Tear Trough Deformity
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
The tear trough is a hallowed and sunken area in the skin between the lower eyelid and the cheekbone that originates in the inner canthus and extends to the midpupillary line and can occur due to inherited anatomical differences or aging.1 This deformity can either occur on its own or in conjunction with lower eyelid fat prolapse because of a thinned and weak orbital septum. Several management options have been extensively described including hyaluronic acid injections, fat grafting, fat repositioning and facial implants. In this article, we explore the anatomy, evaluation, and management techniques for the treatment of tear trough deformity.
Disease
Tear trough deformity occurs because of the ligamentous attachments of the periorbita to the orbital bones, accompanied by fat atrophy and the descent of the surrounding structures.[1]
Anatomy
The anatomy of the tear trough is complex, and it involves several important structures. The layers of this area include the skin and subcutaneous tissue, orbicularis oculi muscle, orbicularis retaining ligament, tear trough ligament, the infraorbital fat pads, and the maxillary bone. [1][2] [3] [4]
- The skin in the tear trough area is thin and has very little subcutaneous fat. [5]
- The upper cheek does have abundant subcutaneous fat, suborbicularis oculi fat, and portions of the malar fat pad, which contribute to the inferior border of the tear trough. [5]
- The orbicularis retaining ligament originates laterally as a reflection of the orbital septum joining a membrane derived from the preperiosteal fat over the zygoma. [6] The medial extent of this retaining ligament is variable, connecting with the orbicularis oculi muscle insertion and indirectly to the medial canthus. [6] The central portion of the retaining ligament is the weakest and distends differentially more with age, allowing for greater exposure of the central fat pad. [6] * The orbital septum is a layer of connective tissue that separates the orbit from the preseptal tissues. It attaches to the orbital rim in a structure named the arcus marginalis. [1] [2]
- The tear trough ligament is an osteocutaneous ligament that runs between the palpebral and orbital parts of the orbicularis oculi muscle. [4] [6] It commences medially, at the level of the insertion of the medial canthal tendon, just inferior to the anterior lacrimal crest, to approximately the medial-pupil line, where it continues laterally as the bilayered orbicularis retaining ligament. [4] [6]
- The infraorbital fat is divided into three distinct pads, lateral, central, and medial. [7] Due to aging, the globe descends within the orbit and the infraorbital fat is displaced anteriorly, causing the tear trough to deepen.
- The maxillary bone is the medial support of the upper cheek.[3] A forward projection of the bone of the upper cheek may cause the tear trough to appear deeper, and this may be more common in patients with either congenital or age-related maxillary hypoplasia. [3]
Etiology and Pathophysiology
Tear through deformity is most commonly the result of a multifactorial process. Age related changes such as fat atrophy, ligamentous weakening with resultant inferior displacement of the infraorbital fat, maxillary bone resorption often results in a tear trough deformity. (all references) Specifically, attenuation of the tear trough ligament which runs from the medial canthus to the maxilla, results in descent of the superior orbital fat pads and formation of a prominent tear trough deformity. [1][3][4][6][8] Additional weakening of the orbicularis retaining ligament and the orbitomalar ligament also contribute to the formation and severity of the tear trough deformity. 8 The prominence of the maxillary bone can influence the development of a tear trough deformity through similar changes in the soft tissues and ligaments in the midface region. [3] In patients with a prominent maxillary bone, there may be a more significant gap between the bone and the skin in the tear trough area, which can lead to a loss of support for the soft tissues in this region. [3] Additionally, the maxillary bone can influence the position and tension of the tear trough ligament which may be pulled more tautly over the bone, resulting in a deeper tear trough depression. [3]
Other etiologies that may contribute to prominent tear trough deformity and overall facial volume loss include:
- Smoking status
- Sun exposure
- Medications: chemotherapeutic or corticosteroid drugs
- Hormonal imbalances: hyperthyroidism, decrease in estrogen, other hormonal imbalance
- Poor nutrition
- Autoimmune diseases: scleroderma, Sjogren’s, systemic lupus
- Psychological process: bulimia nervosa
Diagnosis
History
Patients that present with complaints of a tear trough deformity may have difficulty articulating their exact concerns, and may focus on fat prolapse, wrinkles or other findings that contribute to the “under-eye hollows”. The physician should perform a complete and detailed history and inquire about medical conditions, medications, previous facial or ophthalmic surgeries, trauma and previous injectables in the face. It is also important to define the patients’ goals and expectations.
