All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Isolated orbital floor fracture.
Disease
Orbital floor fracture, also known as “blowout” fracture of the orbit. A "blowout" fracture of the orbital floor is defined as a fracture of the orbital floor in which the inferior orbital rim is intact.
Etiology
Fractures of the orbital floor are common: it is estimated that about 10% of all facial fractures are isolated orbital wall fractures (the majority of these being the orbital floor), and that 30-40% of all facial fractures involve the orbit. The anatomy of the orbital floor predisposes it to fracture. The inferior orbital neurovascular bundle (comprising the infraorbital nerve and artery) courses within the bony floor of the orbit; the roof of this infraorbital canal is only 0.23mm thick, and the bone of the posterior medial orbital floor averages 0.37 mm thick. By contrast, the bone of the lateral portion of the orbital floor averages 1.25 mm thick, over 5 times the thickness of the bone over the neurovascular bundle. As one might suspect, it is this very thin area of the orbital floor overlying the neurovascular bundle where isolated orbital floor fractures frequently occur.
Risk Factors
Patients who suffer blunt trauma to the globe or periocular area, especially directly on the globe or on the cheek, are at risk of developing an orbital floor fracture.
General Pathology
The thin floor of the orbit, typically medial to the infraorbital neuromuscular bundle, is broken and a piece of this bone is generally displaced downward into the maxillary sinus. Orbital tissue herniating into the sinus through the resulting defect in the orbital floor may become entrapped, causing diplopia and possible oculocardiac reflex; if the displacement of the bony fragment is large enough, enophthalmos may develop.
Pathophysiology
Two theories predominate to explain the occurrence of orbital “blowout” fractures. In the “hydraulic” theory, the eyeball itself is struck directly from an object such as a fist or a baseball. The eyeball is thrust posteriorly, transiently raising the pressure within the orbit. As the intraorbital pressure increases dramatically and suddenly, the floor of the orbit “blows out” inferiorly at the point of greatest weakness, just above the intraosseous course of the infraorbital neurovascular bundle. The increased orbital pressure simultaneously fractures the bony floor and pushes the bone fragment downward, displacing the bone into the maxillary sinus, along with soft tissue from the orbit. In the “buckling” theory, blunt trauma to the face (such as a punch to the cheek) transmits a pressure wave posteriorly, acutely compressing the bones of the orbit in the anterior-posterior direction. This increase in bony pressure causes the weakest point in the orbit to “buckle” and crack, with the bone fragment thus created to be pushed inferiorly. It is likely that each mechanism may be operative in varying degrees in different patients, depending on the mechanism and location of the traumatic insult. Indeed, recent studies on cadavers suggest that both theories are valid.
Primary prevention
Prevention of an orbital floor fracture is only possible by preventing blunt trauma to the midface. The use of proper eye and/or face protection for sports can prevent some sports related fractures.
Diagnosis
History
Almost all patients will report recent trauma to the eye or the midface prior to the occurrence of the fracture. In cases of occult fractures discovered incidentally or years after the injury, the patient may have no recollection of the actual traumatic incident.
Physical examination
In the acute setting of midfacial trauma, a complete ophthalmologic examination is vital; in the event of a ruptured globe, retinal detachment, intraocular bleed, or other sight threatening complication, all orbital intervention should be postponed until the eye is stabilized. When an orbital floor fracture is suspected, the presence or absence of enophthalmos should be noted and the measurement of extraocular motility is vital.
Signs
Patients with an orbital floor fracture may present with a tropia in upgaze and/or downgaze, with the affected side demonstrating limitation of full movement. Occasionally, patients may have diplopia in primary gaze and even with horizontal eye movements, but these presentations are much less common. If there is tethering or entrapment of orbital tissue in the fracture the patient may also have nausea and/or bradycardia with vertical eye movements. Many patients will have some level of decreased sensation to V2.
Enophthalmos of the affected side may be present initially, but more commonly develops days to weeks after the injury as orbital swelling subsides.
Symptoms
A patient with a “blowout” fracture of the orbital floor may have pain or diplopia (or both) on vertical eye movements.
