Endoscopic Brow Lift: Difference between revisions
No edit summary |
No edit summary |
||
| (29 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{Article | {{Article | ||
|Authors=Michael.Bouaziz | |Authors=Anne.Barmettler, Michael.Bouaziz | ||
|Category=Oculoplastics/Orbit | |Category=Oculoplastics/Orbit | ||
|Date reviewed=October | |Assigned editor=Anne.Barmettler | ||
|Reviewer=Anne.Barmettler | |||
|Date reviewed=October 1, 2024 | |||
|Article status=Up to Date | |||
|Meta description=The history, procedure, and advantages of the endoscopic brow lift are discussed in detail in this article. | |Meta description=The history, procedure, and advantages of the endoscopic brow lift are discussed in detail in this article. | ||
}} | }} | ||
= Background = | |||
Over time, the skin's elastic nature and muscle's composition deteriorates, resulting in forehead descent.<ref name="siparsky1">Siparsky PN, Kirkendall DT, Garrett WE, Jr. Muscle Changes in Aging. Sports Health. 2014 Jan ;6(1):36-40.</ref> <ref name="matarasso2">Matarasso A. Endoscopically assisted forehead-brow rhytidoplasty: theory and practice. Aesthetic Plast Surg. 1995 Mar-Apr;19(2):141-7.</ref> Correction of these displaced tissues with cosmetic surgery allows patients to improve their aesthetic appearance. This can be done by aging patients, as well as those with physiologically low brows. In deciding whether to pursue aesthetic surgery, important factors for physicians and patients to consider are the invasiveness and risks of the procedure, as well as scar appearance. In the case of brow descent, endoscopic approach to brow lifting allows skin incisions to be hidden within the patient’s hairline, allowing elevation of the entirety of the drooping forehead, in addition to reducing the muscle action of the corrugator supercilii. This is all achieved without the more objectionable associations of the more open approaches, such as a conspicuous scar, prolonged recovery time, and post-operative numbness.<ref name="nassif3">Nassif PS. Evolution in techniques for endoscopic brow lift with deep temporal fixation only and lower blepharoplasty-transconjunctival fat repositioning. Facial Plast Surg. 2007 Feb;23(1):27-42; discussion 43-4.</ref> Because of these advantages, endoscopic brow lifting is one of the most popular choices for surgical correction of the aging forehead.<ref name="graham4">Graham DW, Heller J, Kurkjian TJ, Schaub TS, Rohrich RJ. Brow lift in facial rejuvenation: a systematic literature review of open versus endoscopic techniques. Plast Reconstr Surg. 2011 Oct;128(4):335e-341e.</ref> | |||
[[File:Before and After .png|thumb|391x391px|Figure 1: Before and after photos of a patient who received an endoscopic brow lift for the correction of brow ptosis. Photo credit: Anne Barmettler, MD]] | |||
= History = | |||
The brow lift has evolved over the past century to achieve better outcomes and quicker recoveries. <ref name="byrd5">Byrd HS. The extended browlift. Clin Plast Surg. 1997 Apr;24(2):233-46.</ref> <ref name="rohrich6">Rohrich RJ, Cho MJ. Endoscopic Temporal Brow Lift: Surgical Indications, Technique, and 10-Year Outcome Analysis. Plast Reconstr Surg. 2019 Dec;144(6):1305-1310.</ref> Dr. Passot is credited with popularizing the direct brow lift procedure in the 1930’s, when he described the technique of removing small, symmetrical areas of skin superior to each brow.<ref name="paul7">Paul MD. The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg. 2001 Oct;108(5):1409-24. </ref> The skin is then reapproximated, elevating the brow. Although effective, this procedure leads to a visible scar above the brow and also does not address forehead ptosis in the glabellar region.<ref name="passot8">Passot R. Chirurgie esthetique pure: techniques et results. Paris: Gaston Doin et Cie, 1930. </ref> An adaptation of this procedure, the mid-forehead brow lift, places the incision in a prominent mid-forehead wrinkle.<ref name="booth9">Booth AJ, Murray A, Tyers AG. The direct brow lift: efficacy, complications, and patient satisfaction. Br J Ophthalmol. 2004;88(5):688-691. </ref> The procedural techniques of the brow lift were further revolutionized with the advent of the coronal brow lift. The coronal lift consists of either a subperiosteal or subgaleal dissection of forehead tissue from an ear-to-ear incision line all the way down to the level of the orbital rim. Although the coronal brow lift has the ability to achieve good results, including the glabellar region, it is limited by its relative invasiveness and longer recovery times. The trichophytic brow lift developed in the 1980’s, where the incision is just anterior to the hairline, allowed shortening of the forehead. However, the visibility of the scar along the hairline can sometimes be problematic. This led to the use of endoscopic technology for brow lifting in the 1990’s by Dr. Vasconez.<ref name="guyuron11">Guyuron B, Davies B. Subcutaneous anterior hairline forehead rhytidectomy. Aesthetic Plast Surg. 1988 May;12(2):77-83. </ref> | |||
= Physical Exam = | |||
