Oculocardiac Reflex
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
First described in 1908, the oculocardicac reflex (OCR; also known as the Aschner reflex or trigeminovagal reflex) is a reduction of the heart rate resulting from direct pressure placed on the extraocular muscles (EOM), globe, or conjunctiva.[1] The reflex is defined by a decrease in heart rate by greater than 20% following the exertion of the aforementioned eye pressure.[2] The reflex is mediated by the connection between the ophthalmic branch of the trigeminal nerve and the vagus nerve. Most commonly, the reflex induces bradycardia, though it has also been reported to cause arrhythmias and, in extreme cases, cardiac arrest. The reflex has most often been encountered during ophthalmologic procedures such as strabismus surgery, though it has also been seen in cases of facial trauma, regional anesthetic nerve blocks, and mechanical stimulation.[3] Historically, the oculocardiac reflex was used as a diagnostic tool to evaluate syncope, as well as to terminate supraventricular tachycardias, but this is no longer done given the limited clinical application and the associated risks.[4]
Pathophysiology
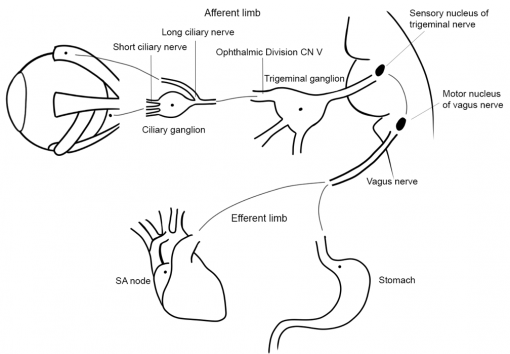
The OCR arc is comprised of an afferent limb (carried by the trigeminal nerve (CN V)) and an efferent limb (carried by the vagus nerve (CN X)). The reflex begins with the activation of stretch receptors in periorbital and ocular tissues. The long and short ciliary nerves carry the impulses to the ciliary ganglion, where the ophthalmic division of CN V carries the impulses to the Gasserian ganglion, and subsequently to the trigeminal nucleus. The afferent nerves synapse with the visceral motor nucleus of the vagus nerve in the reticular formation of the brain stem, where the impulses are then carried to the myocardium to activate the vagal motor response at the sinoatrial (SA) node, resulting in bradycardia.[5]
Epidemiology
Incidence of the OCR varies widely in literature depending on the clinical conditions. Two studies reported the incidence of the OCR during strabismus surgery as 56% and 68%, while rates were lower in facial surgery (specifically an orbitozygomatic approach), where the rate was 31.7%.[6][7] Incidence of the OCR does appear to decrease with age, with the pediatric population being most at risk.[2] Pediatric patients are not only more likely to be in a situation where the reflex is triggered (i.e., strabismus surgery), but they are also at higher risk of susceptibility to worse outcomes due to their higher dependence on heart rate to maintain cardiac output as compared to adults.[8] There does not appear to be a clear consensus on whether incidence is dependent the specific extraocular muscle (EOM). One source mentions that the medial rectus muscle is particularly sensitive to the induction of the OCR, while other studies show that the EOM being operated on makes no significant difference in the occurrence of the reflex.[9][10] Though incidence is reportedly higher in younger populations, the reflex occurs in adults and has been seen during many facial trauma surgeries with stimulation of the branches of the trigeminal nerve.[11]
Other than the physical stimulus of pressure on the orbit and EOMs, other risk factors include hypercarbia, hypoxemia, and type of anesthesia. Hypercarbia and hypoxemia are associated with an increased incidence of bradycardia and are more likely to occur in a spontaneously breathing patient. Anesthesia choice has also been shown to affect the incidence rate of OCR-associated bradycardia. Studies have shown that in mechanically-ventilated patients, propofol anesthesia resulted in the greatest decrease in heart rate, while ketamine was associated with the least decrease. In a separate study in spontaneously breathing patients who did not receive prophylaxis, sevoflurane was associated with the lowest incidence of OCR, while the incidence with halothane was almost double.[1]
Diagnosis
Intra-Operative Diagnosis
Intra-operative diagnosis is made based on the acute change in cardiac function during facial/ocular surgery, where the trigeminal nerve may be involved. The reflex should be suspected in anyone who has a sudden drop in heart rate that is not attributable to other causes and the patient should be stabilized prior to continuing on with the surgery.[2] Patients who are considered at-risk for the OCR should warrant particular attention [see Management for more].
