Contact Lenses
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Contact lenses are clear and rounded disks with curved edges placed on the surface of the eye. Types of contact lenses can be classified by function, material, and design. Functionally, they can be used for corrective, therapeutic, operative, and decorative purposes.
Contact lenses are also helpful for practical purposes such as comfort without the weight of spectacles, during weather conditions (e.g. fog, snow, rain), sports, or in critical situations for first responders or police personnel in which spectacles may be displaced.[1][2][3][4]
History of Contact Lenses
Initial Concepts
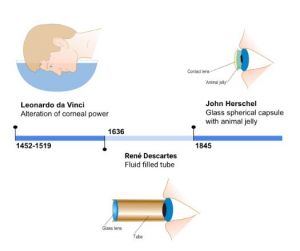
The initial concept of contact lenses is thought to have originated in the 16th century, with Leonardo da Vinci’s Codex of the Eye, Manual D. Da Vinci noted that placing one’s head in a container of water could change corneal power.[5] In the 17th century, René Descartes proposed that refraction could be altered using a fluid-filled tube with a glass lens at the end. A more practical lens design was suggested by Sir John Herschel in the mid-1800s. He correctly suggested that astigmatism could result from severe corneal abnormalities and theorized that it could be corrected by placing an animal jelly-filled, spherical capsule on the cornea.[6][7][8] While frequently attributed to Herschel, other inventors, unaware of Herschel’s ideas, discovered that a contact lens could be crafted by taking a mold of the cornea and transposing it to a transparent medium.
Glass
Contact lens research proliferated in the 1880s. It has been debated who fitted the first contact lens. In 1888, Adolf Eugene Fick published a report of how he fitted a scleral contact lens made out of brown glass, without optical power, on rabbits, himself, and then six patients to correct astigmatism from corneal distortions. In 1889, August Müller was credited for fitting the first powered contact lens, which he used to correct his own myopia.[9][10]
Polymethyl methacrylate
Plastic scleral lenses composed of polymethyl methacrylate (PMMA) were first introduced in the U.S. in 1936.[11] The idea of using PMMA was brought to light by medical officers in World War II, who found that cockpit window fragments lodged in the eyes of injured military personnel remained inert years after.
Corrective spherical plastic lenses were developed by Kevin Tuohy, as a result of a lab error during the creation of a PMMA scleral lens. After more trials were conducted, the rigid corneal contact, or “hard” lens, was patented in 1948. While the initial rigid lens was non-gas permeable, the first rigid gas-permeable lenses were created using cellulose acetate butyrate. Later, in 1974, Norman Gaylord would also integrate silicone into PMMA to create silicone acrylates.[12][13]
Soft Lenses
Otto Wichterle was the first to produce soft lenses from hydroxyethyl methacrylate (HEMA) from which the patent to develop soft lenses was obtained by Bausch & Lomb. In 1972, they introduced soft lenses to the global market.[14]
Indications
Vision Correction
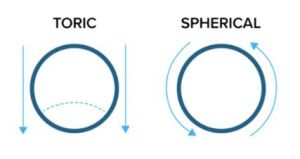
Corrective contact lenses may be purposed to help correct all orders of refractive aberration. Spherical contact lenses are used to correct second order aberrations including myopia and hyperopia. Spherical lenses, in principle, are cut from spheres such to focus light to a point with the same power in all directions.[15] Visual acuity in spherical contact lenses will not change no matter the orientation in the eye.
Soft Lenses
To correct for astigmatism, cylindrical lenses are cut from cylinders and focus light to a line at a specific axis.[16] When there is greater than 1.0 diopter of correctable cylinder power, toric lenses may be used to correct both spherical and cylindrical components of the refractive error. A toric lens, in principle, is cut from a torus (the shape of a donut), from which the lens is shaped like a football over the cornea. Toric contact lenses have been shown to improve vision for low to moderate astigmatism in comparison to spheric contact lenses.[17][18] The strongest soft contact lenses can correct for extreme degrees of myopia, with some lenses able to correct for more than -30 diopters. The highest level of corrective power for most regular soft contact lenses is usually around -12 diopters, but some monthly soft contact lenses can correct up to +/-20 diopters. Toric contact lenses can correct astigmatism up to -5.75 cylinder. Catalogs of contact lens option availability are released annually with detailed information on power ranges, sizes, and material properties (ex. link).