Physical examination
All patients presenting with a desire for aesthetic rejuvenation of the tear trough deformity should have a thorough history and examination that include:
- A comprehensive facial examination, including an evaluation of the position and symmetry of the lower eyelids, the cheek volume and contour, and the overall facial balance.
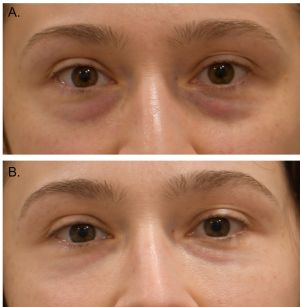
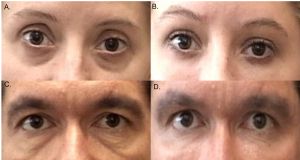
- Assess the depth and extent of the tear trough deformity, including the presence of shadowing or dark circles, orbital fat prolapse, and skin laxity and quality.
- Assess the volume and contour of the cheeks, which can influence the appearance of the tear trough hollowing.
- Evaluate the presence of volume loss or tissue descent in the midface, which can exacerbate the tear trough deformity and may be managed with other options.
- Obtain standardized photographic documentation (front and side views) and measurements to track changes in the tear trough and midface.
Signs and Symptoms
The patient may present with aesthetic concerns regarding tear trough aging that include:
- Dark circles or shadowing under the eyes: Due to the depression (volume loss and facial descent) under the eye, a tear trough deformity can cause a shadowed effect that gives the appearance of dark circles under the eyes. However, dark shadows or circles can also be due to congenital, vascular, or epidermal pigmentation etiologies.
- Under-eye bags or puffiness: A tear trough deformity may be accompanied by under-eye bags or puffiness, because of fat prolapse due to weakened and thin orbital septum, which can exacerbate the appearance of the deformity.
- Tired or aged appearance: Patients often express that they appear tired or aged, even in individuals who are well-rested or young.
- Fine lines or wrinkles: The tear trough area can be prone to fine lines or wrinkles, especially in individuals who have lost volume or elasticity in the soft tissues.
- Skin laxity: In some cases, a tear trough deformity may be accompanied by skin laxity or sagging in the lower eyelid or cheek area.
Management
General treatment
The objective of treating the tear though deformity is to restore volume and enhance the eyelid-cheek junction to create a smooth and youthful appearance. There are various nonsurgical and surgical options available, such as hyaluronic acid or filler augmentation, fat grafting or fat transfer, or placement of a facial implant. These approaches may or may not be combined with other management modalities to address other cosmetic concerns such as lower eyelid fat prolapse, or bags. Skin laxity and texture are often treated with laser or chemical peels to optimize results.
Nonsurgical Management
Fillers
Dermal fillers are substances that are injected into the skin to enhance facial contours, fill wrinkles and fine lines, and restore or augment facial volume. [9] [10] [11] The pharmacology of facial fillers depends on the type of filler used. The most common type of filler is hyaluronic acid (HA), a natural substance found in the body that maintains hydration and volume in the skin. [9][12] Synthetic HA fillers work by attracting and retaining water molecules to add volume to the skin. The duration of the effect of HA fillers varies from several months to a year. Calcium hydroxylapatite (CaHA) fillers, which are made of a naturally occurring mineral found in bone, stimulate collagen production, and provide long-lasting results that can last up to 2 years. Poly-L-lactic acid (PLLA) fillers stimulate collagen production and offer gradual and long-lasting improvement in facial volume and skin texture that can last up to 2 years.[12] Other types of facial fillers include polycaprolactone (PCL), which stimulates collagen production, and autologous fat transfer, which involves transferring fat from one part of the body to the face. There are different injection techniques for various areas of the face. Some of the most common techniques include:
- Linear threading technique: This involves injecting small amounts of filler along multiple parallel lines, which can help to restore volume and contour.
