Femtosecond Lasers and Laser Assisted in Situ Keratomileusis (LASIK)
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
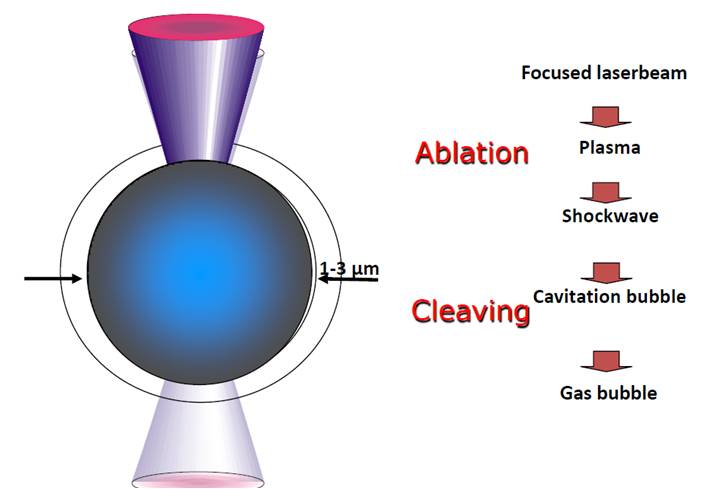
Femtosecond (FS) laser is an infrared laser with a wavelength of 1053nm. FS laser like Nd: YAG laser works by producing photodisruption or photoionization of the optically transparent tissue such as the cornea[1]. Application of either FS laser or Nd:YAG laser results in the generation of a rapidly expanding cloud of free electrons and ionized molecules. The acoustic shock wave so generated results in disruption of the treated tissue[2] (figure 1). However, the two lasers differ significantly in the amount of collateral damage they cause. Nd:YAG laser has a pulse duration in the nanosecond range (10-9 second) where as FS laser has pulse duration in the femtosecond range (10-15 second). Reducing the pulse duration reduces the amount of collateral tissue damage. In fact, collateral damage with FS laser is 106 times less than with the Nd:YAG laser[3] [4]. This makes FS laser safe for use in corneal surgeries which require exquisite precision.
Fig 1. FS laser induced photodisruption (courtesy Alcon Laboratories)
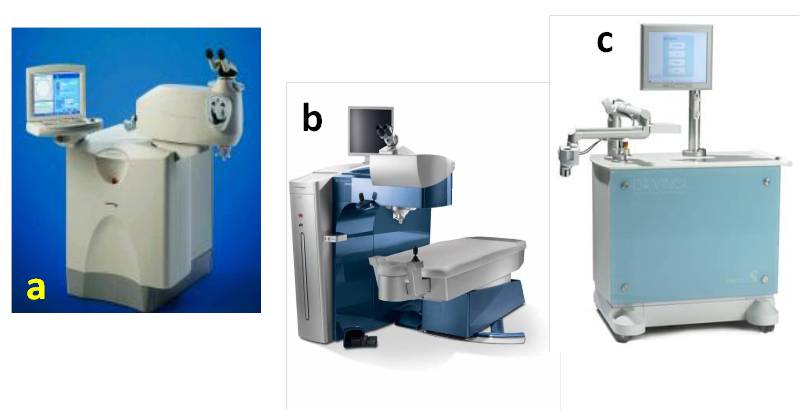
The first Ophthalmic FS laser system was designed by Dr Juhsaz in collaboration with Dr Kurtz at the University of Michigan in the early 1990s[2]. Currently many different FS laser systems are available commercially (figure 2) viz. 1) IntraLase (Abbott Medical Optics Inc, Santa Ana, California); 2) Femtec (20/10 Perfect Vision, Heidelberg, Germany); 3) Femto LDV (Ziemer Ophthalmic Systems, Port, Switzerland); 4) VisuMax (Carl Zeiss Meditec AG, Jena, Germany); 5) WaveLight FS200 (Alcon Laboratories Inc, Ft Worth, Texas); 6) VICTUS (Bausch & Lomb, Rochester, NY) ); and 7) LenSx (Alcon Laboratories Inc, Ft Worth, Texas) . The aforementioned laser systems differ in available applications, pulse energy and frequency, applanation surface (flat or curved) and laser delivery pattern (raster/zigzag or centrifugal/spiral)[5]
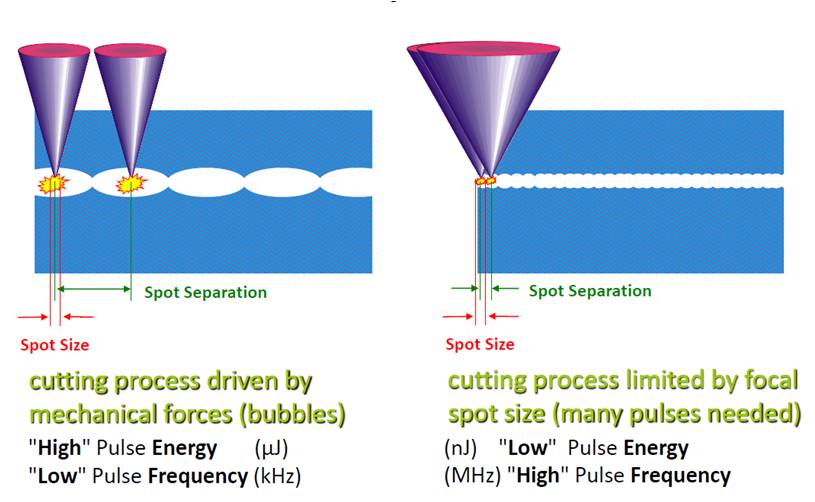
[6]. The technology of FS laser has evolved significantly from its introduction. Laser firing frequency has increased from 10-kHz in 2002 to 150-kHz in fifth generation IntraLase FS system[2][7] [8]. Femto LDV operates in the mHz firing rate range, rather than kHz[2]. The higher frequency allows reduced flap creation time and lower energy per pulse leading to a smoother corneal stromal bed[6] (figure 3).
