Light Adjustable Intraocular Lenses
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Surgical Therapy
Light Adjustable Intraocular lens (LAL) allows post operative titrations in intraocular lens (IOL) power after the eye has healed and secured refractive stability post cataract surgery, facilitating customization and optimization of lens to achieve the desired vision . At present, the LAL can be adjusted for spherical and cylindrical power changes.
Background
The rationale for the invention of the Light Adjustable Lens was to tackle important issues that lead to unsatisfactory uncorrected visual outcomes in cataract surgery such as inaccurate biometry, unpredictable effective lens position, and wound healing, given that cataract extraction is one of the most common surgeries undertaken worldwide.
The project was spearheaded by Danial Schwartz, M.D. from the University of California, San Francisco, and Robert Grubbs, Chemistry Professor at the California Institute of Technology in the year 1997. They jointly developed a lens whose three dimensional structure could be altered non-invasively with the application of light energy.
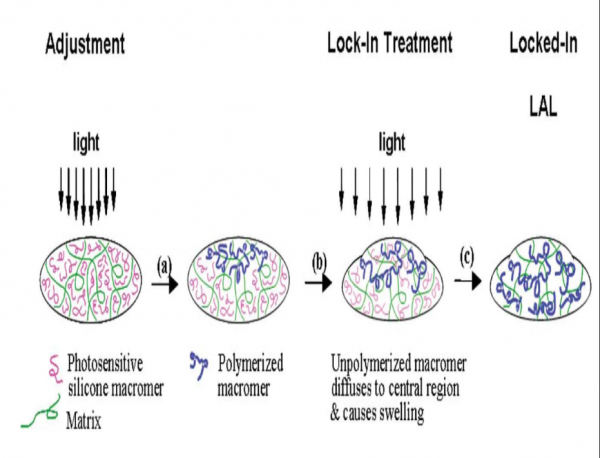
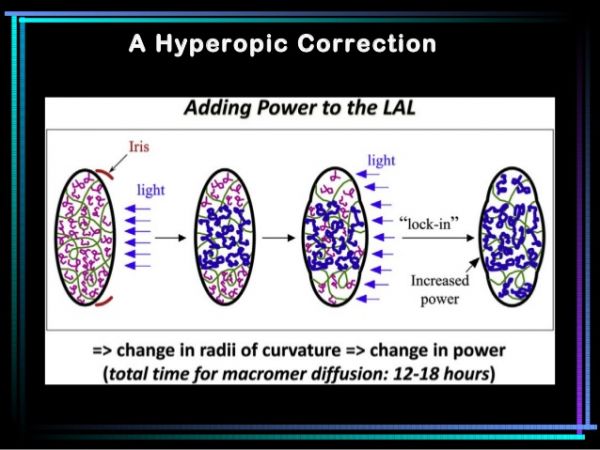
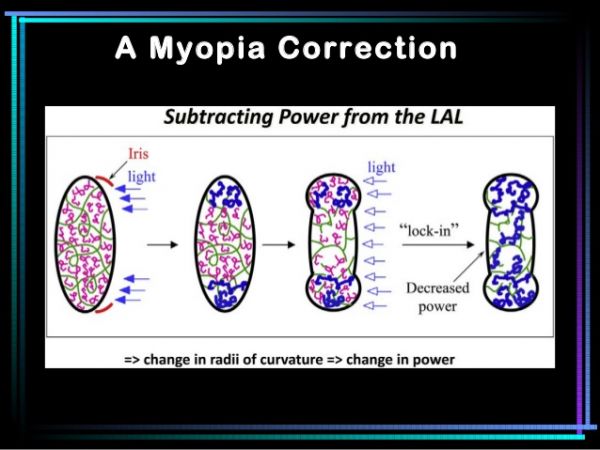
Light adjustability of the lens is based on the principles of photochemistry and diffusion. The LAL incorporates photosensitive molecules known as macromers embedded uniformly in a silicone matrix. When light (365 nm wavelength UV light) is directed to a specific area of the lens, macromers in the path of the light get activated and attach to the ends of other macromers forming polymers. This polymerization creates a concentration gradient between the irradiated region and the rest of the optic. Over a 12 hour period, the remaining unexposed macromers physically diffuse into the exposed area until there is no concentration gradient, causing an highly predictable change in the lens curvature and the refractive power change of the the lens. Light treatments can simultaneously be targeted to perform spherical and cylindrical adjustments. As long as there are untreated macromers further adjustments to refine the corrections can be made by directing light to different areas of the lens. When the adjustment process has been perfected to the satisfaction of the surgeon and the patient, the entire lens is exposed to the treatment light to polymerize all remaining macromers effectively locking them in place to prevent any further changes.
Patient Selection
Indications
FDA approved the LAL for human use on 22 November 2017.
- Well motivated patients with cataract and corneal astigmatism of at least 0.75 diopters (D), without any significant anterior or posterior segment pathology.