Candidates for endoscopic brow lifts have a physiologic or age-related related brow ptosis and are aesthetically inclined. For patients with severe brow ptosis, who wish to focus solely on functional recovery of peripheral vision and do not mind a visible scar, direct brow lift may be a better solution. | |||
Because of its immediate proximity to the orbital region, a ptotic brow must be on the differential for any patient with a perceived excess of upper eyelid skin.<ref name="vasconez12">Vasconez LO. The use of an endoscope in brow lifting. A video presentation at the Annual Meeting of the American Society of Plastic and Reconstructive Surgeons. Washington DC, 1992.</ref> If an aging brow is contributing to the appearance of a drooping eyelid, then the surgical outcomes of an isolated blepharoplasty will likely not meet the patient’s expectations. Adequate preoperative discussions on realistic goals and excellent patient selection are key to successful outcomes. | |||
Brow position anatomy typically varies based on gender; a female brow is typically arched and positioned superior to the orbital rim, whereas a male brow is flatter and position on the orbital rim.<ref name="barmettler13">Barmettler, A. (2020). Chapter 21: Endoscopic Brow Lift. In S. K. Freitag, N. G. Lee, D. R. Lefebvre, & M. K. Yoon, Ophthalmic plastic surgery: Tricks of the trade. New York, NY: Thieme.</ref> While examining for brow ptosis, [[Blepharoptosis|blepharoptosis]] or [[Dermatochalasis|dermatochalasis]] should also be identified and addressed. | |||
Another element to be cognizant of during the examination is the presence of dry eye, lagophthalmos, or [[Exposure_Keratopathy|exposure keratopathy]], as an elevation of the brow could exacerbate these pathological states.<ref name="vasconez12"/> Finally, careful examination of the patient’s hairline is important in evaluation of surgical candidacy. Although there is less visible scar formation with the endoscopic approach to brow lifting, incisions may not be as well concealed if a patient is either balding or has a receding hairline. Some patients may also have a high forehead and wish to have this shortened. If this is the case, a trichophytic or pre-trichial approach may be indicated. Proper pre-operative goal discussion and counseling is crucial. | |||
= Preoperative counseling = | |||
In | In performing any sort of cosmetic surgery, it is important to evaluate patient goals and to ensure that appropriate patient selection occurs. In addition to determining whether a patient’s physical exam makes them a fitting candidate, it is crucial to assess for realistic expectations and motivations for undergoing the brow lift. | ||
= Procedure = | |||
' | In an endoscopic brow lift, a series of preoperative skin markings are made posterior to the hairline. A surgeon will typically make one central marking superior to the glabella, two paracentral markings superior to the lateral brow, and two lateral markings in the regions of the right and left temporal crescents. It is also essential to mark the 1-2 cm encompassing region of the supraorbital notch in order to consider and protect the supraorbital and supratrochlear nerves during the subperiosteal dissection.<ref name="vasconez12"/> | ||
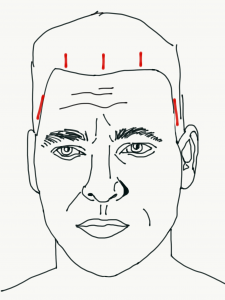
[[File:Sketch .PNG|thumb|300x300px|Figure 2: Sketch demonstrating the five preoperative skin markings made along the posterior region of a patient’s hairline. Photo credit: Naomi Bouaziz ]] | |||
In the areas identified by the central and paracentral markings, incisions are made using a 15 blade down to the bone.<ref name="black14">Black EH NF, Gladstone G, Calvano CJ, MR Levine. Smith and Nesi's Ophthalmic Plastic and Reconstructive Surgery. New York: Springer; 2012.</ref> The tissue is then dissected inferiorly to the orbital rim using a straight, spatulated raspatory in the subperiosteal plane. The endoscope is used to visualize periosteal release and location of the supraorbital nerve. Blunt tipped scissors should be used in a spreading manner to carefully dissect in the marked location of the supraorbital and supratrochlear nerves. Periosteal attachments to the orbital rim are then released, followed by corrugator and procerus muscles release to address glabellar rhytids. The temporal incisions are made down to the deep temporalis fascia in order to avoid damage of the temporal branch of the facial nerve. Dissection is then achieved with a spatulated raspatory in the temporal space to the orbital rim. Excellent release of periosteal attachments to the orbital rim are crucial. The tissue of the forehead and scalp are then mobilized superiorly to arrive at adequate elevation of the brow regions. Following the lift, the tissue is commonly secured and fixed to the bone with either anchored sutures or dissolvable implants, such as Endotines. Skin closure can be done with staples or a suture, such as a 5-0 nylon. | |||
Post-operative | = Post-operative Care = | ||
Post-operative care varies and may include an overnight compressive forehead bandage. Some surgeons recommend oral antibiotics for [[Infection_Prophylaxis|infection prophylaxis]], as well as oral methylprednisolone to address post-operative edema. Most recommend follow up for their first post-operative visit after about seven to eleven days to remove staples. | |||