Fig 2 Different commercially available FS laser systems (a) IntraLase (Abbott Medical Optics Inc, Santa Ana, California), (b) WaveLight FS200 (Alcon Laboratories Inc, Ft Worth, Texas), (c) Femto LDV (Ziemer Ophthalmic Systems, Port, Switzerland) [courtesy Alcon Laboratories]
Fig 3. Low frequency versus high frequency laser application. High frequency laser allows use of lower energy per pulse (courtesy Alcon Laboratories)
Clinical applications
FS laser has a wide range of applications in corneal refractive surgery[6]. This includes LASIK flap creation, astigmatic keratotomy (AK), channel creation for implantation of intrastromal corneal ring segments (ICRS), presbyopia correction, femtosecond lenticule extraction (FLEx), small-incision lenticule extraction (SMILE), and intrastromal presbyopia correction (INTRACOR)[5][9] [10] [11] [12]. Besides FS lasers are also being used in laser-assisted anterior and posterior lamellar keratoplasty, cutting of donor buttons in endothelial keratoplasty, customized trephination in penetrating keratoplasty, wound construction, capsulorrhexis in cataract surgery, and nuclear fragmentation in cataract surgery[13] [14] [15] [16]. In this article, we will discuss the application of FS laser in LASIK surgery.
LASIK flap creation
The suction ring is centered over the pupil and suction is applied once proper centration of the ring has been ensured and verified. The docking procedure is then initiated while keeping the suction ring parallel to the eye. An applanating glass contact lens is used to stabilize the globe and to flatten the cornea. It is important to achieve complete applanation of the cornea to avoid an incomplete flap or other flap related complications. Once the laser’s computer has confirmed centration, the surgeon administers the FS laser treatment. Each pulse of the laser generates free electrons and ionized molecules leading to formation of microscopic gas bubbles dissipating into surrounding tissue. Multiple pulses are applied next to each other to create a cleavage plane and ultimately the LASIK flap. Suction is then released. A spatula is carefully passed across the flap starting at the hinge and sweeping inferiorly to lift the flap for excimer laser ablation.
Advantages
More than 55% of all LASIK procedures in 2009 were performed with FS laser[5]. The number was 30% in 2006[19]. FS laser offers several advantages over the conventional microkeratomes and is gaining popularity across the globe.
