Apocrine Hidrocystoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
2022 ICD-10-CM Diagnosis Code D23. 12: Other benign neoplasm of skin of left eyelid, including canthus.
Description
Apocrine hidrocystomas are benign cystic tumors that arise from apocrine sweat glands. [1] In 1964, Mehregan first described apocrine hidrocystomas as cystic proliferations of the apocrine glands found typically in the head and neck region.[2][1] Though the etiology of apocrine hidrocystoma is elusive, they are predominantly thought to arise from dysregulated tumorous growth of the secretory portion of apocrine glands. Clinicians may suspect the diagnosis of apocrine hidrocystoma through physical exam findings but the definitive diagnosis must be made histologically.[1]
Presentation
Apocrine hidrocystomas are frequently localized to the head and neck region as apocrine glands are found in higher concentrations in these regions. Apocrine glands differ from eccrine glands as they are adjacent to hair follicles which lead to the surface of the skin. Apocrine glands predominate in areas of abundant hair follicles such as the scalp, armpits, face and groin. And hence, apocrine hidrocystomas are also found more frequently in these areas. [3]
Apocrine hidrocystomas classically present as a firm, dome-shaped, blue-gray-purple hued cystic nodule. [4] These lesions are typically mobile upon palpation and they can be translucent with a typical size ranging from 3-15 mm.[5] Apocrine hidrocystomas do not follow any familial inheritance patterns and has been observed in adults aged 30 to 70 with an equal predilection for both men and women. These tumors rarely present in childhood or adolescence. [6]
Clinically, these lesions may present similarly to eccrine hidrocystomas, epidermal inclusion cysts, mucoid cysts, hemangioma and lymphangioma and should be considered in the differential diagnoses. Additionally, malignant lesions such as amelanotic melanoma and basal cell carcinoma may also present similarly to apocrine hidrocystomas making it imperative to have histological assessment of these lesions for correct diagnosis and timely treatment. [6]
Ophthalmological relevance
Apocrine Hidrocystomas are typically found in the head and neck region due to the high concentration of apocrine glands in these regions. These lesions can present on the upper or lower eyelids, eyebrow, medial or lateral canthi, or around the peri-orbital region. Associated symptoms of these lesions include eye irritation, itching, foreign body sensation, dry eyes and cosmetic impact for the patient. Though these lesions are benign, it can be difficult to diagnose definitively without histological assessment. In order to rule out malignancy, it is recommended that excised lesions be submitted for pathological review.
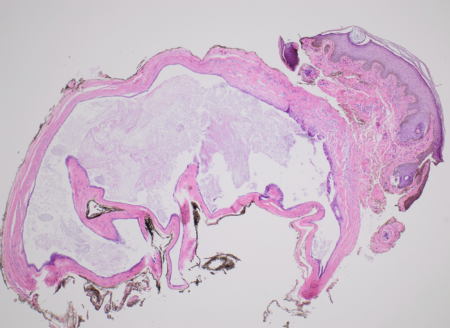
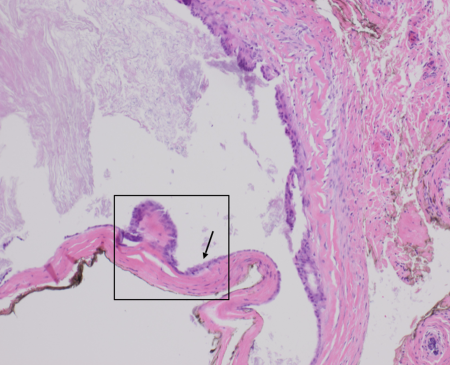
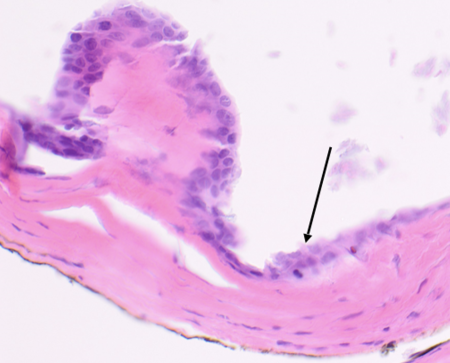
Histological Appearance
Microscopically, apocrine hidrocystomas can appear as a unilocular or multilocular cystic lesion composed of two layers. The first layer is the inner cyst wall that is composed of secretory columnar epithelium. The secretory columnar epithelium can consist of a single layer or a double layer of cuboidal-columnar epithelium. [6] The inner layer of the cysts lies in front of the myoepithelial cells which comprise the outer or peripheral layer. [7] When lipofuscin granules are present, PAS-positive granules can also be seen histologically.[1] Apocrine hidrocystomas also exhibit papillary projections which appear in the lumen of the cyst as an outgrowth from the wall. Papillary projections consist of vascular connective tissue covered by secretory epithelium. [7]
