerve palsy. The Massachusetts eye and ear infirmary Illustrated manual of Ophthalmology. 2nd edition. P. 39-41
- Bhatt, VR. Naqi, M. Bartaula R., Murukutla S., Misra, S. Popalzai, M., Paramanathan, K. Dai, Q. T cell acute lymphoblastic leukaemia presemting with sudden onset right oculomotor nerve palsy with normal neuroradiography and cerebrospinal fluid. BMJ Case Rep. 2012 Mar 27;2012.
- Appenzeller S, Veilleux, M. Clarke, A. Lupus. Third cranial nerve palsy or pseudo 3rd nerve palsy of myasthenia gravis? A challenging diagnosis in systemic lupus erythematosus. 2009 Lupus. Aug;18(9):836-40.
- Chaudhary,N. et al Imaging of Intracranial Aneurysms Causing Isolated Third Nerve Palsy. J. Neuro-Ophthalmol 2009;29:238-244 (8) Trobe,J. Searching for Brain Aneurism in Third Cranial Nerve Palsy. J Neuro-Ophthalmol vol. 29,No.3,2009 pg.171-3
- Douedi S, Naser H, Mazahir U, Hamad AI, Sedarous M. Third Cranial Nerve Palsy Due to COVID-19 Infection. Cureus. 2021;13(4):e14280. Published 2021 Apr 3. doi:10.7759/cureus.14280
- Belghmaidi S, Nassih H, Boutgayout S, et al. Third Cranial Nerve Palsy Presenting with Unilateral Diplopia and Strabismus in a 24-Year-Old Woman with COVID-19. Am J Case Rep. 2020;21:e925897. Published 2020 Oct 15. doi:10.12659/AJCR.925897