Contraindications
LAL should not be advocated in the following situations:
- Pre-existing macular disease
- Prior history of herpes eye infection
- Intake of medications that increase the sensitivity to ultraviolet (UV) light
- Intake of retino-toxic medications (example: Tamoxifen)
- patients with nystagmus
- Poor patient compliance to the postoperative schedule for adjustment and lock-in treatment and to the instructions of wearing UV protective glasses for several weeks following the surgery.
Drugs that increase sensitivity to UV light include:
Tetracycline
Doxycycline
Psoralens
Amiodarone
Phenothiazines
Chloroquine
Hydroxychloroquine
Piroxicam
Ketoprofen
Lomefloxacin
Methoxsalen
Lens specification
Lens optic
- 'Material: photo-reactive UV-absorbing silicone
- Light transmission for all lens power: UV cut-off at 10 percent T 385±2 nm
- Index of refraction :1.43
- Power: +10.0 D to +15.0 D and +2.0 D to +30.0 D in 1 D increments : +16.0 to +24.0 D in 0.5 D increments
- Optic type : Biconvex
- Optic edge: round on anterior surface and square on posterior surface
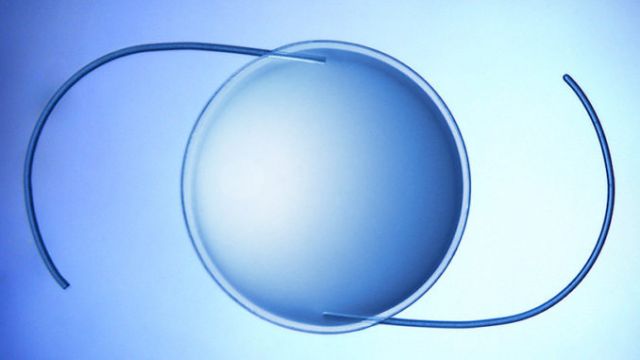
- Overall diameter: 13 mm
- Optic diameter: 6 mm
Haptic
- Configuration: modified C
- Material: blue core polymethylmethacrylate (PMMA) monofilament
- Haptic angle: 10 degrees'
These features prevent posterior capsular opacification and rotation of IOL within the capsular bag, which makes the IOL suitable for toric correction.
The IOL has UV light filtering material concentrated along the posterior aspect of the optic which protects the retina during overexposure to UV radiation during adjustments and lock-in treatments.
Surgical Technique
Prior to surgery, routine baseline measurement to determine the monofocal base power is performed. The surgical procedure of cataract surgery and placement of LAL in the capsular bag is similar to any other standard IOL implantation procedure. After the eye heals (2 -4 weeks after IOL implantation), refraction is done. Based on the refraction and the lifestyle requirements, a custom prescription is formulated for the patient following which a UV light induced customization of the IOL is accomplished with the help of a in-office Light Delivery Device (LDD) in a quick and painless procedure. the LDD is basically an anterior segment biomicroscope with additional optical projection system, electronic control circuit, and a UV light source. The UV light is focused on the IOL with the help of a contact lens placed over the cornea.
The optic is irradiated either in the central region or the peripheral region based on the power change required.
If the doctor wishes to add power in order to treat hyperopia then the central portion of the lens is illuminated and if there is a need to take away power then the peripheral part of the optic is irradiated to increase the peripheral curvature of the lens resolving the myopic refractive error. Similarly, different meridians can be selectively treated to correct astigmatism. Adjustment range varies from -2 D to + 2 D Sphere and from -0.5 to -3.0 D Cylinder. The number of light treatments required to achieve the desired power can range from 2 to 4 , each lasting for approximately 40- 120 seconds (mean of 90 seconds) and separated by approximately 3 days. After the best possible vision has been achieved and the refraction is verified, the entire optic is exposed to UV light to "lock in " the power. It is important to note that all the light adjustments are to be done with a pupil dilatation of around 7 mm as the optic of LAL is 6 mm in diameter.
In order to prevent uncontrolled polymerization of the silicone macromers with unpredictable changes in IOL power from incidental exposure to indoor or outdoor sources of UV light before the lock-in step, the protocol requires the patient to don UV protective glasses during all waking hours of the day right from the time of the surgery, all through the healing and light treatment process , till 24 hours after the final light treatment. Glasses may be removed while sleeping, and may also be temporarily taken off while applying eye drops and taking a shower as long as the patient is not exposed to direct sunlight.
A day after the final treatment , no further changes can be made in the lens power. The patient can discontinue wear of the UV protective glasses and enjoy his customized vision.
Advantage
- Simplifies preoperative decision making regarding the type of lens required as the power of the eye can be optimized in accordance with the manifest refraction after surgery.
- Eliminates the need for preoperative axis marking for astigmatism, wavefront aberrometry, multiple advanced formulae for accurate biometry and intraoperative aberrometry.
- They clearly minimize the error from inaccurate biometry, power calculation, and post-implantation IOL movement. In toric IOL even after meticulous calculation of posterior corneal astigmatism, surgically induced astigmatism, preoperative and inoperative digital alignment, 8-18% of the cases showed a post op rotation of more than 5 degrees.[1] Using LAL to correct astigmatism 3 weeks post operatively when the eye has completely healed and the lens is locked into position due to capsular contraction, circumvents a lot of these problems.