Clinical diagnosis
Patients who have diplopia and/or pain with vertical movements of the eyes after blunt midfacial trauma should be suspected to have an orbital floor fracture. However, the diagnosis of an orbital floor fracture without entrapment can only be made radiologically. Forced ductions to manually rotate the globe can sometimes be performed in the clinic or emergency room setting, and may indicate restriction of movement.
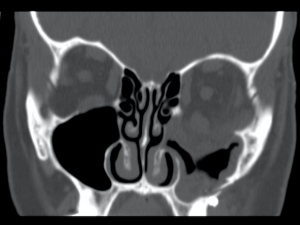
Diagnostic procedures
Patients suspected of suffering an orbital floor fracture should undergo thin cut (1.0 - 1.5mm) axial CT scans of the orbit with coronal reconstruction (Thin cut coronal reconstructions are actually preferred to direct coronal images as they avoid artifact from dental amalgam). In the great majority of floor fractures, a fracture can be localized above, or just medial to, the course of the infraorbital nerve. A fracture in this location leads either to a “trap door” displacement of the orbital floor, or, if a second fracture is present at the junction of the floor and medial wall, to a completely depressed, separate bony fragment. These deformities are best appreciated on coronal images. Herniation of the inferior rectus muscle into the maxillary sinus through the orbital defect does not predict clinical dysmotility. Many patients with radiologic evidence of inferior rectus herniation do not have clinical entrapment, while many patients in whom orbital fat herniates into the defect, but where the inferior rectus muscle remains in the orbit, have severe dysmotility. The extraocular muscles are connected to each other and to the orbital fat through a complicated interconnecting web of septa, such that even if fat alone is incorporated into the fracture, profound dysmotility may result. Entrapment is a purely clinical diagnosis, not a radiologic one. Rarely, if ever, is performing a forced duction test necessary or informative in making the diagnosis of extraocular muscle restriction in an awake patient with an orbital blowout fracture.
Laboratory test
Not applicable
Differential diagnosis
Following periorbital trauma, patients may experience diplopia due to orbital congestion, extraocular muscle or nerve paresis, or a traumatic loss of fusion. Enophthalmos following midfacial trauma is almost always due to an orbital fracture, but may be due to a fracture of the medial wall of the orbit as opposed to the orbital floor.
Management
General treatment
Selection of patients for surgery and timing of repair
Immediately after an orbital floor fracture, the affected eye may have impaired motility, resulting in double vision. The eye may be proptotic or enophthalmic, depending on the amount of edema (causing proptosis) and the size of the fracture (larger fractures leading to enophthalmos). As the acute swelling resolves, double vision will generally either stay the same or improve, while the enophthalmos will either remain the same or worsen. Thus while diplopia may be an initial concern immediately after the injury, it often resolves over time on its own without surgical intervention.
Surgical repair of the fracture is indicated when enophthalmos is troublesome to the patient, or when diplopia interferes with the patient’s activities. In cases of severe entrapment—for example, where there is a complete lack of supraduction, fairly severe pain on eye movement, or hemodynamic instability—urgent intervention is warranted. However, since most cases with less severe dysmotility resolve without intervention, it is prudent to wait at least 14 days to repair an isolated orbital floor fracture, especially if improvement in motility is seen in the first week after the injury. If disabling diplopia is still present two to three weeks after the injury without signs of improving motility, surgical repair is warranted. While motility is improving, especially when documented with a progressively smaller prismatic deviation over time, surgery may be delayed to determine if the diplopia will completely resolve on its own, or at least resolve to the patient’s satisfaction. Usually, by 3-4 weeks after the injury, a decision regarding surgery can be made with respect to disabling diplopia. There is no compelling evidence that orbital fracture surgery should be performed within a "two week window” following the injury, and it is common for patients to continue to note improvement in diplopia even after the two week window, thus avoiding surgery. Further, multiple studies have shown that delaying surgery beyond two weeks is equally effective as earlier surgery, as long as all adhesions to the bony edges and to the sinus mucosa are lysed, the bony defect is completely exposed, and the implant is properly placed.