- Fanning technique: This involves injecting small amounts of filler in a fan-like pattern to help distribute the filler evenly.
- Cross-hatching technique: This involves injecting small amounts of filler in a grid-like pattern.
- Depot technique: This involves injecting larger amounts of filler in a single location to create a more dramatic effect, such as a pronounced temple hollow.
An important consideration is the depth of injection. Filler injections that are too superficial may lead to uneven surfaces or “bumps”, while deeper or even preperiosteal injections may lead to dramatic improvement but often require larger amounts of injectables.
Complications
Complications are rare but may include:
Bruising and swelling
Bruising and swelling are common after facial filler injections and typically resolve within a few days to a week. The use of arnica montana, an agent that has been reported to reduce bruising, is controversial, but has proven effective in some surgical procedures.[13] [14]
Infection
Infection is a rare but serious complication. Signs of infection include redness, swelling, and pain at the injection site. It is suspected that most infections are the result of skin organisms that penetrate the injection site. Topical cleansing with 70% alcohol is recommended prior to facial injections to reduce the risk of infections. Biofilms infections are a particular consideration with filler, as they may be difficult to treat. Biofilms are microorganisms that are proximal to an inert surface and thus poor vascular irrigation is observed. This leads to a decreased concentration of antimicrobial agents when treated. Atypical mycobacteria are a concern in these situations and may require treatment with clarithromycin for adequate coverage.[13] Oral herpes activation has also been reported with facial fillers and can be treated with antivirals. [13]
Allergic reaction
Although rare, some individuals may develop an allergic reaction to the filler material. Reactions may be because of hypersensitivity type I and immediate pruritus’, swelling and in severe cases difficulty breathing or anaphylaxis might be observed. [14] Hypersensitivity type 4 reactions will be delayed and can present as swelling, redness, pruritus’ and a sterile collection that often requires excision or removal of the filler. Treatment consists of antihistamines, corticosteroids, and hyaluronidase injections. [14]
Granulomas
Granulomas are small, firm bumps that can develop under the skin after a facial filler injection. They can be caused by a granulomatous foreign body reaction to the filler material and may require treatment with corticosteroid injections or surgical removal. [13]
Asymmetry
Asymmetry is a potential complication of facial fillers, particularly if they are not injected evenly or if the filler material migrates after injection.
Vascular occlusions
Injection of facial fillers that cause vascular occlusions can lead to devastating consequences and it is often the most feared complication of facial filler injections. Two types of vessel occlusions have been described: arterial with anterograde or retrograde embolic occlusion and venous. Inadvertent canulization of an artery may lead to a filler embolus that travels anterograde and causes distal ischemic occlusion of the smaller vessels leading to tissue necrosis. [13] [14] This will often present as an area that is pale and painful. An arterial occlusion with a retrograde embolus may travel to an adjacent vessel and lead to a central retinal artery occlusion or a cerebrovascular accident. [13] Venous occlusion is often painless, and leads to venous mottling appearance, termed livido reticularis. Different modalities of injections have been recommended to avoid vascular complications including the use of cannula, injecting while retracting the needle and the use of low and slow injection pressure. The management of a vascular complication includes generous hyaluronidase injection into the area to dissolve the filler material, warm compresses, and hyperbaric oxygen.