Major advantages of FS laser[17][20] [21] [22] [23] [24] [25] [26]
- Reduced incidence of flap complications like buttonholes, free caps, irregular cuts etc
- Greater surgeon choice and control over flap diameter and thickness, side cut angle, hinge position and length
- Increased precision with improved flap safety and better thickness predictability
- Capability of cutting thinner flaps to accommodate thin corneas and high refractive errors
- Absence of moving parts
Other advantages include stronger flap adherence, better contrast sensitivity, decreased incidence of epithelial ingrowth, less increase in IOP required, lesser incidence of dry eyes, lesser hemorrhage from limbal vessels less likely, and the ability to retreat immediately if there is incomplete FS laser ablation[27] [28]. Loss of suction during FS laser LASIK flap creation is easier to handle and the suction ring may be reapplied and treatment resumed immediately in many cases[29]. Studies have shown FS laser to be safe and the visual and the refractive outcomes of FS laser LASIK have been shown to be superior to microkeratome LASIK in myopia[30], hyperopia[31] and astigmatism correction.[32]
Disadvantages and Unique Complications
As described above, FS laser has a lot of advantages over microkeratome LASIK and is gaining more and more acceptance worldwide. However, the technique presents with its unique set of disadvantages and related complications[33]. Flap creation with FS laser usually takes longer than microkeratome LASIK, however newer high frequency FS lasers have overcome this disadvantage. Some of the more significant complications unique to FS laser are
- Opaque bubble layer (OBL): Gas bubbles routinely accumulate in the flap interface during FS laser treatment, but occasionally they may dissect into the deep stromal bed. This may interfere with the ability of the excimer laser eye tracker device for tracking and registration. Bubbles may escape into the corneal sub-epithelial space, which is usually innocuous, but larger central vertical gas breakthrough may potentially result in a flap buttonhole[34]. Conversely the bubbles may seep into the anterior chamber by dissecting through the trabecular meshwork[35]. The incidence of OBL can be reduced by use of the raster or centripetal spiral patterns and peripheral gutters programmed into the cut.
- Transient light sensitivity syndrome (TLSS): Also called as good acuity plus photosensitivity (GAPP). TLSS usually occurs days to weeks after FS laser LASIK. Patients present with extreme photophobia and good visual acuity with paucity of clinical findings on exam. It resolves without sequel but requires aggressive topical steroids for weeks[36]. Proposed mechanism is either an inflammatory response of the surrounding tissue to the gas bubbles or biochemical response of the keratocytes to the near-infrared laser energy.
- Micro-irregularities on the back surface of the FS laser LASIK flap can cause “rainbow glare”[37]. Patients complain of colored bands of light radiating from a white light source. These glares are usually inconsequential in terms of their visual impact.
- Photodisruption-induced microscopic tissue injury and ocular surface inflammatory mediators may cause lamellar keratitis in the flap interface[38]. Lamellar keratitis tends to have little effect on visual acuity but flap necrosis following this complication has been reported in literature[39]. Lamellar keratitis after LASIK with the FS laser flap creation usually resolves with minimal sequelae. The mild effect on visual acuity usually persists for less than one week after the surgery[40]. This lamellar inflammation differs from microkeratome LASIK diffuse lamellar keratitis because the location of stromal inflammation is in the flap anterior stroma and corticosteroid treatment seemed to have little effect on outcomes[6]. Other disadvantages include increased cost, need to acquire a new skill on the part of the surgeon, increased difficulty in lifting the flap if retreatment is required, and a low risk of interface haze and interface stromal irregularities.
Conclusions
FS laser is being widely used in various ophthalmic surgical procedures. Advances in technology like lower energy systems with faster firing rates will increase the versatility and precision of the laser systems. This will further reduce ancillary tissue damage and make the surgery safer. As with any other technology, competition will likely bring down the cost of the equipment making the price per case less expensive. FS lasers hold great promise and its applications are continuing to evolve and expand in ophthalmology.
Additional Resources
- American Academy of Ophthalmology. LASIK. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/treatments/lasik-2. Accessed July 11, 2024.
References
- ↑ Chung SH, Mazur E. Surgical applications of femtosecond laser. J Biophotonics. 2009;2(10):557-572.
- ↑ 2.0 2.1 2.2 2.3 2.4 Soong HK et al. Femtosecond Lasers in Ophthalmology. Am J Ophthalmol 2009;147:189-197.
