Trisomy 21/Down Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Down (or Down’s) syndrome (trisomy 21) is the most common chromosomal anomaly in children.[1] This syndrome is typically marked by a characteristic facial appearance, short stature, intellectual disability, and cardiac anomalies. Children with Down syndrome are at increased risk for a variety of ophthalmic disorders, including strabismus, high refractive error, keratoconus, accommodative insufficiency, cataracts, nasolacrimal duct obstruction, blepharitis, and nystagmus. Close observation and management of disorders by a pediatric ophthalmologist is necessary as visual impairment in addition to the social, behavioral, and emotional difficulties experienced by individuals with Down syndrome can be a significant impediment to quality of life.[2]
Disease Entity
Genetics
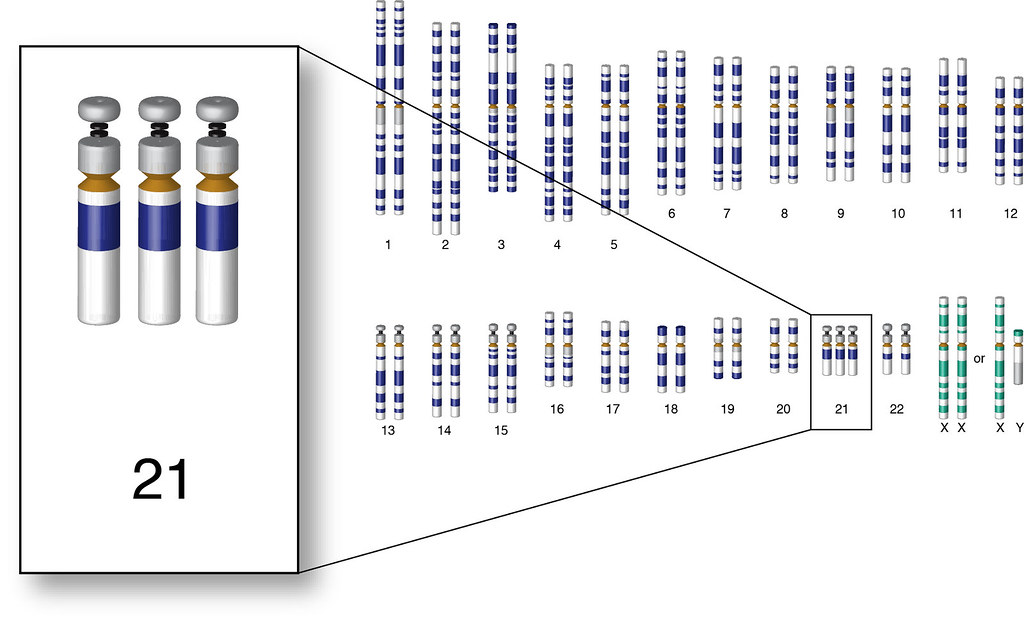
Down syndrome is caused by expression of a third copy of chromosome 21. This extra chromosomal material can be transmitted in three ways. The most common mode of transmission (90-95% of cases) is nondisjunction of either the maternal or paternal chromosome 21 pair during the first phase of meiosis leading to individuals having a complete additional chromosome. Approximately 3-4% of Down syndrome cases are caused by an unbalanced translocation, with chromosome 21 fused via its centromere to another acrocentric chromosome, usually chromosome 14. A de novo mutation leads to 75% of translocation cases, and a balanced translocation in a parent leads to 25% of these cases. In 1-2% of Down syndrome patients, mosaicism is present due to an error in cell division in the early embryonic stage, and these patients may have a less severe phenotype.[3]
Epidemiology
Down syndrome is the most common chromosomal abnormality.[4] Down syndrome occurs in approximately 1 in 700 births, and the frequency rises with maternal age due to an increase in nondisjunction events. Roughly 5,400 children with Down syndrome are born each year in the United States.[5]
The reported prevalence of ophthalmic disorders in Down syndrome patients ranges from 46% to 100%.[6] The incidence of associated eye disease requiring monitoring or intervention increases with age, from 38% of children with Down syndrome < 1 year old to 80% of 5 to 7 year-old children.[7]
Diagnosis
The diagnosis of Down syndrome is generally made by prenatal testing, such as chorionic villus sampling or amniocentesis after a positive first or second trimester screening test. When prenatal testing is not available, the diagnosis of Down syndrome is made by recognition of the phenotypic features of Down syndrome in the neonate, including hypotonia, poor reflexes, flat facial profile, slanted palpebral fissures, and a single palmar crease,[8] followed by a karyotype showing trisomy 21, a translocation, or mosaicism.