Migration
Filler material can migrate away from the injection site, leading to an unnatural appearance or the formation of lumps or bumps. [13] [14] Cases of migration into the orbit from distant injection sites have also been reported, with need for further intervention such as orbit exploration and removal of the filler. [15]
Covid-19 associated swelling
Rare and self-limiting swelling following vaccination or covid-19 infection has been reported. The main management strategy involves observation as most of these cases have been shown to be resolved within 2 weeks without intervention. Hyaluronidase can be employed if no resolution is observed after 2 weeks. [16]
Surgical Management
Fat Grafting
Fat grafting has gained popularity as an effective method for addressing tear trough deformity. Fat grafting involves the harvest of fat, the preparation/filtration of the fat and the injection into the recipient site. [1] The most common harvest site for fat grafting is the abdomen, although alternative sites such as the thighs or buttocks can also be utilized. The procedure begins with the administration of local anesthesia and abundant amount of tumescent anesthesia to the harvest site. Tumescent anesthesia is the mixture of local anesthetic with saline, and it is frequently used to facilitate dissection and harvesting in several procedures. The preparation of tumescent anesthesia depends on surgeon preference. It is the author’s preference to use tumescent anesthesia of 1% lidocaine with epinephrine. For example, to prepare a 1% tumescent anesthesia if it’s determined that 500 mL of volume is required, then 5 mL of lidocaine with epinephrine would be mixed with 495 mL of saline. This is subsequently injected into the harvesting site to facilitate the extraction of the fat cells. A small incision is made in the harvest site, which in the abdomen would be in the umbilicus. Liposuction is then performed. This can be done with a large syringe with a liposuction cannula, in a superficial, subcutaneous plane and using a back-and-forth motion. A red to orange colored fluid with fat particles will be collected into the syringe. The procedure is continued until an adequate amount of fat has been retrieved, which may vary depending on the patient. Once the fat is harvested, it is left resting for several minutes so that gravity may separate the fat from the tumescent anesthetic, which will settle inferiorly in the syringe. This fluid can be carefully discarded, while keeping the fat substrate for injection. This extracted fat now undergoes a purification process in which it is passed through several specialized filters to remove cellular debris, blood and keeping progressively smaller and finer fat substrate. The purified fat is then ready for injection. The fat can be injected with a cannula or with a needle in the same manner as facial fillers. The injection depth should be deep in a pre-periosteal plane. Typically, a surgeon will opt to overfill the area mildly since some fat will be resorbed. There are several advantages to fat grafting including cost, no risk of allergic reaction or rejection and the possibility that the transferred cells will establish a blood supply leading to permanent volumizing effect. Disadvantages of this approach include an unpredictable resorption rate that may lead to revisions, or uneven appearance and a second morbidity site. Possible risks include bleeding from both harvest site and donor site, infection, pain, over or under correction, vascular occlusions that lead to blindness or skin necrosis, scarring and asymmetry.
Implants
Maxillary bone loss is a known component of tear trough deformity. [2][17] Augmenting the skeletal projection anteriorly can alleviate the volume loss that characterizes tear trough deformity. [2][17] A tear trough implant is an excellent option for negative vector patients, that is a posterior relation between the globe and orbital rim due to maxillary bone loss. Several options are available, silicone implants are some of the most used tear trough implants. [2][17] The implants are available in different sizes and the use of sizers is recommended to select the optimal option. [17] The implant requires sculpting intraoperatively to form the crevice where the infraorbital bundle will rest. The most common approach for tear trough implantation is transconjunctivally. A transconjunctival incision is made approx. 