= References = | |||
<references /> | |||
<ol> | |||
<li value="14">Rafaty FM, Goode RL, Abramson NR. The brow lift operation in a man. Arch Otolaryngol1978;104:69–71.</li> | |||
<li>Perenack JD. The Endoscopic Brow Lift. Atlas Oral Maxillofac Surg Clin North Am. 2016 Sep;24(2):165-73.</li> | |||
</ol> | |||
Revision as of 14:02, October 2, 2024
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Over time, the skin's elastic nature and muscle's composition deteriorates, resulting in forehead descent.[1] [2] Correction of these displaced tissues with cosmetic surgery allows patients to improve their aesthetic appearance. This can be done by aging patients, as well as those with physiologically low brows. In deciding whether to pursue aesthetic surgery, important factors for physicians and patients to consider are the invasiveness and risks of the procedure, as well as scar appearance. In the case of brow descent, endoscopic approach to brow lifting allows skin incisions to be hidden within the patient’s hairline, allowing elevation of the entirety of the drooping forehead, in addition to reducing the muscle action of the corrugator supercilii. This is all achieved without the more objectionable associations of the more open approaches, such as a conspicuous scar, prolonged recovery time, and post-operative numbness.[3] Because of these advantages, endoscopic brow lifting is one of the most popular choices for surgical correction of the aging forehead.[4]
History
The brow lift has evolved over the past century to achieve better outcomes and quicker recoveries. [5] [6] Dr. Passot is credited with popularizing the direct brow lift procedure in the 1930’s, when he described the technique of removing small, symmetrical areas of skin superior to each brow.[7] The skin is then reapproximated, elevating the brow. Although effective, this procedure leads to a visible scar above the brow and also does not address forehead ptosis in the glabellar region.[8] An adaptation of this procedure, the mid-forehead brow lift, places the incision in a prominent mid-forehead wrinkle.[9] The procedural techniques of the brow lift were further revolutionized with the advent of the coronal brow lift. The coronal lift consists of either a subperiosteal or subgaleal dissection of forehead tissue from an ear-to-ear incision line all the way down to the level of the orbital rim. Although the coronal brow lift has the ability to achieve good results, including the glabellar region, it is limited by its relative invasiveness and longer recovery times. The trichophytic brow lift developed in the 1980’s, where the incision is just anterior to the hairline, allowed shortening of the forehead. However, the visibility of the scar along the hairline can sometimes be problematic. This led to the use of endoscopic technology for brow lifting in the 1990’s by Dr. Vasconez.[10]
Physical Exam
Candidates for endoscopic brow lifts have a physiologic or age-related related brow ptosis and are aesthetically inclined. For patients with severe brow ptosis, who wish to focus solely on functional recovery of peripheral vision and do not mind a visible scar, direct brow lift may be a better solution.
Because of its immediate proximity to the orbital region, a ptotic brow must be on the differential for any patient with a perceived excess of upper eyelid skin.[11] If an aging brow is contributing to the appearance of a drooping eyelid, then the surgical outcomes of an isolated blepharoplasty will likely not meet the patient’s expectations. Adequate preoperative discussions on realistic goals and excellent patient selection are key to successful outcomes.
Brow position anatomy typically varies based on gender; a female brow is typically arched and positioned superior to the orbital rim, whereas a male brow is flatter and position on the orbital rim.[12] While examining for brow ptosis, blepharoptosis or dermatochalasis should also be identified and addressed.
Another element to be cognizant of during the examination is the presence of dry eye, lagophthalmos, or exposure keratopathy, as an elevation of the brow could exacerbate these pathological states.[11] Finally, careful examination of the patient’s hairline is important in evaluation of surgical candidacy. Although there is less visible scar formation with the endoscopic approach to brow lifting, incisions may not be as well concealed if a patient is either balding or has a receding hairline. Some patients may also have a high forehead and wish to have this shortened. If this is the case, a trichophytic or pre-trichial approach may be indicated. Proper pre-operative goal discussion and counseling is crucial.
Preoperative counseling
In performing any sort of cosmetic surgery, it is important to evaluate patient goals and to ensure that appropriate patient selection occurs. In addition to determining whether a patient’s physical exam makes them a fitting candidate, it is crucial to assess for realistic expectations and motivations for undergoing the brow lift.