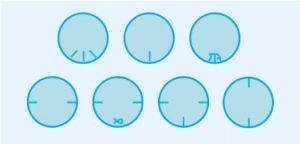
In contrast to spherical contact lenses, toric lenses must have their orientation set on the cornea such that rotation and axis misalignment are prevented. Toric lenses are made to be thicker, and therefore heavier, in certain areas of the lens to stabilize positioning on the eye.[19] These lenses often have scribe markings to indicate orientation allowing for assessment of lens rotation and stability.
Common toric designs for lens stabilization include prism ballast, peri-ballast, modified prism/peri-ballast, dual thin zone, and accelerated stabilization.[20][21] Each has different areas of thickness to stabilize the lens. In the diagram, blue shaded areas correspond to thicker parts of the lens.
a. Prism ballast
Prism-ballast lenses are thin superiorly and thicker inferiorly, which form a prism that is base-down within the optical zone. For stabilization, these lenses follow an effect frequently termed the ‘watermelon seed principle’ because the upper lid covers the thinner portion and pushes the thicker inferior portion towards the lower lid. This design may however be undesirable due to discomfort from lens interaction with the lids and decreased transmission of oxygen due to the thicker center and inferior areas of the lens.
b. Peri-ballast
Peri-ballast lenses are similar to prism-ballast lenses in that they are thinner superiorly and thicker inferiorly, however they are different in that the optical zone does not contain prism. Because the prism and peri-ballast lenses both have the base positioned at the inferior portion of the lens, they typically have a 6 o'clock lens marking.
c. Modified prism/peri-ballast
A ‘reversed’ prism design has been made to improve oxygen transmission and comfort by modifying the inferior portion of the lens to be thinner.
Thin zone and accelerated stabilization lenses are considered dynamic stabilization lens designs in which a thin zone is incorporated into both the inferior and superior areas of the lids for the eyelids to cover.
d. Thin zone
Thin zone lens designs have regions that are thinner superiorly and inferiorly with a thicker middle region. This enables the upper and lower eyelids to stabilize the lens when blinking. Thin zone designs will frequently have two markings in either the horizontal or vertical positions, as their orientation is the same in each axis.
e. Accelerated stabilization
Similar to thin zone lenses, accelerated stabilization has a thinner superior and inferior area but four thicker areas which act as “bumps,” creating four zones of stability. Like thin zone lenses, lens markings are frequently horizontal or vertical due to lens symmetry. The following figure demonstrates an example of an accelerated stabilization lens by ACUVUE.[22]
Rigid Gas Permeable Lenses
Rigid lenses are more durable and can provide better optical clarity than soft contact lenses.18 They are suitable for a wider range of patients, such as those with keratoconus, as they do not conform to the cornea. Patients may find them easier to insert and remove, however, they may take longer to get used to and require more stringent cleaning and care.[23] In terms of cost, they are also generally less expensive over time because they do not need to be replaced as often as soft lenses.
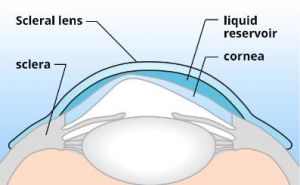
Scleral Lenses
Scleral contact lenses are rigid gas permeable lenses that vault over the cornea, rather than apposed to it, and rest on the conjunctiva. Both rigid gas permeable lenses and scleral lenses are used for vision correction. By vaulting over the cornea, scleral contact lens can provide a smooth surface for correcting high refractive error, astigmatism, and ectatic corneal diseases.[24][25] A liquid reservoir is also present to address surface diseases such as severe dry eye disease.
