Wilson's Disease/Kayser Fleischer Ring
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Wilson’s disease is an inborn error of copper metabolism. A commonly associated symptom is Kayser-Fleischer rings in the cornea of affected individuals.
Detailed Description
Wilson’s disease (also called hepatolenticular degeneration) affects mainly the brain (putamen), liver, cornea and kidney. Although commonly decreased in approximately 85-95% of individuals, a deficiency of ceruloplasmin is not the underlying cause. It results from a mutation in the Wilson Disease Protein, located on chromosome 13. The accumulation of copper in the tissues results in the disease process.
Risk Factors
Wilson’s disease is rare. It occurs in approximately 30 in 1,000,000 people. It comprises less than 5% of chronic active hepatitis cases, but is a common cause of cirrhosis in older children. The mutation is autosomal recessive and no other risk factors have been identified.
Diagnosis
Signs
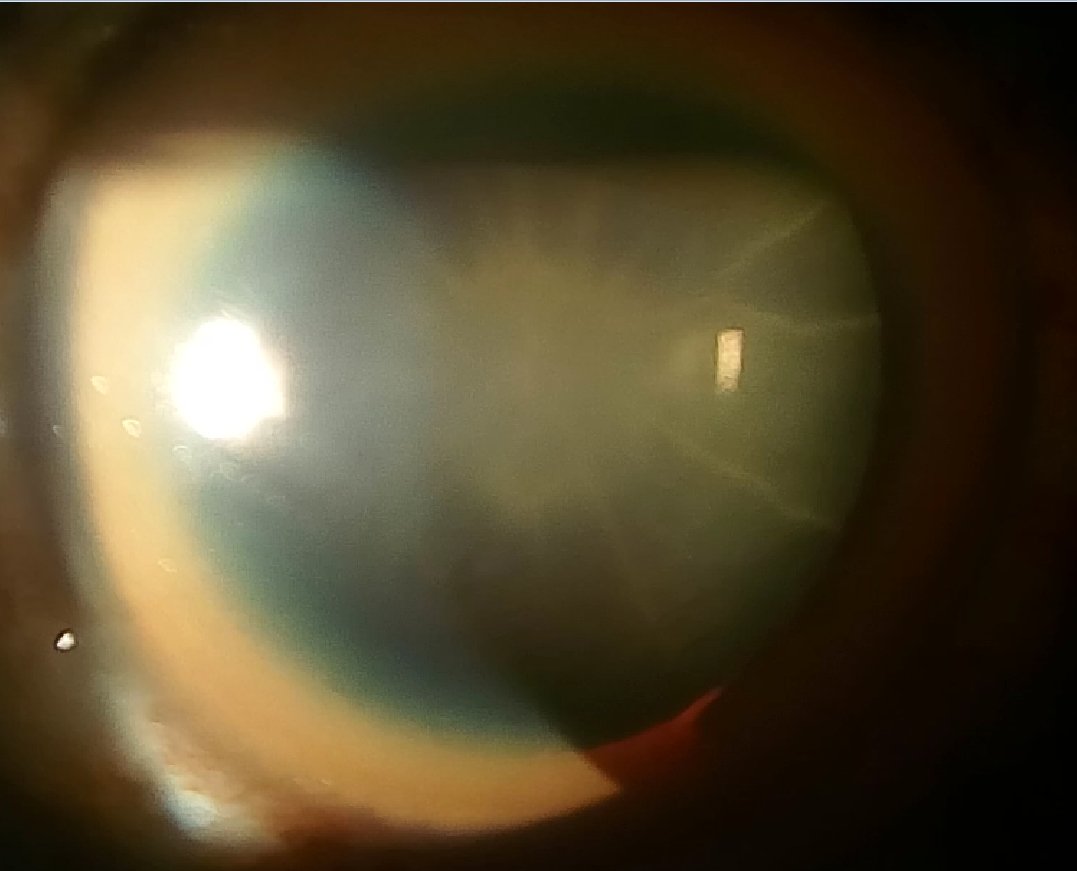
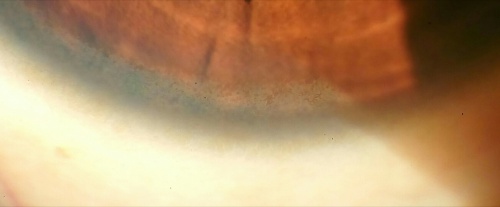
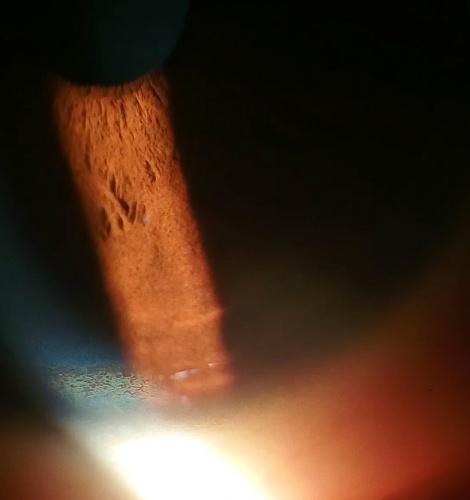
Kayser-Fleischer ring
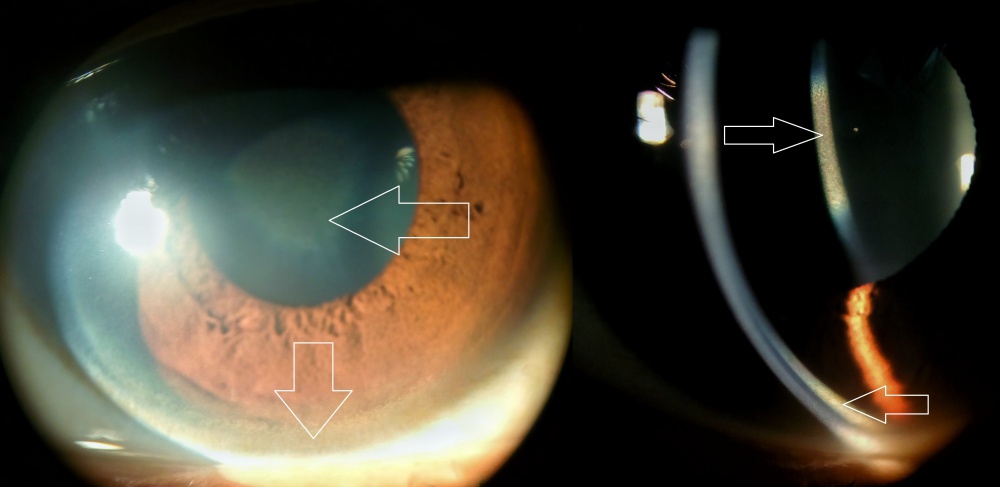
Clinical Diagnosis
On slit lamp examination, one may find Kayser-Fleischer rings which are deposits of copper in Descemet's membrane of the cornea.
Early cases require gonioscopy to detect K-F ring
Laboratory test
- Ceruloplasmin is decreased in 85-90% of individuals
- 24-hour urinary copper and free copper will show increased copper levels
- CBC may show Anemia (copper inhibits glycolytic enzymes causing a Coombs’ negative hemolytic anemia)
- Urinalysis may show aminoaciduria, glycosuria, and increased urinary copper (> 100 mcg/24 hour if symptomatic)