Clinical Features
Strabismus
Strabismus, especially esodeviation, is common in children with Down syndrome. The prevalence of strabismus in Down syndrome ranges from 5% to 47%.[2][9] [10] [11] [12] [13] [14] [15] [16] [17] [18] [19] [20] In most of these studies the strabismus type is esotropia, although in one study of Korean children, 42% of children with Down syndrome with strabismus were found to have exotropia.[20] Only one study of children with Down syndrome mentions hyperdeviation, which was found in 7% of patients with strabismus.[16] Strabismus in Down syndrome is typically acquired, rather than congenital.[21]
Nystagmus
Nystagmus has been found to be present in 3% to 33% of children with Down syndrome, which is significantly more prevalent than in control patients.[2][9][10][11][15][17][18][19][20][22] The form is usually a rapid horizontal nystagmus.[14][23] Eighty to 89% of children with Down syndrome with nystagmus have a manifest nystagmus while a smaller cohort have a latent or manifest-latent nystagmus.[13][23][24] [25] Nystagmus in Down syndrome has been associated with lesser visual acuities.[25]
Refractive Error and Astigmatism
Children with Down syndrome have a higher prevalence of hyperopia and astigmatism and a higher magnitude of refractive error compared to age-matched controls.[2][26] Refractive error outside the range of a spherical equivalent of -0.50 to +1.00 D is found in almost 80% of children with Down syndrome.[27] Hyperopia in children with Down syndrome has been found to range from 4% to 65%.[2][6][28] Although the prevalence of myopia ranges from 8% to 41% in children with Down syndrome,[6] it has not been found to be significantly higher than in controls.[2][28] In addition, before one year of age, there is no significant difference in the prevalence of refractive error when comparing to age-matched controls.[29] Failure of emmetropization has been proposed as the etiology of the increase in prevalence of refractive error after infancy.[30]
In infants up to 12 months old without Down syndrome, clinically significant astigmatism is common, with a prevalence ranging from 40 to 53%. The prevalence of astigmatism then declines to 10% to 18% by 4 years of age.[31] [32] In infants and in children up to age 4 with Down syndrome, the prevalence of astigmatism is not significantly different than with controls. However, while the rates of astigmatism decline after infancy in control patients, children with Down syndrome continue to have roughly the same prevalence of astigmatism. At the primary school age (4 to 12 years), children with Down syndrome have a 37.5% prevalence of astigmatism, significantly higher than in age-matched controls.[29]
Infants with Down syndrome generally have “with the rule” astigmatism. The type of astigmatism often changes, with 26% to 54.8% of patients with astigmatism having an oblique type of astigmatism.[30][33] [34] [35] Looking at a cross sectional population of children with Down syndrome by age, the prevalence of oblique astigmatism is low in infancy, at 7.1% of children with astigmatism at one year of age, and raises to 45% of 15-year-old children with astigmatism.[36] The development of oblique astigmatism has been proposed to be caused by the oblique, upslanting palpebral fissues in Down patients,[37] as the axis of astigmatism has been correlated with the angle of the palpebral fissure.[38]
Visual Acuity
Best corrected visual acuity (BCVA) in Down syndrome patients is on average less than comparative controls, even in patients with no apparent ocular abnormalities [39]. In studies of visual acuity in children with Down syndrome, BCVA was found to be 20/45 on average,[28] worse than 20/50 in 24% of patients,[40] and below average for age for 94% of subjects, with 79% of subjects falling two standard deviations below the mean.[41] There are multiple causes for this decrease in BCVA. One major cause is amblyopia, which affects 3% to 26% of children with Down syndrome.[16][19][23][40] As strabismus is common in Down syndrome, early and regular assessment and treatment can help minimize visual loss due to amblyopia. Nystagmus may also account for a substantial extent of visual acuity loss.[25] Other common causes of decreased visual acuity in Down syndrome patients include cataracts and high refractive errors.[42] It has also been hypothesized that abnormalities in the development of the visual cortex may further limit visual potential, even in children with relatively mild ocular pathology. [43]
Accommodation
Poor accommodative ability is a classic ophthalmologic finding in children with Down syndrome, and this may be an additional barrier to literacy and early learning in these children. Using dynamic retinoscopy, studies have found that 32% to 100% of children with Down syndrome have an abnormally low ability to accommodate, measured by accommodative response.[34][44] [45][46] Inaccurate accommodation has been found to be associated with hypermetropia and strabismus.[34][47] The etiology of this hypoaccommodation is still unclear. While mechanical deficits of the accommodative mechanism (as in presbyopia) may be a factor, recent research suggests a more likely etiology is impaired sensory pathway signaling for an accommodative response to a near stimulus.[28]
Eyelids and Midface
The most common findings are upward slanting palpebral fissures, with a prevalence ranging from 63% to 82% in children with Down syndrome,[16][20] and large epicanthal folds, ranging from 31% to 97%.[13][15][16][17][20] Blepharitis is also a common finding in Down syndrome patients. The prevalence of blepharitis in children with Down syndrome ranges from 3% to 34.5%.[10][11][13][14][15][16][17][18][19][20][22] The wide range in prevalence may be due to differing criteria for diagnosing blepharitis.[48] The high rate of blepharitis has been speculated to be due to impaired immune or due to skin abnormalities in Down syndrome individuals.[16][49] Other disorders of the eyelids include epiblepharon, which has been found to be more common in a Korean population of Down syndrome patients with a prevalence of 54% (ranging from 43% at birth to the highest of 65% at ages 4 to 6).[20] In comparison to a Japanese population of control patients, epiblepharon incidence at birth was 46% and decreased to 9.9% by age 18.[50] However, in a Malaysian population of children with Down syndrome with a mean age of 7 years old, the incidence of epiblepharon was 2%.[17]
Lacrimal