Myopic Prevention
Orthokeratology (Ortho-K) is a method of fitting rigid gas permeable lenses to be worn overnight, which temporarily reshapes the cornea, allowing the wearer to go without vision correction during the day.[26]
Presbyopia
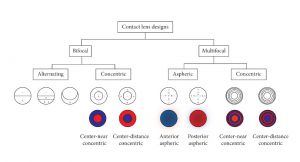
Presbyopia can be corrected with bi- or multifocal contact lenses or monovision correction.[27] There are two strategies for designing lenses that correct presbyopia: one is the alternating image method and the other is the simultaneous image method. [28]
The alternating image design has differing powers on separate vertical positions on the lens similar to a bifocal pair of glasses. The higher power portion of the corrective lens is typically designed to be inferior, so that when in down gaze subsequent translation of the lens superiorly results in the inferior portion of the lens to be in view, correcting presbyopia.
Simultaneous image contact lenses come in either concentric (bifocal or multifocal) or aspheric (multifocal) designs. Concentric designs feature a center of either near or far spherical correction surrounded by alternating rings of near and distance correction, whereas aspheric designs provide a progressive and gradual change of corrective power. These allow for the simultaneous presentation of both near and far images to the retina, relying on the user’s neural adaptation to choose the proper focus for the object in view.
A global study demonstrated that those 45 years and older were seldom using presbyopic contact lenses, suggesting that they are using reading spectacles.[29] This decreased use with older ages is attributed to infrequency of fittings in this group as well as age-dependent changes to the eyes which may influence contact lens use such as decreased eyelid tone, lacrimal secretion, and tear stability.[30][31]
Therapeutic
Bandage contact lenses
Bandage contact lenses are therapeutic plastic contact lenses that protect the cornea to allow healing of the epithelium.[32] They can relieve pain in the setting of corneal epithelial defects as well as prophylactically provide mechanical protection to the cornea after surgery (eg. from sutures irritation from the upper palpebral region), to the lid (eg. after corneal gluing), and help maintaining the position of an underlying graft (eg. conjunctival pedicle flap, amniotic membrane transplant, etc). They may also be used in a daily setting in conjunction with daily topical antibiotic drops in the setting of very severe dry eye syndrome associated with recurrent corneal erosions and persistent epithelial defects. These come in various sizes with diameters from 13.6 to 24 mm.
Scleral Lenses
In keratoconus, long-term scleral lens wear has been found to decrease the need for corneal transplant.[33] Scleral lenses can be used in limbal stem cell deficiency for visual rehabilitation.[34] See BostonSight PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem) and Scleral Contact Lenses for more information.
Design or Colored Lenses
Corrective and non-corrective contact lenses may be tinted to hide the appearance of an iris,[35] to reduce photophobia in albinism, aniridia, and achromatopsia,[36] to reduce nystagmus,[37][38] and to cosmetically alter eye color.
Prismatic Effect
In a prism ballast soft contact lens, classically, a minimal quantity of prism of approximately one prism diopter (PD) is grounded base down into the lens, utilizing gravity to keep the lens rotation base down. As a secondary effect, between two-thirds to the full amount of prism is translated onto the optical axis. A correction of up to four PD base down has been reported for vertical diplopia using custom prism-ballast soft contact lenses.[39] Incorporating prism for the purpose of diplopic correction is limited by lens thickness and tolerability.[40]
Rigid gas permeable (RGP) CTLs can correct small-angle vertical diplopia with an upper limit of approximately four PD base down. Recently, 3D-printed custom-molded or other rotationally stable scleral lenses have also been shown to incorporate up to four PD in any direction including horizontally (theoretically up to eight PD correction using four PD in each eye).[41]
Operative
Rigid gas permeable lenses may be placed on the operative cornea during microscopic surgery to improve visualization through a highly irregular corneal surface, often from corneal scarring.
Handheld lenses that make contact with the surface of the eye are used in the clinic and intraoperatively by surgeons for diagnosis, evaluation, and treatment of ocular diseases. See Gonioscopy and Lasers (surgery) for more information.
Decorative
Decorative contact lenses are frequently referred to as fashion, costume, and/or colored contact lenses.[42] however these products are also considered medical devices by the FDA.[43]
In 2005, it was established that all contact lenses fall under regulation as medical devices by the FDA and cannot be legally marketed as over the counter merchandise.[44] The FDA emphasizes that decorative lenses must be bought with a prescription, with appropriate fitting and evaluation of eyes for contact lenses. Otherwise, injury to the eye may result.