- T2-MRI may show atrophy of caudate and putamen with increased intensity and degenerative changes in the brain with focal cavitation
- Occasionally, studies showing the incorporation of radioactive copper into ceruloplasmin may be necessary
Differential diagnosis
Biliary obstruction (copper is excreted through bile), alcoholic cirrhosis, cryptogenic cirrhosis, ITP, viral or drug-induced hepatitis.
Management
Patients are typically placed on a low-copper diet (no liver, shellfish, nuts, chocolate or mushrooms and started on lifelong chelating agents. Of the chelating agents, D-penicillamine is the drug of choice. Hepatic transplantation for fulminant hepatic failure. Routine monitoring of serum copper and ceruloplasmin is indicated along with liver enzymes, INR, CBC with diff and urinalysis while on chelators. Also a yearly physical with 24-hour urinary copper should be performed while on medication [1].
Prognosis
Patients will have a normal life expectancy if diagnosed early, however, they will develop fulminant hepatic failure if left untreated.
References
- ↑ Roberts EA, Schilsky ML; Division of Gastroenterology and Nutrition, Hospital for Sick Children, Toronto, Ontario, Canada. A practice guideline on Wilson disease. Hepatology. 2003 Jun;37(6):1475-92. Erratum in: Hepatology. 2003 Aug;38(2):536. PubMed PMID: 12774027.
- Ala A, Walker AP, Ashkan K, Dooley JS, Schilsky ML. Wilson's disease. Lancet. 2007 Feb 3;369(9559):397-408. Review. PubMed PMID: 17276780.
- El-Youssef M. Wilson disease. Mayo Clin Proc. 2003 Sep;78(9):1126-36. Review. PubMed PMID: 12962167.
- Roberts EA, Schilsky ML; American Association for Study of Liver Diseases (AASLD). Diagnosis and treatment of Wilson disease: an update. Hepatology. 2008 Jun;47(6):2089-111. PubMed PMID: 18506894.