Non-Operative Diagnosis
In a non-operative setting, such as a patient presenting with orbital trauma, motility restriction (e.g. restrictive vertical strabismus, in the case of an orbital trapdoor fracture) in combination with nausea, vomiting, diplopia, and headache should raise concerns for a possible OCR. Patients may also present with symptoms seen in intra-operative OCR, such as bradycardia and asystole.[12] This type of trauma is particularly relevant in the pediatric population, as they are susceptible to trapdoor fractures due to their more flexible bones.[13]
Management
When patients who have sustained ocular trauma (particularly orbital fractures) present with symptoms described in the previous section and OCR is suspected, an electrocardiogram (ECG) should be performed to assess cardiac function. If heart block is present, immediate surgery is indicated. Not only could this prevent death from fatal arrhythmias induced by the reflex, but it will improve outcomes for ocular motility as well.[14] The OCR can evolve over time, so the patient needs to be monitored closely for changes to their wellbeing and stability.[15]
In a peri-operative setting, the first step in management of the OCR is risk stratification, which begins with identifying those individuals who fall into an at-risk population (i.e., pediatric) or require an at-risk surgery (i.e., strabismus surgery). If a patient is deemed to be at-risk based on these factors, the surgical team needs to be aware of the consequences of the OCR and should implement the following protocol:[16]
- Avoid sudden or sustained traction on EOMs
- Use prophylaxis (regional nerve block and/or anticholinergics) in high-risk patients [see 'Prophylaxis' below])
- Implement continuous cardiac monitoring and avoid hypoxia/CO2 retention
- If the OCR is triggered, immediately remove the inciting stimulus
- If removal of stimulus does not stabilize the patient, administer IV anticholinergic (e.g. atropine or glycopyrrolate)
- In the event of an OCR refractory to anticholinergic administration, add epinephrine and institute cardiopulmonary resuscitation
Releasing the traction that triggered the stimulus is usually enough to stop the dysrhythmia within 10-20 seconds. If bradycardia persists longer than 20 seconds or if the dysrhythmia is concerning based on other factors (such as patient status), then IV atropine (10-20 mcg/kg) or glycopyrrolate (10 mcg/kg) should be administered. If IV access is unavailable, intraglossal administration can be used, as it has been shown to be superior to IM administration and may even be superior to IV administration.[3]
Once sinus rhythm is restored, it is generally safe to proceed with the surgery. Prevention and treatment of the OCR is simpler in a controlled environment, such as elective surgery, and more difficult under less controlled environments such as trauma; in these situations, pharmacological intervention tends to be more of a necessity.[2]
Prophylaxis