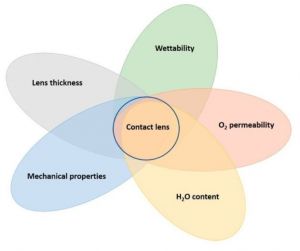
Materials
Contact lens materials differ in their water content, oxygen permeability, wettability, lens thickness, and mechanical properties.[45] Higher water content lenses are more fragile but have improved oxygen transport to the eye and increased comfort. Oxygen permeability is important especially for extended wear, as poor oxygen permeability can lead to hypoxia and corneal acidosis, limbal hyperemia, corneal vascularization, and epithelial thinning over time.[46] Oxygen permeability (Dk) is an intrinsic property of material and can be calculated by multiplying the diffusion coefficient (D) of the material with the oxygen solubility (k).[47] Oxygen transmissibility (Dk/t) takes into account the thickness (t) of a lens for a given design and provides a more clinically relevant measure. Wettability describes how well liquid spreads across the contact lens surface, which is influenced by the hydrophobic and hydrophilic components of the polymer material.[48] A high wetting angle (greater than 90 degrees) indicates that there are many dry spots, whereas a low wetting angle (lower than 90 degrees) indicates an even dispersion.[49] The combination of these factors result in lenses that vary in their comfort, wear time, handling, cost, and vision.
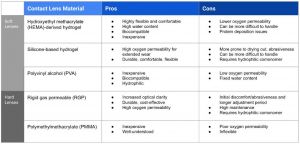
Soft Lenses
Soft lenses are highly flexible, allowing them to form to the cornea and provide increased comfort.[50] This means that their parameters for refractive correction are more limited when compared to rigid lenses.14 Hydroxyethyl methacrylate (HEMA) is a comfortable and inexpensive oxygen-permeable hydrogel with high water content suitable for those with drier eyes.[51][52] Silicone-based hydrogel lenses feature a higher oxygen permeability allowing for extended wear. They are currently the most common type of contact lens. Since silicone materials are naturally hydrophobic, manufacturers often combine them with hydrophilic comonomers to improve wettability. Polyvinyl alcohol (PVA) hydrogels are a newer material with high biocompatibility and hydrophilicity. PVA may leech from the lens to create an artificial tear film for comfortability.
Rigid "Hard" Lenses
Rigid gas permeable (RGP) lenses are made of multiple materials including fluoro silicone or siloxane acrylate moieties and hydrophilic monomers.[53] The first hard plastic contacts were made of polymethylmethacrylate (PMMA), an inflexible, non-gas permeable material, however gas permeable lenses are used much more commonly due to their better oxygen permeability.
Hybrid Lenses
Hybrid lenses consist of a rigid center and soft edges, providing the optical advantages of a hard lens with the comfort of a soft lens.[54] These are especially beneficial for patients with irregular corneas.
Wear Time
Per the FDA, “disposable” lenses are single-use lenses, used once prior to disposal. Soft contact lenses may be single-use (also referred to as “dailies”), extended-wear disposable, and scheduled replacement lenses.
Extended-wear lenses are either soft or RGP lenses which can be typically used for 7 days without removal and overnight.[55] However, there is an increased risk of complications with prolonged use. Extended-wear disposable lenses are soft lenses that can be worn typically 1-6 days then discarded and provide a decreased risk of infection from use. Current available scheduled replacement soft contact lenses in the market include every two weeks, monthly, or quarterly lenses. These lenses are removed daily and may be properly stored to reuse the next day from the time they are opened up until their end date.
Contraindications
Contact lenses should be avoided in those with ocular allergies, especially during seasonal allergic flares, vernal conjunctivitis, or giant papillary conjunctivitis, since the lens surface biofilm acts as an antigen depot, exacerbating ocular allergy symptoms.[56] Patients with conjunctivitis, uveitis, scleritis, superficial punctate keratitis, or corneal ulcers should not wear contact lenses (except for therapeutic lenses) as they may contribute to further irritation and prevent healing. Caution should be used in those who are predisposed to dry eye disease since contact lenses disrupt the tear film and introduce other changes to the corneal surface. Strabismus is a relative contraindication since contacts cannot incorporate more than approximately 8 PD to correct diplopia.[57] Other contraindications include the inability to properly handle and clean lenses and unsuitable working or living conditions.