Differential Diagnoses
- Eccrine Hidrocystoma
- Epidermal Inclusion cyst
- Mucoid Cysts
- Hemangioma
- Lymphangioma
- Basal cell carcinoma
- Blue nevi
- Cutaneous melanoma
- Follicular cyst
- Milia
- Syringoma
Treatment
The most common treatment for apocrine hidrocystoma is surgical excision with narrow margins.[1] After excision, the prognosis is excellent due to the benign nature of the lesion. Alternate treatments include needle puncture, cyst puncture followed by hypertonic glucose sclerotherapy and include cyst puncture with trichloroacetic acid injection and botulinum toxin A are currently being explored.[4] Needle puncture has been found to have higher rate of recurrence compared to complete cystic excision including the walls of the cyst.[8] Cyst puncture followed by hypertonic glucose sclerotherapy or followed by trichloroacetic acid injection and botulinum toxin A have been found to be an effective therapeutic modality. (Anandasabapathy)[9]
Prognosis
Apocrine hidrocystomas are benign cystic lesions and therefore have no metastatic potential. Complete surgical excision offers excellent prognosis with minimal chance of recurrence.
Complications
Apocrine hidrocystoma lesion removal is an elective procedure usually completed due to ocular irritation for the patient.
Complications association with surgical excision of the apocrine hidrocystoma includes infection, bleeding, ocular pain and inflammation and possible injury to the orbit with potential for visual deterioration or complete vision loss. [1]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Hafsi W, Badri T, Shah F. Apocrine Hidrocystoma. [Updated 2021 Sep 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448109/
- ↑ Mehregan AH. Apocrine Cystadenoma; A Clinicopathologic Study With Special Reference To The Pigmented Variety. Arch Dermatol. 1964;90:274–9.
- ↑ Magdaleno-Tapial J, Valenzuela-Oñate C, Martínez-Doménech Á, García-Legaz-Martínez M, Martínez-Aparicio A, Alegre-de Miquel V, Pérez-Ferriols A. Apocrine hidrocystoma on the nipple: the first report in this unusual location. Dermatol Online J. 2019 Oct 15;25(10)
- ↑ 4.0 4.1 Nam JH, Lee GY, Kim WS, Kim KJ. Eccrine hidrocystoma in a child: an atypical presentation. Ann Dermatol. 2010 Feb;22(1):69-72.
- ↑ Birkenbeuel J, Goshtasbi K, Mahboubi H, Djalilian HR. Recurrent apocrine hidrocystoma of the external auditory canal. Am J Otolaryngol. 2019 Mar - Apr;40(2):312-313.
- ↑ 6.0 6.1 6.2 6.3 Sarabi K, Khachemoune A. Hidrocystomas--a brief review. MedGenMed. 2006 Sep 06;8(3):57.
- ↑ 7.0 7.1 Chen Y, James C, Leibovitch I, Selva D. Primary orbital apocrine hidrocystoma with sebaceous elements. Clin Exp Ophthalmol. 2018 Jul;46(5):560-562.
- ↑ Osaki TH, Osaki MH, Osaki T, Viana GA. A Minimally Invasive Approach for Apocrine Hidrocystomas of the Eyelid. Dermatol Surg. 2016 Jan;42(1):134-6.
- ↑ Anandasabapathy N, Soldano AC. Multiple apocrine hidrocystomas. Dermatol Online J. 2008 May 15;14(5):12.