- ↑ Stern D, Schoenlein RW, Puliafito CA et al. Corneal ablation by nanosecond, picosecond, and femtosecond lasers at 532 and 625 nm. Arch Ophthalmol. 1989;107(4):587-592.
- ↑ Ratkay-Traub I, Ferincz IE, Juhasz T, et al. First clinical results with the femtosecond neodymium-glass laser in refractive surgery. J Refract Surg 2003;19:94 –103.
- ↑ 5.0 5.1 5.2 Binder PS. Femtosecond applications for anterior segment surgery. Eye Contact Lens. 2010;36(5):282-285.
- ↑ 6.0 6.1 6.2 6.3 6.4 Kymionis GD, Reinstein DZ et al. Femtosecond Laser Technology in Corneal Refractive Surgery: A Review. J Refract Surg. 2012 Dec;28(12):912-20.
- ↑ Ratkay-Traub I, Juhasz T, Horvath C, et al. Ultra-short pulse (femtosecond) laser surgery: initial use in LASIK flap creation. Ophthalmol Clin North Am. 2001;14(2):347-355.
- ↑ Hjortdal J, Nielsen E, Vestergaard A, Søndergaard A. Inverse cutting of posterior lamellar corneal grafts by a femtosecond laser. Open Ophthalmol J. 2012;6:19-22.
- ↑ Schanzlin DJ, Asbell PA, Burris TE, Durrie DS. The intrastromal corneal ring segments: phase II results for the correction of myopia. Ophthalmology. 1997;104(7):1067-1078.
- ↑ Abbey A, Ide T, Kymionis GD, Yoo SH Femtosecond laser-assisted astigmatic keratotomy in naturally occurring high astigmatism. Br J Ophthalmol. 2009;93(12):1566-1569.
- ↑ Seyeddain O, Riha W, Hohensinn M, Nix G et al. Refractive surgical correction of presbyopia with the Acufocus small aperture corneal inlay: two-year follow-up. J Refract Surg. 2010;26(10):707-715.
- ↑ Sekundo W, Kunert K, et al. First efficacy and safety study of femtosecond lenticule extraction for the correction of myopia: six-month results. J Cataract Refract Surg. 2008;34(9):1513-1520.
- ↑ Yoo S, Kymionis G, Koreishi A, et al. Femtosecond laser assisted sutureless anterior lamellar keratoplasty. Ophthalmology. 2008;115:1303–1307.
- ↑ Seitz B, Langenbucher A, Hofmann-Rummelt C, et al. Nonmechanical posterior lamellar keratoplasty using the femtosecond laser (femto-plak) for corneal endothelial decompensation. Am J Ophthalmol 2003;136:769–772.
- ↑ Soong HK, Mian S, Abbasi O, Juhasz T. Femtosecond laser assisted posterior lamellar keratoplasty: Initial studies of surgical technique in eye bank eyes. Ophthalmology 2005;112:44–49.
- ↑ Roberts TV, Lawless M, Chan CC, Jacobs M, et al. Femtosecond laser cataract surgery: technology and clinical practice. Clin Experiment Ophthalmol. 2013 Mar;41(2):180-6.
- ↑ 17.0 17.1 Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront guided laser assisted in situ keratomileusis: prospective contralateral eye study. J Cataract Refract Surg. 2005;31(1):120-126.
- ↑ Holzer MP, Rabsilber TM et a. Femtosecond laser-assisted corneal flap cuts: morphology, accuracy and histopathology. Invest Ophthalmol Vis Sci. 2006;47(7):2828-2831.
- ↑ 19.0 19.1 Slade SG. The use of the femtosecond laser in the customization of corneal flaps in laser in situ keratomileusis. Curr Opin Ophthalmol. 2007;18(4):314-317.
- ↑ Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical microkeratomes for laser in situ keratomileusis. J Cataract Refract Surg 2004;30:804–811.
- ↑ Talamo JH, Meltzer J, Gardner J. Reproducibility of flap thickness with IntraLase FS and Moria LSK-1 and M2 microkeratomes. J Refract Surg.. 2006;22(6):556-561.