Complications
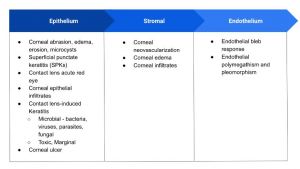
While contact lenses provide a multitude of benefits, complications from contact use are common.[58] Complications of contact lens use can be split into three categories–conjunctival, corneal, and other complications.[59] Conjunctival complications include allergic conjunctivitis, giant papillary conjunctivitis, and superior limbic keratoconjunctivitis. Corneal complications can be divided into epithelial, stromal, and endothelial as listed in the adjacent table.
Other complications include contact lens damage, discoloration, deposits, loss, and secondary eyelid ptosis.[60] See Contact Lens Complications for more information.
References
- ↑ Tyhurst K, McNett R, Bennett E. The safety and efficacy of contact lens wear in the industrial and chemical workplace. Optom - J Am Optom Assoc. 2007;78(11):596-604.
- ↑ Morehouse CA, Krecklow DE, Fisher JT, Welling TW, Morrison WE. Soft Contact Lenses for Sports. Phys Sportsmed. 1978;6(5):106-115.
- ↑ Sheedy JE. Contact lenses for police officers. J Am Optom Assoc. 1986;57(9):658-660
- ↑ Wells GA, Brown JJ, Casson EJ, Easterbrook M, Trottier AJ. To wear or not to wear: current contact lens use in the Royal Canadian Mounted Police. Can J Ophthalmol J Can Ophtalmol. 1997;32(3):158-162.
- ↑ Efron N. Contact Lens Practice. Butterworth-Heinemann/Elsevier; 2010.
- ↑ Efron N. Contact Lens Practice. Butterworth-Heinemann/Elsevier; 2010.
- ↑ Shaker LM, Al-Amiery A, Isahak WNRW. Revolutionizing contact lens manufacturing: exploring cutting-edge techniques and innovations for enhanced vision and comfort. Int J Low-Carbon Technol. 2024;19:359-385.
- ↑ Herschel JFW. Of the structure of the eye, and of vision. Encycl Metrop. 1845;4(Section XII, Light).
- ↑ Efron N. Contact Lens Practice. Butterworth-Heinemann/Elsevier; 2010.
- ↑ Efron N, Pearson RM. Centenary Celebration of Fick’s Eine Contactbrille. Arch Ophthalmol. 1988;106(10):1370-1377.
- ↑ Efron N. Contact Lens Practice. Butterworth-Heinemann/Elsevier; 2010.
- ↑ Efron N. Contact Lens Practice. Butterworth-Heinemann/Elsevier; 2010.
- ↑ US Patent for Oxygen permeable contact lens composition, methods and article of manufacture Patent (Patent # RE 31,406 issued October 4, 1983) - Justia Patents Search. Accessed August 25, 2024. https://patents.justia.com/patent/RE31406
- ↑ Efron N. Contact Lens Practice. Butterworth-Heinemann/Elsevier; 2010.
- ↑ Schwartz GS. The Eye Exam: A Complete Guide. SLACK Incorporated; 2006.
- ↑ Schwartz GS. The Eye Exam: A Complete Guide. SLACK Incorporated; 2006.
- ↑ Cox SM, Berntsen DA, Bickle KM, et al. Efficacy of Toric Contact Lenses in Fitting and Patient-Reported Outcomes in Contact Lens Wearers. Eye Contact Lens. 2018;44 Suppl 1:S296-S299.
- ↑ Chao C, Skidmore K, Tomiyama ES, Wolffsohn JS, Richdale K. Soft toric contact lens wear improves digital performance and vision—A randomised clinical trial. Ophthalmic Physiol Opt. 2023;43(1):25-34.