Lacrimal duct obstruction is common, found to range from 3.3% to 36% in children with Down syndrome.[10] [13] [14] [15] [17] [18] [19] [20] In one study, bilateral involvement was found in 73% of patients.[51] The higher rate of nasolacrimal duct obstruction is related to the facial morphology of Down syndrome.[52] Compared to the general pediatric population where congenital nasolacrimal duct obstruction is typically due to failure of Hasner’s membrane to open, congenital nasolacrimal duct obstruction in Down syndrome tends to be more complex, with pathology such as bony obstruction, canalicular atresia or stenosis, anteriorly displaced inferior turbinate, or exceptionally tight ducts.[51]
Cornea
Down syndrome is one of the strongest risk factors for keratoconus, as studies using modern corneal topography have demonstrated an incidence as high as 20.8-32% in people with Down syndrome.[53][54] One study in Norway found that the risk of keratoconus was 30 times higher in patients with Down syndrome compared to the population at large.[55] Keratoconus in Down syndrome commonly develops in childhood or teenage years, with one case report describing a child diagnosed as early as 4 years old.[56][57]
The cornea in patients with Down syndrome is steeper with higher rates of astigmatism than controls.[26] Eye-rubbing has been thought to play a role in developing keratoconus,[58] [59] which patients with Down syndrome may be more prone to due to the higher rate of chronic blepharitis.[48] [60]Some studies have suggested a genetic link between genes on chromosome 21 and keratoconus, which could explain the increased prevalence in trisomy 21.[61] [62]
Iris

Brushfield spots are white, gray, or brown spots spaced around the periphery of the iris. They are focal areas of iris stromal connective tissue hyperplasia which are of no functional importance.[27] They are not pathognomonic for Down syndrome and can be seen in children without disease. Brushfield spots are more common on blue, green or hazel irides compared to dark irides.[16] The prevalence of Brushfield spots differ in various ethnic populations, possibly reflecting variations in predominant iris color between ethnic groups.[10] In studies of children with Down syndrome in Italian, Egyptian, and South and East Asian populations, Brushfield spots were not found in any patient. [11] [13] [15] [18] [20] In Slovenian, Brazilian and American studies, the prevalence was found to be 16.9%, 52%, and 81% respectively.[16][48][63]
Lens

Lenticular abnormalities are common in Down syndrome, with the published prevalence of cataracts in Down syndrome varying from 4% to 72% depending on age and diagnostic criteria, and with the two most characteristic cataract types seen in Down syndrome being congenital cataracts and cerulean cataracts.[2] [14] [15] [16] [17] [19] [22][64] The incidence of congenital cataracts in Down syndrome has been found to be as high as 2.2% in one large retrospective observational study in Brazil.[65] Another population-based study found that the relative risk of congenital cataracts was about 300 times higher in infants with Down syndrome compared to those without.[66] A retrospective study at Children’s University Hospital in Dublin found that over a 25-year period, approximately 7% of children undergoing cataract surgery at their institution had Down syndrome.[67]
More commonly patients with Down syndrome are found to have cerulean cataracts, which are characterized by scattered blue-dot opacities throughout the cortex and occasionally nucleus. These opacities may be found in the lens of up to 50% of patients with Down syndrome, but they are not generally considered visually significant.[68][64]
Some studies have also found that age-related nuclear sclerotic cataracts may develop at an earlier age in the Down syndrome population, with one paper reporting an average age of 48.4 years at time of diagnosis of age-related NSC.[69][64]
Retina
OCT studies have demonstrated a high incidence of foveal hypoplasia in children with Down syndrome, with abnormalities of the inner retinal layers especially prevalent.[70][71]
Retinoblastoma has also been speculated to be connected to Down syndrome, possibly caused by oncogenic genes overexpressed on chromosome 21, although there have only been a few recorded cases of this disease in Down syndrome patients.[17][72][73]
It has been reported that diabetics with Down syndrome may have a lower incidence of diabetic retinopathy, though the only relevant study included only 9 patients.[74] There are no published studies on the incidence of macular degeneration in the Down syndrome population.
Optic Nerve
Optic nerve anomalies are relatively common in children with Down syndrome, with increased incidence of optic nerve hypoplasia, optic disc torsion, optic disc elevation, peripapillary atrophy, peripapillary pigment anomalies, and optic nerve crescents.[75]
Another common disc abnormality in Down syndrome is a spoke-like appearance with a high number of vessels crossing the margin of the optic nerve. Although not associated with vision loss, studies have found that 13% to 38% of children with Down syndrome have 18 or more vessels crossing the disc margin.[10][20][24][76] This has been proposed to be a consequence of a deficiency in systemic angiogenesis.[77]
Glaucoma
Glaucoma in children with Down syndrome is rare.[49] In most recent studies, the prevalence ranges from 0% to 1% of cases, [11] [14] [15] [19] [20] [63] although in one series in Malaysian children with Down syndrome, the prevalence was 7%.[17] In contrast, in a general pediatric population, the incidence of primary childhood glaucoma over a 40-year period was 0.38 per 100,000 children.[78]
There is only one published study on the incidence of glaucoma in adults with Down syndrome. Despite having identified only three patients with both Down syndrome and glaucoma, the authors concluded that adults with Down syndrome have a higher incidence of glaucoma. [79]
Visual cortex
Down syndrome is associated with impaired cortical development during pregnancy and early childhood, as well as accelerated brain atrophy as individuals age.[80][81] It is hypothesized that abnormalities of the visual cortex may contribute to the decreased visual acuity often encountered in patients with Down syndrome, including those with relatively normal ocular anatomy.[39]
Management
General