The use of prophylaxis for the OCR and its efficacy has been long debated. The consensus is that most pediatric patients who are undergoing strabismus surgery should be treated with prophylactic IV anticholinergics (glycopyrrolate has been shown to be somewhat more effective with a 5% reduction in OCR incidence versus the 2% reduction from atropine ). Oral or IM administration for preoperative treatments is less effective and not recommended. Those who oppose using atropine as a prophylactic measure worry that atropine itself can cause dysrhythmias (i.e. ventricular tachycardia and ventricular fibrillation). These dysrhythmias can be more concerning and more difficult to mitigate than those caused by the OCR; these consequences are also more common in adult patients, making the use of prophylaxis in adults less favorable. Given that healthy pediatric patients can typically tolerate the tachycardic effects of atropine, administration of the prophylaxis should be safe in this population. Retrobulbar blocks have been shown to be effective in the prevention of the OCR, though they are not commonly used during pediatric procedures and have been known to trigger the reflex during their placement. One study found that administration of topical lidocaine was associated with a 60% decrease in the incidence of the OCR, though the study had a limited sample size and this topic has not been studied since then.[3]
Prognosis
In general, post-operative recovery of surgically-induced OCR is uneventful if the reflex is recognized and managed appropriately.[5] That being said, there are several reports of OCR-related deaths; it is estimated that 1 out of every 3500 cases of OCR-induced cardiac arrhythmia is fatal, making the OCR an important consideration.[17] The OCR can be complicated by underlying health issues, as in a case report of a 5-year-old boy who died of OCR exaggerated by an Epstein-Barr Virus (EBV) myocarditis during elective strabismus surgery.[18] Other reports of death from the OCR have also been reported, resulting from procedures, such as cold ocular irrigation, retinal detachment surgery, and strabismus surgery.[19]
References
- ↑ 1.0 1.1 Tobin JR, Grey Weaver R, Chapter 34 - Ophthalmology, A Practice of Anesthesia for Infants and Children (Sixth Edition), Elsevier, 2019, Pages 790-803.e4, ISBN 9780323429740, doi:10.1016/B978-0-323-42974-0.00034-3.
- ↑ 2.0 2.1 2.2 2.3 Dunville LM, Sood G, Kramer J. Oculocardiac Reflex. [Updated 2020 Jun 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.https://www.ncbi.nlm.nih.gov/books/NBK499832/.
- ↑ 3.0 3.1 3.2 Justice LT, Valley RD, Bailey AG, Hauser MW, CHAPTER 27 - Anesthesia for Ophthalmic Surgery, Smith's Anesthesia for Infants and Children (Eighth Edition), Mosby, 2011, Pages 870-888, ISBN 9780323066129, doi:10.1016/B978-0-323-06612-9.00027-4. (http://www.sciencedirect.com/science/article/pii/B9780323066129000274)
- ↑ Brignole M, Menozzi C, Gianfranchi L, Oddone D, Lolli G, Bertulla A. Carotid sinus massage, eyeball compression, and head-up tilt test in patients with syncope of uncertain origin and in healthy control subjects. Am Heart J. 1991;122(6):1644-1651. doi:10.1016/0002-8703(91)90282-m.
- ↑ 5.0 5.1 Spiriev T, Chowdhury T, Schaller BJ, Chapter 2 - The Trigeminal Nerve: Anatomical Pathways. Trigeminocardiac Reflex Trigger Points, Academic Press, 2015, Pages 9-35, ISBN 9780128004210, doi: 10.1016/B978-0-12-800421-0.00002-3. (http://www.sciencedirect.com/science/article/pii/B9780128004210000023)
- ↑ Min, SW., Hwang, JM. The incidence of asystole in patients undergoing strabismus surgery. Eye 23, 864–866 (2009). https://doi.org/10.1038/eye.2008.127 (https://www.nature.com/articles/eye2008127)