Surgery to prevent enophthalmos should probably be discouraged, since it is impossible to predict who will develop enophthalmos and how enophthalmos will affect the patient (i.e., the patient may not be bothered by it). Furthermore, studies support the notion that enophthalmos is corrected equally well when addressed several weeks after an injury when compared to repair within the “two week window.” The risks of surgery should also be discussed with the patient, including implant infection or reaction, hyperglobus, diplopia, hemorrhage, infection, injury to the globe or optic nerve, and loss of vision.
Medical therapy
Patients with dysmotility may benefit from a short (5-7 day) course of steroids (0.75 – 1.0 mg/kg per day of prednisone) in the acute setting if there are no contraindications. Such treatment may help periorbital and extraocular muscle edema to subside more quickly to determine if the patient’s dysmotility is transient or if surgery is necessary. Antibiotics may be prescribed in the acute setting. Patients should be informed that nose-blowing could lead to orbital or soft tissue emphysema and is discouraged for 4-6 weeks after the injury.
Medical follow-up
Adult patients who have diplopia (or pain on eye movements) in the acute setting of an orbital floor fracture should be evaluated again within a week following the injury, and if diplopia persists, should be seen at weekly intervals as long as the dysmotility is improving. Once improvement stops, a decision for surgical repair is appropriate.
Surgery
All orbital floor fractures should be repaired via a transconjunctival approach. While a lateral canthotomy and inferior cantholysis are often advocated, they are unnecessary and can be omitted with no loss of exposure.
A conjunctival incision is made with monopolar cautery (with a corneal protector in place) across the length of the eyelid just below the base of the tarsus. Once the incision is complete, two 5-0 silk traction sutures are placed in the free conjunctival edge, pulled superiorly, and clamped to the head drape over the forehead, pulling a sheet of conjunctiva superiorly to cover the cornea; this maneuver serves to protect the cornea as well as to provide retraction. Blunt dissection can be performed in the eyelid atraumatically in the plane between the orbital septum and orbicularis muscle with a cotton tipped applicator down to the orbital rim, while the anterior lamella is simultaneously retracted with a DeMarres retractor. The perisoteum is opened with monopolar cautery and lifted off of the orbital floor.
In order to perform a successful repair, all of the herniated orbital tissue must be repositioned back into the orbit. When possible, the infraorbital neurovascular bundle, inferior rectus, and inferior oblique should be visualized as they are important surgical landmarks. A plane should be developed between the orbital tissue (above the plane of dissection) and the infraorbital nerve and the exposed sinus mucosa (below the plane of dissection). Both blunt and sharp dissection may need to be employed. It is important to completely dissect over the entire fracture site, i.e., 360 degrees of bony edge must ultimately be visualized around the fracture site. An orbital implant should be fashioned in the shape of a “guitar pick” with the narrow-width portion placed posteriorly, and if porous, can be soaked in an antibiotic solution such as a mixture of Bacitracin and Polymixin. The orbital implant should then be placed (under direct visualiztion) to rest on the posterior lip of the fracture, thereby covering the entire defect, without incarcerating orbital tissue beneath the implant. The implant may be fixated by a variety of methods, depending on the surgeon’s preference. There are also options for patient-specific implants that are custom made for each patient's fracture based on the defect seen on radiographic imaging[1]. Following the placement of the implant, a forced duction test can be performed to insure that no tissue is trapped beneath the implant. In some cases where the inferior rectus muscle is swollen or hemorrhagic, a forced duction test may still reveal resistance despite a properly performed surgical repair; in such cases, diplopia may still resolve over time but there is a greater likelihood that some level of diplopia will persist due to intrinsic damage to the inferior rectus muscle.
One technique that may be useful in implant fixation is to use a few drops of a cyanoacrylate derivative (a “superglue” such as Histoacryl) just beneath the leading edge of the implant to cause adherence of the implant to the (dry) bone beneath it. A 1 cc tuberculin syringe with a 26 gauge needle is ideal for this purpose. This technique is especially valuable with porous implants that will eventually fibrose into place biologically but may need 3-4 weeks of stabilization postoperatively prior to tissue ingrowth.