- ↑ Rocha KM, Randleman JB, Stulting RD. Analysis of microkeratome thin flap architecture using Fourier-domain optical coherence tomography. J Refract Surg. 2011;27(10):759-763.
- ↑ Sutton G, Hodge C. Accuracy and precision of LASIK flap thickness using the IntraLase femtosecond laser in 1000 consecutive cases. J Refract Surg. 2008;24(8):802-806.
- ↑ Stahl JE, Durrie DS, Schwendeman FJ et al. Anterior segment OCT analysis of thin IntraLase femtosecond flaps. J Refract Surg. 2007;23(6):555-558.
- ↑ Lim T, Yang S et al. Comparison of IntraLase femtosecond laser and mechanical microkeratome for laser in situ keratomileusis. Am J Ophthalmol 2006;141(5):189-197.
- ↑ Patel SV, Maguire LJ et al. Femtosecond laser versus mechanical microkeratome for LASIK: a randomized controlled study. Ophthalmology. 2007;114(8):1482-1490.
- ↑ Salomão MQ, Ambrosio R Jr, Wilson SE. Dry eye associated with laser in situ keratomileusis: mechanical microkeratome versus femtosecond laser. J Cataract Refract Surg. 2009;35(10):1756- 1760.
- ↑ Netto MV, Mohan RR, Medeiros FW, et al. Femtosecond laser and microkeratome corneal flaps: comparison of stromal wound healing and inflammation. J Refract Surg. 2007;23(7):667-676.
- ↑ Ide T, Yoo SH, Kymionis GD, Haft P, O’Brien TP. Second femtosecond laser pass for incomplete laser in situ keratomi- leusis flaps caused by suction loss. J Cataract Refract Surg. 2009;35(1):153-157.
- ↑ Kanellopoulos AJ, Asimellis G. Long-term bladeless LASIK outcomes with the FS200 Femtosecond and EX500 Excimer Laser workstation: the Refractive Suite. Clin Ophthalmol 2013; 7: 261-9.
- ↑ Gil-Cazorla R, Teus MA, de Benito-Llopis L, Mikropoulos DG. Femtosecond laser vs mechanical microkeratome for hyperopic laser in situ keratomileusis. Am J Ophthalmol 2011; 152: 16-21
- ↑ . Raoof-Daneshvar D, Mian SI. Femtosecond Laser-Assisted Astigmatism Correction, Astigmatism - Optics, Physiology and Management. [online] 2012 [cited 2015 September 17]. Available from: URL: http://www.intechopen.com/books/astigmatism-optics-physiology-and-management/femtosecond-laser-assisted-astigmatism-correction.
- ↑ Chang JS. Complications of sub-Bowman’s keratomileusis with a femtosecond laser in 3009 eyes. J Cataract Refract Surg.2008;24(1):S97-S101.
- ↑ Srinivasan S, Herzig S. Sub-epithelial gas breakthrough during femtosecond laser flap creation for LASIK. Br J Ophthalmol.2007;91(10):1373.
- ↑ Srinivasan S, Rootman DS. Anterior chamber gas bubble formation during femtosecond laser flap creation for LASIK. J Refract Surg. 2007;23(8):828-830.
- ↑ Stonecipher KG, Dishler JG, Ignacio TS, Binder PS. Transient light sensitivity after femtosecond laser flap creation: clinical findings and management. J Cataract Refract Surg.2006;32(1):91-94.
- ↑ Krueger RR, Thornton IL, Xu M, Bor Z, van den Berg TJ. Rainbow glare as an optical side effect of IntraLASIK. Ophthalmology.2008;115(7):1187-1195.
- ↑ Gil-Cazorla R, Teus MA et al. Incidence of diffuse lamellar keratitis after laser in situ keratomileusis associated with the IntraLase 15 kHz femtosecond laser and Moria M2 microkeratome. J Cataract Refract Surg.2008;34(1):28-31.
- ↑ Hainline BC, Price MO et al. Central flap necrosis after LASIK with microkeratome and femtosecond laser created flaps. J Refract Surg. 2007;23(3):233-242.
- ↑ de Paula FH, Khairallah CG, Niziol LM, et al. Diffuse lamellar keratitis after laser in situ keratomileusis with femtosecond laser flap creation. J Cataract Refract Surg. 2012;38(6):1014-1019.