4 mm below the level of the tarsus with dissection in the pre-septal plane towards the orbital rim. [2][17] Once the rim is exposed, the periosteum is incised and elevated with Freer elevators. Dissection is then directed inferiorly, taking care medially for the infraorbital bundle and laterally for the zygomaticofacial nerve. Periosteum elevation should proceed in a conservative manner, to avoid an extended dissection and possible implant migration. Once the periosteum has been elevated, the implant may be placed. The implant must rest against the bone, without any tension or movement as this will increase the risks of migration. Fixation is optional, if the implant is properly placed without tension, no fixation is needed. Some surgeons advocate for screw fixation of the implant into the bone. Periosteum closure is followed, and it is a very important step, as it also reduces the risks of migration. At this point, the surgeon may opt to proceed with any other surgical procedures that the patient may require such as a lower blepharoplasty. The advantages of implant placement include no harvest site, permanent results, and a faster procedure. [2][17] The disadvantages of this approach include costs. Complications of this surgery include the risks of infection; implants may develop a biofilm of bacteria that may be resistant to antibiotics and may require removal. Additionally, the risks of migration, under or over-correction and/or scarring. [2][17]
Lower Blepharoplasty with Fat Transposition
Tear trough deformity is often addressed in conjunction with lower blepharoplasty. [1] [2] [7] This will ensure optimal eyelid cheek junction, as it will remove the anterior projection of the prolapsed orbital fat and the posterior volume loss of the tear trough. [1] [2] [7] A lower blepharoplasty with fat transfer to the tear trough may address both cosmetic concerns. The indications and considerations are like those described above. There are several techniques to perform this procedure, with one of the most common being the Goldberg technique. [2] The eyelids are everted, and an incision is made 4 mm below the level of the tarsus, and dissection is directed inferiorly towards the orbital rim in a pre-septal plane. Once adequate exposure has been achieved, the septum is opened, and the orbital fat pads are visualized. The lateral and central fat pads are carefully sculpted. Special attention is taken with the inferior oblique muscle which is localized between the medial and central fat pads. The orbital rim is then exposed and the arcus marginalis is opened and using cautery the periosteum is also opened and elevated, creating a subperiosteal pocket. The medial fat pad is fashioned into a pedicle which can then be moved into the subperiosteal plane, if additional volume is required, the central fat pad may be transposed as well. The fat transposition is secured with externalized sutures, which can be removed 3-5 days after surgery. Bolsters may be used to soften the suture pressure on the skin. A modification to this technique has been proposed that includes placing the fat pads in a pre-periosteal plane which would improve vascularization to the transposed fat. [2]
Prognosis
Improvement of tear trough deformity is generally good but depends on the modality of management, general health and comorbidities of the patient, environmental factors, and continued aging.
Facial Fillers
HA fillers offer immediate and nonsurgical correction of tear though deformity. The longevity of filler results in the tear trough area can vary depending on factors such as the type of filler used, individual metabolism, and lifestyle factors. On average, HA fillers can provide improvement for approximately 9 to 12 months. Periodic maintenance treatments can help sustain the desired outcome.
Fat Grafting
Fat grafting offers promising long-term results. The transferred fat cells, once integrated into the surrounding tissues, tend to establish a stable blood supply, increasing their chances of long-term survival. Over time, the injected fat cells exhibit natural volume restoration, helping to alleviate the hollow appearance and improve the contour of the under-eye area. While some initial swelling and bruising may occur, these typically subside within a few weeks, allowing the final results to become apparent. It's important to note that the longevity of fat grafting results can vary among individuals. Some patients may experience a gradual reduction in volume over time, necessitating touch-up treatments to maintain the desired outcome. However, for many patients, fat grafting can provide a long-lasting and natural solution to tear trough deformities.
Facial Implants
Facial implants offer a predictable and enduring solution for tear trough deformity correction. Once the implants are properly placed, they maintain their shape and volume, delivering long-lasting outcomes. Facial implants provide a stable and consistent correction, addressing the hollowing and improving the overall contour of the under-eye area. The prognosis for facial implants is generally positive, with patients experiencing a significant improvement in tear trough deformities. However, it is important to consider that individual healing and implant integration can vary. In rare cases, complications such as implant shifting, malposition, or extrusion may occur, necessitating revision surgery.