Pediatric ophthalmologists should be considered part of all Down syndrome children’s healthcare team whose contributions greatly assist in allowing the patient to reach his or her full health and developmental potential. The American Academy of Pediatrics provides the following recommendations for visits to a pediatric ophthalmologist or ophthalmologist with special expertise and experience with children with disabilities by all children with Down syndrome:
- Within the first 6 months of life: Refer for evaluation for strabismus, cataracts, nasolacrimal duct obstruction, refractive errors, glaucoma, and nystagmus
- 1-5 years of age: Check the child’s vision, and use developmentally appropriate subjective and objective criteria, including photoscreening if available, at each well-child visit. Refer if abnormal findings on photoscreening or annually if no photoscreening available
- 5-12 years of age: Perform photoscreening at every health supervision visit. Refer if abnormal findings on photoscreening or every 2 years if no photoscreening available
- 12-21 years old: Perform visual acuity testing or photoscreening or ensure that they are under care of appropriate ophthalmologist to assess for onset of cataracts, refractive error, or keratoconus.[3]
Photoscreening appears to be a suitable method to screen children with Down Syndrome and normal baseline examination in terms of detecting the development of treatable ocular conditions.[82] Although the development of new ocular pathology in a child with trisomy 21 and a previously normal examination is not unusual, most of these new abnormalities are detectable with automated vision screening techniques or direct visual inspection of the eyes and ocular adnexa; thus once a child has a normal examination, formal vision screening can replace a formal ophthalmologic examination. [83]
Strabismus
The treatment of strabismus for children with Down syndrome is similar to the general pediatric population. Bilateral medial rectus muscle recession for esotropia in patients with Down syndrome with the standard surgical dosage results in similar outcomes as controls and does not typically result in overcorrection as has been thought to occur in developmentally delayed children.[84] [85]
Nystagmus
A fine, rapid horizontal nystagmus in patients in Down syndrome occurs frequently, is generally stable or self-resolving, and needs no specific investigation or intervention.[14]
Refractive Error and Astigmatism
Refractive error is treated with prescription glasses. Compliance with glasses wear is generally high, although difficulties can arise depending on the individual. The addition of bifocals due to reduced accommodative ability may be important for optimal near vision to promote learning potential.
Visual Acuity
Although visual acuity testing can be difficult in children, especially with intellectual disability, visual acuity has been measured in preverbal children with Down syndrome using Teller, Keeler, and Cardiff acuity cards with success rates ranging up to 100%. [12] [13] [25] [40] [41]
Accommodation
Use of bifocal prescriptions can significantly improve the accommodative ability of people with Down syndrome, with the improvement often continuing after returning to single vision lenses.[86] In addition, bifocals have also been found to help with accommodation when looking through the distance portion of their glasses, meaning that instead of solely being a focusing aid as with presbyopic adults, bifocals may help children better use their own accommodative ability.[87] Nandakumar et al. suggests that children should first be checked for their refractive error, as they found that 79% of children with Down syndrome did not have a correct prescription, possibly due to difficulties with examining this population or due to lack of adequate care for patients with developmental delays.[46] Compliance with eyeglasses wear was comparable to children without disabilities, at 82% being fully compliant and 18% being partially compliant.[87]
Eyelids and Midface
Blepharitis can be treated similarly as with children without Down syndrome. See EyeWiki article on Blepharitis.
Lacrimal
In the general pediatric population, probing procedures have a high rate of success, as the common reason for obstruction is failure for Hasner’s membrane to open. However, in Down syndrome, canalicular stenosis and atresia are more common reasons for obstruction. A more aggressive initial treatment may be appropriate, such as stents or balloon dilation, depending on the etiology of the obstruction.[51][88]
Cornea
Keratoconus can be difficult to diagnose and treat in the Down syndrome population. Relying on cycloplegic refraction alone as a screening tool for the Down syndrome population is insufficient, as even children with low amounts of astigmatism may have keratoconus. Children with Down syndrome should be routinely screened with corneal topography as soon as they are old enough or cooperative enough to sit for the exam.[89]. Treatment can be complicated by difficulties in fitting contact lenses, excessive eye rubbing, and in patient reporting of changes in visual acuity.[90] Corneal collagen cross-linking has been found to be safe and effective in the Down syndrome population, even in children as young as 4 years old.[91][56] See EyeWiki article on Keratoconus.
Iris
Brushfield spots are a benign finding and require no treatment.
Lens
Neonates with known Down syndrome should be carefully checked for a robust red reflex by a pediatrician shortly after birth to screen for congenital cataracts. If a cataract is found, surgical intervention may be required. See EyeWiki article on Congenital Cataracts.
Retina
The blood vessel spoke-like appearance is a benign finding with no management needed. Other retinal pathology should be treated as with the general pediatric population.
Optic Nerve
Optic nerve edema, papilledema or idiopathic intracranial hypertension should be suspected in children with elevated optic disks, but they may represent transient, benign findings in children with Down syndrome.[92]
Glaucoma
The child should be monitored for signs of primary congenital glaucoma, and if present, medical and surgical interventions are required.
Summary
Down syndrome is a common genetic disease with a high rate of ophthalmic findings. Some manifestations are benign, such as epicanthal folds and Brushfield spots, but Down syndrome is associated with lower visual acuity due to refractive error, astigmatism, amblyopia, nystagmus, and cataracts, among other disorders. These disorders require early evaluation and follow-up by a pediatric ophthalmologist with expertise in developmentally challenged populations to provide the best visual outcome for the child and throughout adulthood.
