Wallenberg Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Wallenberg syndrome (WS) is a neurological disorder that is due to damage to the lateral portion of the medulla oblongata (i.e., the lateral medullary syndrome). WS is typically due to ischemia from a vertebral artery or posterior inferior cerebellar artery infarction.[1] This monograph highlights the neuro-ophthalmic presentations for the WS.
Anatomy
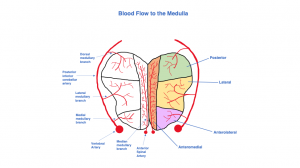
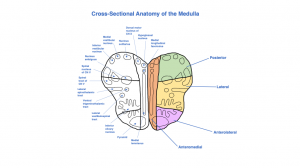
The medulla can be divided into 4 regions: anteromedial, anterolateral, lateral, and posterior ( Figure 1). These regions are divided based on their differing arterial supply. The primary blood supply to the medulla comes from the vertebral arteries. The vertebral artery supplies the posterior inferior cerebellar artery (PICA), which has 3 main branches: the dorsal, medial, and lateral medullary branches. The dorsal medullary branch of PICA perfuses the posterior medulla. The medial medullary branch of PICA perfuses the anterior lateral medulla, and the lateral medullary branch perfuses the lateral medulla. The anterior spinal artery provides blood flow to the remainder of the medulla. The anterior spinal artery has its own median medullary branch, which perfuses the anteromedial region of the medulla.[2] The blood flow and the cross-sectional anatomy of the medulla are illustrated in figures 1 and 2.
Etiology
WS is most commonly due to an occlusion of the PICA, resulting in ischemia and infarction of the lateral medulla. While most commonly due to PICA occlusion, other arteries, such as the vertebral artery or branches of PICA, can be involved as well.[1][2] Primary etiologies include atherosclerosis, hypertension and other vasculopathic risk factors. Other rarer causes such as vertebral artery dissection especially in predisposed younger individuals with Ehlers-Danlos Syndrome, Marfan syndrome, fibromuscular dysplasia and hypoplastic vertebral artery have been noted in prior literature.[3][4]
Diagnosis
Ocular Manifestations
- Horner syndrome (miosis, ptosis, upside down ptosis, anhidrosis)– due to disruption of the oculosympathetic chain, which descends through the lateral medulla
- Ptosis from Horner syndrome
- Oscillopsia due to rotary nystagmus – due to disruption of communicating neurons between brainstem and inferior cerebellar peduncle; patient experiences oscillopsia, nausea, vomiting, vertigo, dizziness[5]
- Binocular oblique diplopia – secondary to skew deviation from disruption of otolithic input at the level of the brainstem[6]
Systemic Manifestations[2] (Table 1[7])
- Ipsilateral facial pain/numbness
- Contralateral body pain/numbness
- Gait ataxia
- Dysphagia – difficulty swallowing
- Dysarthria – slurred speech
- Dysphonia – disorderly voice
- Palatal myoclonus – twitching mouth
| Anatomical Structure of Medulla | Signs and Symptoms |
|---|---|
| Medial lemniscus | Contralateral loss of vibration and proprioception of body |
| Pyramid | Contralateral motor loss |
| Inferior olivary nucleus | Loss of motor coordination and learning |
| Lateral vestibulospinal tract | Minor loss of vestibulomotor coordination |
| Ventral trigeminothalamic tract | Ipsilateral loss of pain and temperature of face |
| Lateral spinothalalmic tract | Contralateral loss of pain and temperature of body |
| Spinal tract of CN V | Ipsilateral loss of pain and temperature of face |
| Spinal nucleus of CN V | Ipsilateral loss of pain and temperature of face |
| Nucleus ambiguus | Difficulty swallowing, elevating palate, hoarseness, dysphagia |
| Inferior vestibular nucleus | Nausea, vomiting, vertigo |
| Medial vestibular nucleus | Nausea, vomiting, vertigo |
| Nucleus solitarius | Difficulty with taste and processing visceral sensory info |
| Dorsal motor nucleus of CN X | Difficulty swallowing, elevating palate, hoarseness, dysphagia |
| Hypoglossal nucleus | Difficulty with movement of tongue |
| Medial longitudinal fasciculus | Disconjugate horizontal gaze |
Management
Treatment
Treatment for WS depends on its etiology. Because it is almost always caused by a stroke, treatment is time dependent. Because this condition is caused by a stroke of the brainstem, the use of intravenous tissue-type plasminogen activator can be used if administered within 4-5 hours of symptom onset.[8] Long term ophthalmic care after WS are designed to improve visual symptoms. Optical therapy, using eye patches or prisms , has been used to alleviate unresolved diplopia.
References
- ↑ 1.0 1.1 Saleem F, M Das J. Lateral Medullary Syndrome. [Updated 2019 Dec 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
- ↑ 2.0 2.1 2.2 Ogawa K, Suzuki Y, Oishi M, Kamei S. Clinical study of 46 patients with lateral medullary infarction. J Stroke Cerebrovasc Dis. 2015 May;24(5):1065-74.
- ↑ Galende, A.V., Camacho, A., Gomez‐Escalonilla, C., Penas, M., Juntas, R., Ramos, A. and Esteban, J. (2004), Lateral Medullary Infarction Secondary to Vertebral Artery Dissection Presenting as a Trigeminal Autonomic Cephalalgia. Headache: The Journal of Head and Face Pain, 44: 70-74. doi:10.1111/j.1526-4610.2004.04012.x
- ↑ Giannopoulos S, Markoula S, Kosmidou M, Pelidou SH, Kyritsis AP. Lateral medullary ischaemic events in young adults with hypoplastic vertebral artery. J. Neurol. Neurosurg. Psychiatry. 2007 Sep;78(9):987-9.
- ↑ Morrow, M.J. and Sharpe, J.A. (1988), Torsional nystagmus in the lateral medullary syndrome. Ann Neurol., 24: 390-398. doi:10.1002/ana.410240307
- ↑ Brandt TH, Dieterich M. Different types of skew deviation. Journal of Neurology, Neurosurgery & Psychiatry 1991;54:549-550.
- ↑ Berkowitz AL. eds. Clinical Neurology and Neuroanatomy: A Localization-Based Approach New York, NY: McGraw-Hill; . http://neurology.mhmedical.com.srv-proxy2.library.tamu.edu/content.aspx?bookid=1984§ionid=147771107.Accessed March 24, 2020.
- ↑ Salerno A, Cotter BV, Winters ME. The Use of Tissue Plasminogen Activator in the Treatment of Wallenberg Syndrome Caused by Vertebral Artery Dissection. J Emerg Med. 2017 May;52(5):738-740.