Procedure
In an endoscopic brow lift, a series of preoperative skin markings are made posterior to the hairline. A surgeon will typically make one central marking superior to the glabella, two paracentral markings superior to the lateral brow, and two lateral markings in the regions of the right and left temporal crescents. It is also essential to mark the 1-2 cm encompassing region of the supraorbital notch in order to consider and protect the supraorbital and supratrochlear nerves during the subperiosteal dissection.[11]
In the areas identified by the central and paracentral markings, incisions are made using a 15 blade down to the bone.[13] The tissue is then dissected inferiorly to the orbital rim using a straight, spatulated raspatory in the subperiosteal plane. The endoscope is used to visualize periosteal release and location of the supraorbital nerve. Blunt tipped scissors should be used in a spreading manner to carefully dissect in the marked location of the supraorbital and supratrochlear nerves. Periosteal attachments to the orbital rim are then released, followed by corrugator and procerus muscles release to address glabellar rhytids. The temporal incisions are made down to the deep temporalis fascia in order to avoid damage of the temporal branch of the facial nerve. Dissection is then achieved with a spatulated raspatory in the temporal space to the orbital rim. Excellent release of periosteal attachments to the orbital rim are crucial. The tissue of the forehead and scalp are then mobilized superiorly to arrive at adequate elevation of the brow regions. Following the lift, the tissue is commonly secured and fixed to the bone with either anchored sutures or dissolvable implants, such as Endotines. Skin closure can be done with staples or a suture, such as a 5-0 nylon.
Post-operative Care
Post-operative care varies and may include an overnight compressive forehead bandage. Some surgeons recommend oral antibiotics for infection prophylaxis, as well as oral methylprednisolone to address post-operative edema. Most recommend follow up for their first post-operative visit after about seven to eleven days to remove staples.
References
- ↑ Siparsky PN, Kirkendall DT, Garrett WE, Jr. Muscle Changes in Aging. Sports Health. 2014 Jan ;6(1):36-40.
- ↑ Matarasso A. Endoscopically assisted forehead-brow rhytidoplasty: theory and practice. Aesthetic Plast Surg. 1995 Mar-Apr;19(2):141-7.
- ↑ Nassif PS. Evolution in techniques for endoscopic brow lift with deep temporal fixation only and lower blepharoplasty-transconjunctival fat repositioning. Facial Plast Surg. 2007 Feb;23(1):27-42; discussion 43-4.
- ↑ Graham DW, Heller J, Kurkjian TJ, Schaub TS, Rohrich RJ. Brow lift in facial rejuvenation: a systematic literature review of open versus endoscopic techniques. Plast Reconstr Surg. 2011 Oct;128(4):335e-341e.
- ↑ Byrd HS. The extended browlift. Clin Plast Surg. 1997 Apr;24(2):233-46.
- ↑ Rohrich RJ, Cho MJ. Endoscopic Temporal Brow Lift: Surgical Indications, Technique, and 10-Year Outcome Analysis. Plast Reconstr Surg. 2019 Dec;144(6):1305-1310.
- ↑ Paul MD. The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg. 2001 Oct;108(5):1409-24.
- ↑ Passot R. Chirurgie esthetique pure: techniques et results. Paris: Gaston Doin et Cie, 1930.
- ↑ Booth AJ, Murray A, Tyers AG. The direct brow lift: efficacy, complications, and patient satisfaction. Br J Ophthalmol. 2004;88(5):688-691.
- ↑ Guyuron B, Davies B. Subcutaneous anterior hairline forehead rhytidectomy. Aesthetic Plast Surg. 1988 May;12(2):77-83.
- ↑ Jump up to: 11.0 11.1 11.2 Vasconez LO. The use of an endoscope in brow lifting. A video presentation at the Annual Meeting of the American Society of Plastic and Reconstructive Surgeons. Washington DC, 1992.
- ↑ Barmettler, A. (2020). Chapter 21: Endoscopic Brow Lift. In S. K. Freitag, N. G. Lee, D. R. Lefebvre, & M. K. Yoon, Ophthalmic plastic surgery: Tricks of the trade. New York, NY: Thieme.
- ↑ Black EH NF, Gladstone G, Calvano CJ, MR Levine. Smith and Nesi's Ophthalmic Plastic and Reconstructive Surgery. New York: Springer; 2012.
- Rafaty FM, Goode RL, Abramson NR. The brow lift operation in a man. Arch Otolaryngol1978;104:69–71.
- Perenack JD. The Endoscopic Brow Lift. Atlas Oral Maxillofac Surg Clin North Am. 2016 Sep;24(2):165-73.