- A additional advantage o f these lens is the consistency in delivering refractive accuracy . According to the EUREQUO study which published the data of 2,80,000 patients from 100 clinics, 27% of eyes failed to land within 0.5 D sphere of the refractive target. This scenario has been changed with the introduction of LAL where more precision could be achieved in a more reproducible manner.91.6 percent of patients procured 20/25 without glasses. [2] After adjustments 92 percent of the patients were within 0.5 D and 99.5 percent were within 1 D of the intended refraction. In terms of toric adjustments 82 percent of the subjects had a maximum of 0.5 D astigmatism at 6 months and 98.5 percent had a maximum astigmatism of 1 D.[3]
- With regards to post operative refractive adjustments LAL enjoys a supremacy over procedures like PRK or LASIK in terms of the interval required between the primary surgery and the final adjustments to the refractive power of the eye. For keratorefractive procedure post cataract surgery one needs to wait for a period of 3 months for the wounds to stabilize, whereas with light assisted adjustments of the optic can be initiated at three weeks postop. The concern pertaining to post operative surprises after keratorefractive procedures linked to the variability of how corneal epithelium and stroma heals is obliterated, as there is not much variability in how the LAL heals. Moreover the later is a noninvasive procedure ensuring better patient satisfaction.
- Provides a predictable approach to provide desired refraction in cases of cataract surgery post corneal refractive procedures. This was clearly demonstrated in a retrospective study by Brierley conducted on 34 post refractive surgery eyes of 21 patients all of whom underwent LAL. The manifest refraction spherical equivalent (MRSE) relative to target refraction after the completion of the procedure was within ±0.25 D in 74% eyes , within ±0.50 D in 97% eyes and within ±1.00 D in 100% eyes.[4]The results demonstrated by Brierley were 60% more predictable than the visual outcomes achieved by monofocal lens implantation in postrefractive surgery patients in previous studies.
- Light adjustable IOL is a novel way to deliver customized monovision.
Disadvantage/Concerns
- LALs are premium IOL so that comes with an extra cost. This technology comes with an extra fee for the work that is involved.
- The procedure can be challenging in settings of poor pupillary dilatation. Light adjustments require full view of the optic of the lens so the pupil should be dilated to a minimum of 6.5 - 7 mm. In cases where this dilatation cannot be achieved, there will be a portion of the lens periphery that remains behind the iris containing untreated macromers.
- The corneal astigmatism can change over time which might effect the permanence of the vision provided by the LAL. To overcome this hurdle there has been a proposal to combine adaptive optics with LAL, which will allow the device to detect and compensate for optical distortions.[5]
Outcomes
In a FDA study conducted among 600 participants , those who received the LAL followed by adjustments were twice as likely to achieve an uncorrected distance vision of 20/20 at 6 months when compared to those who received a standard mono focal IOL.[3]
Researchers are continuing to study the effects and the visual outcomes of LAL implantation . The lens has shown great potential and will undoubtedly play a significant role in shaping the refractive outcome of cataract surgery.
Complications
All the risks associated with cataract surgery and intraocular lens implantation can be present.
- Adverse effects unique to LAL, primarily due to the UV light exposure procedures are erythropsia (red-tinted vision) and alterations in color vision (difficulty in distinguishing between blue, violet and green). Both these conditions tend to resolve once the adjustments are completed . Corneal abrasions due to faulty handling of the contact lens during LDD assisted adjustments have also been reported. There is also a potential risk of UV light induced retinal damage which may occur due to over exposure as a result of the filter dysfunction in the LDD.
- Minor complications include temporary dryness of eye and activation of an preexisting herpetic eye disease. The adverse effects that emerged in the FDA study was that 1.7% of the subjects required a secondary surgical intervention(SSI). These SSIs included explantation of IOL 3 weeks post operatively due to a scratch in the optic, an endothelial keratoplasty done to treat corneal edema during the initial implantation procedure, wound leak repairs, iridectomy or vitreous aspiration for pupillary blocks and a barrage for retinal tear.
References
- ↑ Lee BS, Chang DF Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmology.2018;125(9):1325-1331.
- ↑ Lundstrom M, et al. Risk factors for refractive error after cataract surgery: analysis of 282,811 cataract extractions reported to the European Registry of Quality Outcomes of Cataract and Refractive Surgery. J cataract Refract Surg. 2018:44;447-42.
- ↑ 3.0 3.1 FDA.gov.LAL Summary of Safety and Effectiveness. https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160055B.pdf. Accessed 11 December 2017
- ↑ Brierley L. Refractive results after implantation of a light-adjustable intraocular lens in postrefractive surgery cataract patients. Ophthalmology.2013;120:1968-1972.
- ↑ Artal, P, Guirao, A, Berrio, E, et al. Compensation of corneal aberration by the internal optics in the human eye. J Vis 2001;1:1-8.