Additional Resources
Support groups
- National Down Syndrome Society: http://www.ndss.org/Resources/Local-Support
- Global Down Syndrome Foundation: http://www.globaldownsyndrome.org/about-down-syndrome/resources/local-organizations/
References
- ↑ Antonarakis SE. Parental origin of the extra chromosome in trisomy 21 as indicated by analysis of DNA polymorphisms. Down Syndrome Collaborative Group. N Engl J Med. 1991 Mar 28;324(13):872-6. doi: 10.1056/NEJM199103283241302. PMID: 1825697.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Akinci A, Oner O, Bozkurt OH, et al. Refractive errors and strabismus in children with Down syndrome: a controlled study. J Pediatr Ophthalmol Strabismus 2008;46:83–86.
- ↑ Jump up to: 3.0 3.1 Bull MJ, Trotter T, Santoro SL. Health Supervision for Children and Adolescents With Down Syndrome. Pediatrics 2022;149: e2022057010.
- ↑ Malt EA, Dahl RC, Haugsand TM, et al. Health and disease in adults with Down syndrome. Tidsskr den Nor Laegeforening. 2013;133:290–294.
- ↑ Sherman SL, Allen EG, Bean LH, Freeman SB. Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev. 2007;13:221–227.
- ↑ Jump up to: 6.0 6.1 6.2 Creavin AL, Brown RD. Ophthalmic abnormalities in children with Down syndrome. J Pediatr Ophthalmol Strabismus 2008;46:76–82.
- ↑ Roizen NJ, Patterson D. Down’s syndrome. Lancet. 2003;361:1281–1289.
- ↑ Jones KL, Jones MC, Campo M. Smith’s Recognizable Patterns of Human Malformation. 7th ed. Philadelphia: Elsevier; 2013.
- ↑ Jump up to: 9.0 9.1 Kim U, Hwang J-M. Refractive errors and strabismus in Asian patients with Down syndrome. Eye (Lond) 2009;23:1560–1564.
- ↑ Jump up to: 10.0 10.1 10.2 10.3 10.4 10.5 Berk AT, Saatci AO, Erçal MD, et al. Ocular findings in 55 patients with Down’s syndrome. Ophthalmic Genet. 1996;17:15–19.
- ↑ Jump up to: 11.0 11.1 11.2 11.3 11.4 Wong V, Ho D. Ocular abnormalities in Down syndrome: An analysis of 140 Chinese children. Pediatr Neurol. 1997;16:311–314.
- ↑ Jump up to: 12.0 12.1 Mohd-Ali B, Mohammed Z, Norlaila MD, et al. Visual and binocular status of down syndrome children in Malaysia. Clin Exp Optom. 2006;89:150–154.
- ↑ Jump up to: 13.0 13.1 13.2 13.3 13.4 13.5 13.6 Paudel N, Leat SJ, Adhikari P, et al. Visual defects in Nepalese children with Down syndrome. Clin Exp Optom. 2010;93:83–90.
- ↑ Jump up to: 14.0 14.1 14.2 14.3 14.4 14.5 14.6 Stephen E, Dickson J, Kindley D, et al. Surveillance of vision and ocular disorders in children with Down syndrome. Dev Med Child Neurol. 2007;49:513–515.
- ↑ Jump up to: 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 Fimiani F, Iovine A, Carelli R, et al. Incidence of ocular pathologies in Italian children with Down syndrome. Eur J Ophthalmol. 2007;17:817–822.
- ↑ Jump up to: 16.0 16.1 16.2 16.3 16.4 16.5 16.6 16.7 16.8 16.9 Da Cunha RP, Moreira JB. Ocular findings in Down’s syndrome. Am J Ophthalmol. 1996;122:236–244.
- ↑ Jump up to: 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 17.8 Liza-Sharmini AT, Azlan ZN, Zilfalil BA. Ocular findings in Malaysian children with Down syndrome. Singapore Med J. 2006;47:14–19.
- ↑ Jump up to: 18.0 18.1 18.2 18.3 18.4 Afifi HH, Abdel Azeem AA, El-Bassyouni HT, et al. Distinct ocular expression in infants and children with Down syndrome in Cairo, Egypt: myopia and heart disease. JAMA Ophthalmol. 2013;131:1057–66.
- ↑ Jump up to: 19.0 19.1 19.2 19.3 19.4 19.5 19.6 Roizen NJ, Mets MB, Blondis TA. Ophthalmic disorders in children with Down syndrome. Dev Med Child Neurol. 1994;36:594–600.
- ↑ Jump up to: 20.00 20.01 20.02 20.03 20.04 20.05 20.06 20.07 20.08 20.09 20.10 Kim JH, Hwang JM, Kim HJ, Yu YS. Characteristic ocular findings in Asian children with Down syndrome. Eye (Lond). 2002;16:710–714.
- ↑ Haugen OH, Høvding G. Strabismus and binocular function in children with Down syndrome. A population-based, longitudinal study. Acta Ophthalmol Scand. 2001 Apr;79(2):133-9. doi: 10.1034/j.1600-0420.2001.079002133.x. PMID: 11284750.
- ↑ Jump up to: 22.0 22.1 22.2 Merrick J, Koslowe K. Refractive errors and visual anomalies in Down syndrome. Downs Syndr Res Pract. 2001;6:131–133.
- ↑ Jump up to: 23.0 23.1 23.2 Ljubic A, Trajkovski V, Stankovic B. Strabismus, refractive errors and nystagmus in children and young adults with Down syndrome. Ophthalmic Genet. 2011;32:204–211.
