Bergmeister Papilla
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
ICD-10 Q14.2
Disease
The Bergmeister papilla was first reported by Austrian ophthalmologist Dr. Otto Bergmeister in 1877.[1][2] Also referred to as an epipapillary veil, it is a remnant of the fibrous sheath surrounding the fetal hyaloid artery during embryological development.[3]
Etiology
In the fetus, blood is supplied to various parts of the eye by the hyaloid artery. The hyaloid artery travels through the optic nerve head to the posterior aspect of the lens, where it branches into the tunica vasculosa lentis.[4] During normal development at around 30 weeks of gestational age, this blood supply is resorbed and develops into Cloquet’s (hyaloid) canal.[4][5][6] Incomplete resorption of these structures during development can result in persistent fetal vasculature, such as the Mittendorf dot and the Bergmeister papilla.[3] It is suspected that defects in genes guiding cell apoptosis result in persistent fetal vasculature.[4]
Diagnosis
History
Patients with Bergmeister papillae are often born premature, though many are born full term.[4]
Symptoms
Bergmeister papillae are typically asymptomatic and found incidentally. Changes to vision would depend upon association with secondary effects on the retina or macula.[4]
Diagnostic procedures
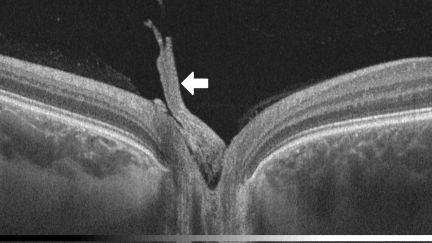
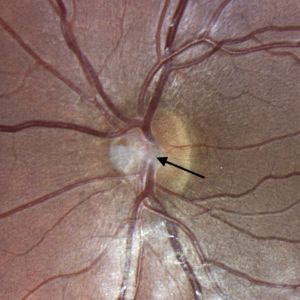
Bergmeister papillae can be observed with ophthalmoscopy and fundus photography (Figure 3), but they are more likely to be identified through optical coherence tomography (OCT) (Figure 1).[6][7][8] Visualization reveals a cluster of veil-like glial or fibroglial tissue emerging anteriorly, centrally, and nasally from the optic nerve head.[9][10][11] Presence of papillae can influence the size of the optic nerve head cup.[4] Bergmeister papillae can be unilateral or bilateral.[7]
Papillae can be vascularized by a retinal vessel, otherwise known as a prepapillary vascular loop. If it is vascularized, this can be visualized on fluorescein angiography (FA).[9] Without vascularization, the FA of a patient with Bergmeister papilla would be unremarkable.[3]
Differential diagnosis
The most important differential diagnosis is regressed (fibrosed) neovascularization of disc (NVD). Examination of the retina usually reveals retinal vascular disease (ischemic NVD) or inflammation (inflammatory NVD) in cases with NVD.[12] FA is useful in such cases to confirm NVD and to evaluate the retinal vascular status.
Management
General treatment
None indicated if Bergmeister papillae are without associated complications.
Prognosis
Prognosis is good in the vast majority of cases as the papilla itself is clinically insignificant. There have been reports of Bergmeister papilla associated with vitreoretinal adhesion and macular retinoschisis.[13][14] If a prepapillary vascular loop exists within the papilla, thrombosis of this vessel could cause vitreous hemorrhage, hyphema, branch retinal artery occlusion or branch retinal vein occlusion, though reports of these complications are rare.[15][16]
References
- ↑ Bergmeister O. Beiträge zur Entwicklungsgeschichte des Säugethierauges. Wien Embryologische Institut Mitteilungen. 1877;1:63-84.
- ↑ Royal Society of London. B. In: Catalogue of Scientific Papers (1800-1883) Supplementary Volume. Vol XII. Cambridge, UK: Cambridge University Press; 1902:72.
- ↑ 3.0 3.1 3.2 Orellana J, Friedman AH. Bergmeister's Papilla. In: Clinico-Pathological Atlas of Congenital Fundus Disorders. New York, New York: Springer; 1993:107-108. doi:10.1007/978-1-4613-9320-7_20
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Goldberg MF. Persistent fetal vasculature (PFV): An integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). Am J Ophthalmol. 1997;124(5):587-626. doi:10.1016/s0002-9394(14)70899-2
- ↑ Petersen HP. Persistence of the Bergmeister papilla with glial overgrowth. Acta Ophthalmol. 2009;46(3):430-440. doi:10.1111/j.1755-3768.1968.tb02826.x
- ↑ 6.0 6.1 Lin Q, Deng J, Ohno-Matsui K, He X, Xu X. The existence and regression of persistent Bergmeister's papilla in myopic children are associated with axial length. Transl Vis Sci Technol. 2021;10(13):4. doi:10.1167/tvst.10.13.4
- ↑ 7.0 7.1 Liu JJ, Witkin AJ, Adhi M, et al. Enhanced Vitreous Imaging in healthy eyes using swept-source optical coherence tomography. PLoS One. 2014;9(7):e102950. doi:10.1371/journal.pone.0102950
- ↑ Sherman J, Nath S, Sadun AA, Wong V, Delgado A, Boneta J, He W. Spectral OCT Reveals Bergmeister's papillae in the majority of normal, young patients. Investig Ophthalmol Vis Sci, 2008;49(13):929.
- ↑ 9.0 9.1 Bedell AJ, Jokl A. Epipapillary tissues. Trans Am Ophthalmol Soc. 1954;52:291-304.
- ↑ Roth AM, Foos RY. Surface structure of the optic nerve head. Am J Ophthalmol. 1972;74(5):977-985. doi:10.1016/0002-9394(72)91221-4
- ↑ Samuels B. Epipapillary tissues. Arch Ophthalmol. 1931;6(5):704-723. doi:10.1001/archopht.1931.00820070733006
- ↑ Kumawat BL, Chawla R, Venkatesh P, Tripathy K. Inflammatory optic disc neovascularisation managed with oral steroids/immunosuppressants and intravitreal ranibizumab. BMJ Case Rep. 2017;2017:bcr2017222262. Published 2017 Nov 3. doi:10.1136/bcr-2017-222262
- ↑ Ramesh SV, Ray P, Ramesh PV, Ramesh MK, Rajasekaran R. There’s more to a Bergmeister’s papilla than which meets the eye. J Clin Diagn Res. 2021;15(5):NJ01-NJ02. doi:10.7860/jcdr/2021/48931.14909
- ↑ Venkateswaran N, Moster SJ, Goldhagen BE. Bergmeister papilla with overlying traction. JAMA Ophthalmol. 2019;137(9):e185915-e185915. doi:10.1001/jamaophthalmol.2018.5915
- ↑ Brucker AJ, Michels RG, Fine SL. Congenital retinal arterial loops and vitreous hemorrhage. Am J Ophthalmol. 1977;84(2):220-223. doi:10.1016/0002-9394(77)90855-8
- ↑ Degenhart W, Brown G, Augsburger J, Magargal L. Prepapillary Vascular Loops. J Ophthalmol. 1981;88(11):1126-1131. doi:10.1016/s0161-6420(81)34894-5