- ↑ Darling D. toric contact lenses. Accessed August 25, 2024. http://www.daviddarling.info/encyclopedia/T/toric_contact_lenses.html
- ↑ Lai N. TAKE A TURN WITH SOFT TORIC LENSES FOR ASTIGMATISM. PentaVision. Accessed August 25, 2024. https://clspectrum.com/issues/2019/september/take-a-turn-with-soft-toric-lenses-for-astigmatism/
- ↑ Optician Online - CPD Archive. Accessed August 25, 2024. https://www.opticianonline.net/cpd-archive/6485/
- ↑ Darling D. toric contact lenses. Accessed August 25, 2024. http://www.daviddarling.info/encyclopedia/T/toric_contact_lenses.html
- ↑ About Contact Lens Types | Healthy Contact Lens Wear and Care | CDC. Accessed August 25, 2024. https://www.cdc.gov/contact-lenses/about/about-contact-lens-types.html
- ↑ Bavinger JC, DeLoss K, Mian SI. Scleral lens use in dry eye syndrome. Curr Opin Ophthalmol. 2015;26(4):319.
- ↑ The Growing Role of Scleral Contact Lenses in Corneal and External Ocular Conditions - American Academy of Ophthalmology. Accessed August 25, 2024. https://www.aao.org/education/current-insight/growing-role-of-scleral-contact-lenses-in-corneal-
- ↑ Health C for D and R. Types of Contact Lenses. FDA. Published online August 15, 2023. Accessed August 25, 2024. https://www.fda.gov/medical-devices/contact-lenses/types-contact-lenses
- ↑ Charman WN. Developments in the correction of presbyopia I: spectacle and contact lenses. Ophthalmic Physiol Opt. 2014;34(1):8-29. doi:10.1111/opo.12091
- ↑ Remón L, Pérez-Merino P, Macedo-de-Araújo RJ, Amorim-de-Sousa AI, González-Méijome JM. Bifocal and Multifocal Contact Lenses for Presbyopia and Myopia Control. J Ophthalmol. 2020;2020(1):8067657.
- ↑ Morgan PB, Efron N, Woods CA, The International Contact Lens Prescribing Survey Consortium. An international survey of contact lens prescribing for presbyopia. Clin Exp Optom. 2011;94(1):87-92.
- ↑ Charman WN. Developments in the correction of presbyopia I: spectacle and contact lenses. Ophthalmic Physiol Opt. 2014;34(1):8-29. doi:10.1111/opo.12091
- ↑ Woods RL. The aging eye and contact lenses — a review of ocular characteristics. J Br Contact Lens Assoc. 1991;14(3):115-127
- ↑ Therapeutic Contact Lenses - ClinicalKey. Accessed July 31, 2024. https://www-clinicalkey-com.ezp2.lib.umn.edu/#!/content/3-s2.0-B978070207168300026X?scrollTo=%23c00026
- ↑ Koppen C, Kreps EO, Anthonissen L, Van Hoey M, Dhubhghaill SN, Vermeulen L. Scleral Lenses Reduce the Need for Corneal Transplants in Severe Keratoconus. Am J Ophthalmol. 2018;185:43-47.
- ↑ Kim KH, Deloss KS, Hood CT. Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) for Visual Rehabilitation in Limbal Stem Cell Deficiency. Eye Contact Lens. 2020;46(6):359.
- ↑ Coloboma | National Eye Institute. Accessed August 25, 2024. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/coloboma
- ↑ Vincent SJ. The use of contact lenses in low vision rehabilitation: optical and therapeutic applications. Clin Exp Optom. 2017;100(5):513-521.
- ↑ Saeed F, Schlange D, Najafi T. Sustained benefits of Therapeutic Tinted Contact Lenses (CL) in patients with Albinism. Invest Ophthalmol Vis Sci. 2013;54(15):2778.
- ↑ Theodorou M, Quartilho A, Xing W, et al. Soft Contact Lenses to Optimize Vision in Adults with Idiopathic Infantile Nystagmus: A Pilot Parallel Randomized Controlled Trial. Strabismus. 2018;26(1):11-21.