- ↑ Jump up to: 24.0 24.1 Wagner RS, Caputo AR, Reynolds RD. Nystagmus in Down’s syndrome. Ophthalmology. 1990;97:1439–1444.
- ↑ Jump up to: 25.0 25.1 25.2 25.3 Felius J, Beauchamp CL, Stager DR. Visual acuity deficits in children with nystagmus and down syndrome. Am J Ophthalmol. 2014;157:458–463.
- ↑ Jump up to: 26.0 26.1 Little J-A, Woodhouse JM, Saunders KJ. Corneal power and astigmatism in Down syndrome. Optom Vis Sci. 2009;86:748–754.
- ↑ Jump up to: 27.0 27.1 Watt T, Robertson K, Jacobs RJ. Refractive error, binocular vision and accommodation of children with Down syndrome. Clin Exp Optom. 2015;98:3–11.
- ↑ Jump up to: 28.0 28.1 28.2 28.3 Anderson HA, Manny RE, Glasser A, Stuebing KK. Static and dynamic measurements of accommodation in individuals with down syndrome. Investig Ophthalmol Vis Sci. 2011;52:310–317.
- ↑ Jump up to: 29.0 29.1 Woodhouse JM, Pakeman VH, Cregg M, et al. Refractive errors in young children with Down syndrome. Optom Vis Sci. 1997;74:844–851.
- ↑ Jump up to: 30.0 30.1 Doyle SJ, Bullock J, Gray C, et al. Emmetropisation, axial length, and corneal topography in teenagers with Down’s syndrome. Br J Ophthalmol. 1998;82:793–796.
- ↑ Mohindra I, Held R, Gwiazda J, Brill J. Astigmatism in infants. Science. 1978;202:329–331.
- ↑ Gwiazda J, Scheiman M, Mohindra I, Held R. Astigmatism in children: Changes in axis and amount from birth to six years. Investig Ophthalmol Vis Sci. 1984;25:88–92.
- ↑ Antonela L, Vladimir T. Refractive errors in children and young adults with Down’s syndrome. Acta Ophthalmol. 2011;89:324–327.
- ↑ Jump up to: 34.0 34.1 34.2 Haugen OH, Høvding G, Lundström I. Refractive development in children with Down’s syndrome: a population based, longitudinal study. Br J Ophthalmol. 2001;85:714–719.
- ↑ Cregg M, Woodhouse JM, Stewart RE, et al. Development of refractive error and strabismus in children with Down syndrome. Investig Ophthalmol Vis Sci. 2003;44:1023–1030.
- ↑ Al-Bagdady M, Murphy PJ, Woodhouse JM. Development and distribution of refractive error in children with Down’s syndrome. Br J Ophthalmol. 2011;95:1091–1097.
- ↑ Haugen OH, Høvding G, Eide GE. Biometric measurements of the eyes in teenagers and young adults with Down syndrome. Acta Ophthalmol Scand. 2001;79:616–625.
- ↑ Read SA, Collins MJ, Carney LG. The influence of eyelid morphology on normal corneal shape. Investig Ophthalmol Vis Sci. 2007;48:112–119.
- ↑ Jump up to: 39.0 39.1 39.2 39.3 Postolache L, Monier A, Lhoir S. Neuro-Ophthalmological Manifestations in Children with Down Syndrome: Current Perspectives. Eye Brain. 2021;13:193-203. Published 2021 Jul 21. doi:10.2147/EB.S319817
- ↑ Jump up to: 40.0 40.1 40.2 Tsiaras WG, Pueschel S, Keller C, et al. Amblyopia and visual acuity in children with Down’s syndrome. Br J Ophthalmol. 1999;83:1112–1114.
- ↑ Jump up to: 41.0 41.1 Courage ML, Adams RJ, Reyno S, Kwa PG. Visual acuity in infants and children with Down syndrome. Dev Med Child Neurol. 1994;36:586–593.
- ↑ Morton G V. Why do children with down syndrome have subnormal vision? Am Orthopt J. 2011;61:60–70.
- ↑ Woodhouse JM, Pakeman VH, Saunders KJ, et al. Visual acuity and accommodation in infants and young children with Down's syndrome. Journal of Intellectual Disability Research. 1996;40:49-55. https://doi.org/10.1111/j.1365-2788.1996.tb00602.x
- ↑ Woodhouse JM, Meades JS, Leat SJ, Saunders KJ. Reduced accommodation in children with Down syndrome. Investig Ophthalmol Vis Sci. 1993;34:2382–2387.
- ↑ Woodhouse JM, Cregg M, Gunter HL, et al. The effect of age, size of target, and cognitive factors on accommodative responses of children with Down syndrome. Invest Ophthalmol Vis Sci. 2000;41:2479–2485.
- ↑ Jump up to: 46.0 46.1 Nandakumar K, Leat SJ. Bifocals in Down Syndrome Study (BiDS): design and baseline visual function. Optom Vis Sci. 2009;86:196–207.
- ↑ Stewart RE, Woodhouse JM, Cregg M, Pakeman VH. Association between accommodative accuracy, hypermetropia, and strabismus in children with Down’s syndrome. Optom Vis Sci. 2007;84:149–155.
- ↑ Jump up to: 48.0 48.1 48.2 Shapiro MB, France TD. The ocular features of Down’s syndrome. Am J Ophthalmol. 1985;99:659–663.