Fat Transposition
Lower blepharoplasty with fat transposition offers a permanent correction for tear trough deformities. By utilizing the patient's own fat pads, the procedure achieves long-lasting volume restoration and improved contouring of the under-eye area. Once the fat pads are repositioned, they establish a stable blood supply and integrate with the surrounding tissues, enhancing the long-term stability of the correction. This reduces the likelihood of future volume loss and maintains the desired results over time.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Jiang J, Wang X, Chen R, Xia X, Sun S, Hu K. Tear trough deformity: different types of anatomy and treatment options. Postepy Dermatol Alergol. 2016;33(4):303-308.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Stutman RL, Codner MA. Tear trough deformity: review of anatomy and treatment options. Aesthet Surg J. 2012;32(4):426-440. PMID: 22539575.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Haddock NT, Saadeh PB, Boutros S, Thorne CH. The tear trough and lid/cheek junction: anatomy and implications for surgical correction. Plast Reconstr Surg. 2009;123(4):1332-1340; discussion 1341-1342. PMID: 19337097.
- ↑ 4.0 4.1 4.2 4.3 Wulc AE, Sharma P, Czyz CN. The tear trough ligament: anatomical basis for the tear trough deformity.Plast Reconstr Surg Glob Open. 2012;129(6):1392-1402.PMID: 22634665. 10.Gladstone GJ, Black EH, Nesi FA.Treatment of the tear trough deformity with hyaluronic acid.Dermatol Surg .2009;35 Suppl 1:482-488.PMID:19207361.
- ↑ 5.0 5.1 Ugradar S, Kim JS, Massry G. A review of midface aging. Ophthalmic Plastic & Reconstructive Surgery. 2023;39(2):123-131.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Muzaffar AR, Mendelson BC, Adams WP. Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg. 2002;110:873–84. discussion 897-911.
- ↑ 7.0 7.1 7.2 Rohrich RJ, Ghavami A, Mojallal A. The five-step lower blepharoplasty: blending the eyelid-cheek junction. Plast Reconstr Surg 2011;128:775–83
- ↑ O J, Kwon HJ, Choi YJ, Cho TH, Yang HM. Three-dimensional structure of the orbicularis retaining ligament: an anatomical study using micro-computed tomography. Sci Rep. 2018;8(1):17042.
- ↑ 9.0 9.1 Rohrich RJ, Ghavami A, Crosby MA. The role of hyaluronic acid fillers (Restylane) in facial cosmetic surgery: review and technical considerations. Plast Reconstr Surg. 2007;120(6 Suppl):41S-54S. PMID: 18090748.
- ↑ Goldberg RA, Fiaschetti D. Filling the periorbital hollows with hyaluronic acid gel: initial experience with 244 injections. Ophthal Plast Reconstr Surg. 2006;22(5):335-341; discussion 341-343. PMID: 16985415.
- ↑ Sharad J. Dermal fillers for the treatment of tear trough deformity: A review of anatomy, treatment techniques, and their outcomes. J Cutan Aesthet Surg. 2012;5(4):229.
- ↑ 12.0 12.1 Yag-Howard C, DeNigris J. Novel Filler Technique: Hyaluronic acid and Calcium hydroxylappetite mixture resulting in favorable esthetic and longevity outcomes. International Journal of Women’s Dermatology. 2021;7(5):817-819.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 Woodward J, Khan T, Martin J. Facial filler complications. Facial Plastic Surgery Clinics of North America. 2015;23(4):447-458.
- ↑ 14.0 14.1 14.2 14.3 14.4 Chiang YZ, Pierone G, Al-Niaimi F. Dermal fillers: pathophysiology, prevention and treatment of complications. J Eur Acad Dermatol Venereol. 2017;31(3):405-413.
- ↑ Hamed-Azzam S, Burkat C, Mukari A, et al. Filler migration to the orbit. Aesthetic Surgery Journal. 2021;41(6):NP559-NP566.
- ↑ Ng C, Tay E, D’Souza A. Localised swelling at sites of dermal filler injections following administration of Covid-19 vaccines: a systematic review. SINGAPORE MED J. 2023;0(0):0.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 Flowers RS, Kanodia R, Donenfeld A, et al. Tear trough implants for correction of tear trough deformity. Clin Plast Surg. 1993;20(2):403-415; discussion 416-417. PMID: 8494408.