- ↑ Lam H, Zabrowski C, Lee M. Correction of vertical diplopia with soft contact lenses. Eye. 2022;36(3):639-640.
- ↑ Resultant vertical prism in toric soft contact lenses - PubMed. Accessed August 26, 2024. https://pubmed-ncbi-nlm-nih-gov.ezp1.lib.umn.edu/25823433/
- ↑ Vincent SJ, Fadel D. Optical considerations for scleral contact lenses: A review. Contact Lens Anterior Eye. 2019;42(6):598-613.
- ↑ Commissioner O of the. Colored and Decorative Contact Lenses: A Prescription Is A Must. FDA. Published online October 23, 2023. Accessed August 25, 2024. https://www.fda.gov/consumers/consumer-updates/colored-and-decorative-contact-lenses-prescription-must
- ↑ Commissioner O of the. Cosmetics & U.S. Law. FDA. Published online August 22, 2024. Accessed August 25, 2024.
- ↑ Health C for D and R. Decorative, Non-corrective Contact Lenses. March 19, 2020. Accessed August 25, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/decorative-non-corrective-contact-lenses
- ↑ Musgrave CSA, Fang F. Contact Lens Materials: A Materials Science Perspective. Materials. 2019;12(2):261.
- ↑ Michaud L. Understanding the Influence of Water Content in Soft Lenses. Review of Optometry. August 15, 2023. Accessed August 25, 2024. https://www.reviewofoptometry.com/article/understanding-the-influence-of-water-content-in-soft-lenses
- ↑ Galas S, Copper LL. Oxygen permeability of the pigmented material used in cosmetic daily disposable contact lenses. Clin Ophthalmol Auckl NZ. 2016;10:2469-2474.
- ↑ Sindt CW. The Modern Age of Surface Wettability. Review of Cornea & Contact Lenses. October 13, 2011. Accessed August 25, 2024.
- ↑ Musgrave CSA, Fang F. Contact Lens Materials: A Materials Science Perspective. Materials. 2019;12(2):261.
- ↑ Types of Contact Lenses. Accessed August 25, 2024. https://www.aoa.org/healthy-eyes/vision-and-vision-correction/types-of-contact-lenses?sso=y
- ↑ Musgrave CSA, Fang F. Contact Lens Materials: A Materials Science Perspective. Materials. 2019;12(2):261. doi:10.3390/ma12020261
- ↑ Musgrave CSA. Contact Lens Materials - A Materials Science Perspective. Scholarly Community Encyclopedia. January 27, 2022. Accessed August 25, 2024. https://encyclopedia.pub/entry/18834
- ↑ Musgrave CSA, Fang F. Contact Lens Materials: A Materials Science Perspective. Materials. 2019;12(2):261
- ↑ About Contact Lens Types | Healthy Contact Lens Wear and Care | CDC. Accessed August 25, 2024. https://www.cdc.gov/contact-lenses/about/about-contact-lens-types.html
- ↑ Types of Contact Lenses. Accessed August 25, 2024. https://www.aoa.org/healthy-eyes/vision-and-vision-correction/types-of-contact-lenses?sso=y
- ↑ Lemp MA, Bielory L. Contact lenses and associated anterior segment disorders: dry eye disease, blepharitis, and allergy. Immunol Allergy Clin North Am. 2008;28(1):105-117, vi-vii.
- ↑ Assessment of Patient Suitability for Contact Lenses - ClinicalKey. Accessed August 25, 2024.
- ↑ Alipour F, Khaheshi S, Soleimanzadeh M, Heidarzadeh S, Heydarzadeh S. Contact Lens-related Complications: A Review. J Ophthalmic Vis Res. 2017;12(2):193-204.
- ↑ Gurnani B, Kaur K. Contact Lens–Related Complications. In: StatPearls. StatPearls Publishing; 2024. Accessed July 31, 2024. http://www.ncbi.nlm.nih.gov/books/NBK587443/
- ↑ Alipour F, Khaheshi S, Soleimanzadeh M, Heidarzadeh S, Heydarzadeh S. Contact Lens-related Complications: A Review. J Ophthalmic Vis Res. 2017;12(2):193-204.