- ↑ Jump up to: 49.0 49.1 Catalano RA. Down syndrome. Surv Ophthalmol. 1993;34:385–398.
- ↑ Noda S, Hayasaka S, Setogawa T. Epiblepharon with inverted eyelashes in Japanese children. I. Incidence and symptoms. Br J Ophthalmol. 1989;73:126–7.
- ↑ Jump up to: 51.0 51.1 51.2 Coats DK, Brady McCreery KM, Plager D a., et al. Nasolacrimal outflow drainage anomalies in Down’s syndrome. Ophthalmology. 2003;110:1437–1441.
- ↑ Baran F, Kelly JP, Finn LS, et al. Evaluation and treatment of failed nasolacrimal duct probing in Down syndrome. J AAPOS. 2014;18:226–231.
- ↑ Marsack JD, Benoit JS, Kollbaum PS, Anderson HA. Application of Topographical Keratoconus Detection Metrics to Eyes of Individuals with Down Syndrome. Optom Vis Sci. 2019;96(9):664-669. doi:10.1097/OPX.0000000000001417
- ↑ Imbornoni LM, Wise RE, Taravella MJ, Hickey F, McCourt EA. Keratoconus and corneal morphology in patients with Down syndrome at a pediatric hospital. J AAPOS. 2020 Jun;24(3):140.e1-140.e5. doi: 10.1016/j.jaapos.2020.02.004. Epub 2020 May 27. PMID: 32473288.
- ↑ Kristianslund O, Drolsum L. Prevalence of Keratoconus in Persons With Down Syndrome in a National Registry in Norway. JAMA Netw Open. 2021;4(3):e210814. doi:10.1001/jamanetworkopen.2021.0814
- ↑ Jump up to: 56.0 56.1 Sabti S, Tappeiner C; Frueh BE. Corneal Cross-Linking in a 4-Year-Old Child With Keratoconus and Down Syndrome. Cornea. 2015;34(9):1157-1160 doi: 10.1097/ICO.0000000000000491
- ↑ Hashemi, H., Miraftab, M., Amanzadeh, K. et al. Keratoconus detection by novel indices in patients with Down syndrome: a cohort population-based study. Jpn J Ophthalmol. 2020;64:285–291. https://doi.org/10.1007/s10384-020-00725-4
- ↑ McMonnies CW. Mechanisms of rubbing-related corneal trauma in keratoconus. Cornea. 2009;28:607–615.
- ↑ Lindsay RG, Bruce AS, Gutteridge IF. Keratoconus associated with continual eye rubbing due to punctal agenesis. Cornea. 2000;19:567–569.
- ↑ Miyazaki EA. The orthoptics of Down syndrome. Am Orthopt J. 2014;64:12–6.
- ↑ Burdon KP, Vincent AL. Insights into keratoconus from a genetic perspective. Clin Exp Optom. 2013;96:146–154.
- ↑ Nielsen K, Hjortdal J, Pihlmann M, Corydon TJ. Update on the keratoconus genetics. Acta Ophthalmol. 2013;91:106–113.
- ↑ Jump up to: 63.0 63.1 Stirn Kranjc B. Ocular Abnormalities and Systemic Disease in Down Syndrome. Strabismus. 2012;20:74–77.
- ↑ Jump up to: 64.0 64.1 64.2 Fong AH, Shum J, Ng AL, Li KK, McGhee S, Wong D. Prevalence of ocular abnormalities in adults with Down syndrome in Hong Kong. Br J Ophthalmol. 2013 Apr;97(4):423-8. doi: 10.1136/bjophthalmol-2012-302327. Epub 2013 Feb 1. PMID: 23376568.
- ↑ Bermudez BEBV, de Souza do Amaral ME, da Silva Gomes C, Novadzki IM, de Oliveira CM, Serpe CC. Ophthalmological abnormalities in Down syndrome among Brazilian patients. Am J Med Genet Part A. 2020; 182A: 2641– 2645. https://doi.org/10.1002/ajmg.a.61845
- ↑ Källén B, Mastroiacovo P, Robert E. Major congenital malformations in down syndrome. Am J Med Genet. 1996;65:160–166.
- ↑ Gardiner C, Lanigan B, O’Keefe M. Postcataract surgery outcome in a series of infants and children with Down syndrome. Br J Ophthalmol. 2008;92:1112-1116.
- ↑ Little JA, Mahil ADS, Richardson P, et al. In-vivo anterior segment OCT imaging provides unique insight into cerulean blue-dot opacities and cataracts in Down syndrome. Sci Rep 10, 10031 (2020). https://doi.org/10.1038/s41598-020-66642-1
- ↑ Krinksy-McHale SJ, Jenkins EC, Zigman WB, Silverman W. Ophthalmic Disorders in Adults with Down Syndrome. Current Gerontology and Geriatrics Research. 2012; Article ID 974253. https://doi.org/10.1155/2012/974253
- ↑ Nicholson R, Osborne D, Fairhead L, Beed L, Hill CM, Lee H. Segmentation of the foveal and parafoveal retinal architecture using handheld spectral-domain optical coherence tomography in children with Down syndrome. Eye (Lond). 2022 Jan 10. doi: 10.1038/s41433-021-01883-6. Epub ahead of print. PMID: 35001092.