- ↑ Neils D, Singanallur P, Vasilakis M, Wang H, Tsung A, Klopfenstein J, Incidence and Ramifications of the Oculocardiac Reflex During the Orbitozygomatic Approach: A Prospective Assessment, World Neurosurgery, Volume 82, Issue 6, 2014, Pages e765-e769, ISSN 1878-8750, doi:10.1016/2013.08.032. (https://www.sciencedirect.com/science/article/pii/S187887501301053X)
- ↑ Jean YK, Kam D, Gayer S, Palte HD, Stein ALS. Regional Anesthesia for Pediatric Ophthalmic Surgery: A Review of the Literature. Anesth Analg. 2020;130(5):1351-1363. doi:10.1213/ANE.0000000000004012
- ↑ Deriy L, Gerstein NS, Panikkath P, Ram H, Starr B, Chapter 16 - Cardiac Patients Requiring Emergent Noncardiac Surgery, Essentials of Cardiac Anesthesia for Noncardiac Surgery, Elsevier, 2019, Pages 404-452, ISBN 9780323567169, doi:10.1016/B978-0-323-56716-9.00016-3. (https://www.sciencedirect.com/science/article/pii/B9780323567169000163)
- ↑ Ha, SG., Huh, J., Lee, BR. et al. Surgical factors affecting oculocardiac reflex during strabismus surgery. BMC Ophthalmol 18, 103 (2018). Doi:10.1186/s12886-018-0771-9 (https://bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-018-0771-9)
- ↑ Pham CM, Couch SM. Oculocardiac reflex elicited by orbital floor fracture and inferior globe displacement. Am J Ophthalmol Case Rep. 2017;6:4-6. Published 2017 Feb 3. doi:10.1016/j.ajoc.2017.01.004
- ↑ Bansagi ZC, Meyer DR, Internal orbital fractures in the pediatric age group: Characterization and management, Ophthalmology, Volume 107, Issue 5, 2000, Pages 829-836, ISSN 0161-6420, Doi: 10.1016/S0161-6420(00)00015-4. (https://www.sciencedirect.com/science/article/pii/S0161642000000154)
- ↑ Buck LS, Stockton S, Spankovich C, Jordan JR, Pediatric orbital floor fractures and the oculocardiac reflex: Experience from a level I trauma center, American Journal of Otolaryngology,Volume 41, Issue 4, 2020, 102553, ISSN 0196-0709, doi: 10.1016/j.amjoto.2020.102553. (https://www.sciencedirect.com/science/article/pii/S0196070920302477)
- ↑ Sires, Bryan S. M.D., Ph.D. Orbital Trapdoor Fracture and Oculocardiac Reflex, Ophthalmic Plastic & Reconstructive Surgery: July 1999 - Volume 15 - Issue 4 - p 301. (https://journals.lww.com/op-rs/Citation/1999/07000/Orbital_Trapdoor_Fracture_and_Oculocardiac_Reflex.14.aspx)
- ↑ Yoo JJ, Gishen KE, Thaller SR. The Oculocardiac Reflex: Its Evolution and Management. J Craniofac Surg. 2021 Jan-Feb 01;32(1):e80-e83. doi: 10.1097/SCS.0000000000006995. PMID: 33186288. (https://pubmed.ncbi.nlm.nih.gov/33186288/)
- ↑ Sachidanand J. Bharati, Tumul Chowdhury, Chapter 7 - The Oculocardiac Reflex, Trigeminocardiac Reflex, Academic Press, 2015, Pages 89-99, ISBN 9780128004210, doi:10.1016/B978-0-12-800421-0.00007-2. (http://www.sciencedirect.com/science/article/pii/B9780128004210000072)
- ↑ Sires BS, Stanley RB, Levine LM. Oculocardiac Reflex Caused by Orbital Floor Trapdoor Fracture: An Indication for Urgent Repair. Arch Ophthalmol. 1998;116(7):955–956. (https://jamanetwork.com/journals/jamaophthalmology/fullarticle/262873)
- ↑ Fayon M, Gauthier M, Blanc VF, Ahronheim GA, Michaud J. Intraoperative cardiac arrest due to the oculocardiac reflex and subsequent death in a child with occult Epstein-Barr virus myocarditis. Anesthesiology. 1995 Sep;83(3):622-4. doi: 10.1097/00000542-199509000-00024. PMID: 7661365.
- ↑ Smith, R.B. Death and the oculocardiac reflex. Can J Anaesth 41, 760 (1994). Doi: 10.1007/BF03015643 (https://link.springer.com/article/10.1007/BF03015643#citeas)