Intraoperatively, steroids should be given intravenously (20 mg of Decadron), followed by a three to five day course of oral prednisone (0.75 – 1.0 mg/kg per day) to limit orbital swelling.
It is helpful to remind patients preoperatively that even with a perfect repair, residual/permanent diplopia can still result if the inferior rectus is damaged. Further, even though herniated tissue is repositioned back into the orbit, fat atrophy may occur and enophthalmos is therefore typically improved but not always completely eliminated. Prior to surgery, patients should also be reassured that recovery of extraocular muscle function will not be immediate, and that several weeks (and even a few months) may be required for full recovery to occur. Usually 6-9 months should elapse after surgery before assuming that no further recovery will be observed, and before strabismus surgery, if indicated, should be performed.
Postoperatively, if motility is not improving or improving very slowly, a CT scan can be performed to check the placement of the implant. Radiologically visible implants hold an advantage in this regard, and a CT image showing proper implant placement can reassure the patient (and surgeon) that no further intervention is warranted.
Surgical follow up
Patients undergoing repair should have the vision checked in the recovery room to ensure there is no intraoperative loss of vision, and then can be seen one week postoperatively, 3 weeks postoperatively, and 2-3 months postoperatively. A postoperative CT scan is often warranted to document the proper placement of the implant.
Complications
The most common mistakes and complications in the management of orbital floor fractures are the following:
Operating too early: In many cases, diplopia resolves on its own in two or three weeks, or resolves to the point where it does not interfere with the patient’s activities (e.g, the patient is left with diplopia only in extreme upgaze). Unless there is severe restriction of motility where recovery of normal movement is clearly impossible without intervention, observing the patient for a period of one or two weeks is preferred prior to making a decision regarding surgery.
Creating a subciliary incision or performing aggressive dissection through the lower eyelid: Lower eyelid malposition (such as severe cicatricial retraction) following a subciliary incision is common and difficult to treat; creating a transconjunctival incision and atraumatically dissecting through the lower eyelid bluntly prevents a multiple plane dissection, and minimizes the chances of scarring in the eyelid causing postoperative contracture and retraction.
Not covering the entire posterior extent of the bony defect with the implant, especially posteriorly: Failure to cover the defect posteriorly can lead to herniation of tissue through the residual hole with scarring to the sinus mucosa, leading to postoperative enophthalmos and diplopia. It is essential to cover the entire defect, and fixation can insure that, once in place, the implant will not shift (especially anteriorly) and be displaced through the hole in the orbital floor.
Visual loss: Nearly all cases of visual loss following orbital floor fracture repair occur due to elevated pressure in the orbit causing a compartment syndrome, either due to orbital hemorrhage or edema compressing the optic nerve. The optic nerve exits the orbit through the optic foramen, located at the superonasal portion of the orbit. As one surgically dissects posteriorly to gain access to the posterior rim of the floor fracture, the nerve is actually not in close proximity to the area of dissection. Many more complications ensue from failure to dissect posteriorly enough in the repair of the fracture than from causing direct injury to the optic nerve, an intraoperative complication which is extraordinarily rare and, from an anatomic point of view, difficult to produce.
Prognosis
Most patients who suffer an isolated orbital floor fracture—even those requiring surgical repair—have good outcomes. In those patients whose fractures are repaired appropriately, poor outcomes are generally associated with permanent paresis of an extraocular muscle (usually due to the initial injury) or fibrosis of an extraocular muscle causing restriction. Persistent enophthalmos may occur in the setting of fat atrophy.
Long term complications related to implants, however, include implant infection, migration, capsular hemorrhage, and need for implant removal. These complications have been reported to occur even many years after the initial repair.
Additional Resources
- Boyd K, Rizzuto PR. What Is an Orbital Fracture? American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/orbital-fracture. Accessed March 02, 2023.
References
- ↑ Habib LA, Yoon MK. Patient specific implants in orbital reconstruction: A pilot study. Am J Ophthalmol Case Rep. 2021 Oct 19;24:101222. doi: 10.1016/j.ajoc.2021.101222. PMID: 34746511; PMCID: PMC8554165.