- ↑ Mangalesh S, Vinekar A, Jayadev C, Kemmanu V, Bhat M, Sivakumar M, Bauer N, Webers C, Shetty B. Spectral Domain Optical Coherence Tomography in Detecting Sub-Clinical Retinal Findings in Asian Indian Children with Down Syndrome. Current Eye Research. 2019;44(8):901-907, DOI: 10.1080/02713683.2019.1597128
- ↑ Brichard B, Vermylen C, De Potter P, Casteels I. Down syndrome: Possible predisposition to retinoblastoma. Med Pediatr Oncol. 2003;41:73–74.
- ↑ Satgè D, Schorderet DF, Balmer A, Beck-Popovic M, Addor MC, Beckmann JS, Munier FL. Association Down Syndrome-Retinoblastoma: A New Observation. Ophthalmic Genetics. 2005. 26(3):151-152, DOI: 10.1080/13816810500228894
- ↑ Fulcher T, Griffin M, Crowley S, Firth R, Acheson R, O'Meara N. Diabetic retinopathy in Down's syndrome. Br J Ophthalmol. 1998 Apr;82(4):407-9. doi: 10.1136/bjo.82.4.407. PMID: 9640190; PMCID: PMC1722576.
- ↑ Postolache L. Abnormalities of the Optic Nerve in Down Syndrome and Associations With Visual Acuity. Front Neurol. 2019;10:633. doi:10.3389/fneur.2019.00633
- ↑ Williams EJ, McCormick AQ, Tischler B. Retinal vessels in Down’s syndrome. Arch Ophthalmol. 1973;89:269–271.
- ↑ Parsa CF, Almer Z. Supranumerary optic disc vessels may indicate reduced systemic angiogenesis in Down syndrome. Br J Ophthalmol. 2008;92:432–433.
- ↑ Aponte EP, Diehl N, Mohney BG. Incidence and clinical characteristics of childhood glaucoma: a population-based study. Arch Ophthalmol. 2010;128:478–482.
- ↑ Yokoyama T, Tamura H, Tsukamoto H, Yamane K, Mishima HK. Prevalence of glaucoma in adults with Down's syndrome. Jpn J Ophthalmol. 2006 May-Jun;50(3):274-6. doi: 10.1007/s10384-005-0305-x. PMID: 16767384.
- ↑ Wisniewski KE. Down syndrome children often have brain with maturation delay, retardation of growth, and cortical dysgenesis. Am J Med Genet Suppl. 1990;7:274-81. doi: 10.1002/ajmg.1320370755. PMID: 2149962.
- ↑ Teipel SJ, Hampel H. Neuroanatomy of Down syndrome in vivo: a model of preclinical Alzheimer's disease. Behav Genet. 2006 May;36(3):405-15. doi: 10.1007/s10519-006-9047-x. PMID: 16485178.
- ↑ Yanovitch T, Wallace DK, Freedman SF, Enyedi LB, Kishnani P, Worley G, Crissman B, Burner E, Young TL. The accuracy of photoscreening at detecting treatable ocular conditions in children with Down syndrome. J AAPOS. 2010 Dec;14(6):472-7. doi: 10.1016/j.jaapos.2010.09.016. PMID: 21168069; PMCID: PMC3042280.
- ↑ Umfress AC, Hair CD, Donahue SP. Prevalence of Ocular Pathology on Initial Screening and Incidence of New Findings on Follow-up Examinations in Children With Trisomy 21. Am J Ophthalmol 2019;207:373–377.
- ↑ Yahalom C, Mechoulam H, Cohen E, Anteby I. Strabismus surgery outcome among children and young adults with Down syndrome. J AAPOS. 2010;14:117–119.
- ↑ Motley WW, Melson AT, Gray ME, Salisbury SR. Outcomes of Strabismus Surgery for Esotropia in Children With Down Syndrome Compared With Matched Controls. J Pediatr Ophthalmol Strabismus. 2012;49:211–214.
- ↑ Al-Bagdady M, Stewart RE, Watts P, et al. Bifocals and Down’s syndrome: Correction or treatment? Ophthalmic Physiol Opt. 2009;29:416–421.
- ↑ Jump up to: 87.0 87.1 Stewart RE, Woodhouse JM, Trojanowska LD. In focus: The use of bifocal spectacles with children with Down’s syndrome. Ophthalmic Physiol Opt. 2005;25:514–522.
- ↑ Lueder GT. Treatment of nasolacrimal duct obstruction in children with trisomy 21. J AAPOS. 2000;4:230–232.
- ↑ Smith C. Screening Corneal Tomography as a Helpful Adjunct in the Diagnosis of Keratoconus in Children with Down Syndrome. Oral Presentation at American Association of Pediatric Ophthalmology and Strabismus Annual Meeting; March 26, 2022; Scottsdale, AZ
- ↑ Frantz JM, Insler MS, Hagenah M, et al. Penetrating keratoplasty for keratoconus in Down’s syndrome. Am J Ophthalmol. 1990;109:143–147.
- ↑ Hashemi H, Amanzadeh K, Seyedian M, et al. Accelerated and Standard Corneal Cross-Linking Protocols in Patients with Down Syndrome: A Non-inferiority Contralateral Randomized Trial. Ophthalmol Ther. 2020. 9:1011–1021. https://doi.org/10.1007/s40123-020-00303-4
- ↑ Catalano RA, Simon JW. Optic disk elevation in Down’s syndrome. Elsevier Inc.; 1990:28–32.