Sensory and Motor Testing
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
History
Prior to initiating testing, it can be helpful to obtain a history regarding the misalignment of the eye. The following information may be helpful in determining what type of sensory and motor testing is needed.
Characterize the deviation: Which eye is most often deviated and in what direction? Does the other eye deviate as well? How often does it occur? How long does the deviation last when it occurs? Is it noted at distance and near? When was the deviation first noted?
Characterize the patient symptoms: Does the patient have diplopia? If yes, is it binocular or monocular (note that a patient can have bilateral monocular diplopia)? Do they have issues with depth perception? Do they have a sense of eye strain or frequent headaches?
Ocular history: Is there a history of poor vision in one eye compared to the other? Have they previously been prescribed glasses? Have they previously been prescribed prism glasses? Has the patient had amblyopia treatment in the past? Have they have eye alignment surgery in the past?
Observation
Prior to initiating testing, observe the patient. This can be done while obtaining a history. Note any obvious misalignment of the eyes that is manifesting spontaneously, how much of the time it is occurring, and if there is a fixation preference. Look for any abnormal head position or nystagmus. Note any ptosis.
Assessment of Eye Movements
Ocular Rotations
Ductions are uniocular rotations of the eye. Versions are simultaneous rotations of the two eyes in the same direction. Typically versions are tested first to help evaluate for subtle imbalances in eye movements. If versions are not full, ductions may be tested on one eye with the other eye covered. This could be helpful, for example, when testing abduction in a patient with infantile esotropia who cross-fixates, leading to an apparent abduction deficit on versions, but normal abduction when tested monocularly.
Ocular motility is typically noted on a scale from 0 to 4. Zero indicates normal ductions. Underaction is indicated with a minus sign and overaction is indicated with a plus sign. For example, an eye that cannot abduct past the midline due to a CN VI palsy would be noted as -4. A left eye with moderate overelevation in adduction would be noted looking up and in as +2. Occasionally, limitation of a duction is sufficiently severe that the eye cannot make it to midline, this duction would be noted as >4.
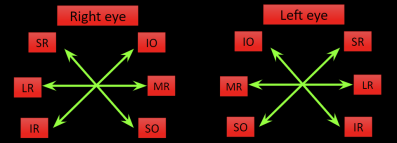
Diagnostic Positions of Gaze
Eye alignment is typically checked in 9 positions:
Primary position: the head is straight and the eyes are fixated straight ahead
6 cardinal positions: These correspond to the primary field of action of the extraocular muscles. The muscle indicated for each cardinal position is the primary muscle responsible for moving the eye into that position. For example, when the eye is adducted, the inferior oblique elevates the eye; when the eye is adducted the superior oblique depresses the eye. Of note, the cardinal positions are not the same as the muscles' actions. For example, the oblique muscles have a tertiary action as abductors of the eye, but their function is tested in adduction; the opposite is true for the vertical recti.
Upgaze and downgaze: These are impacted by both the vertical recti and oblique muscles.
In patients with a vertical misalignment, right and left head tilt should also be assessed.
The amount the eye is deviated may be the same in all positions of gaze (comitant) or vary depending on the position of gaze (incomitant).
Assessment of Eye Alignment
There are a few ways to detect strabismus (deviating eyes) on a patient depending on their visual acuity and whether or not they are verbal. Eyes can be deviated inward (esotropia), outward (exotropia), upward (hypertropia), downward (hypotropia), intorted (incyclotorsion/ intorsion), or extorted (excylcotorsion/ extorsion).[1]
The relative position of the eyes can be assessed by multiple different methods. Cover testing is usually preferred, when possible, but requires that the patient has foveal fixation in both eyes, can move their eyes, and is has sufficient attention and cooperation for the test. Evaluation of the light reflex with Hirschberg or Krimsky testing can be used if these criteria cannot be met. Hirschberg and Krimsky can also be used to estimate the deviation prior to cover testing.
Hirschberg (H) Test
The examiner evaluates for symmetry of the corneal light reflex.[1] This can be useful as an initial estimate of alignment. It may also be used in children who will not allow for either cover or Krimsky testing.
Procedure/Interpretation
A muscle light or penlight is used at 1/3 of a meter and patient is asked to fixate on the light. If the light reflex is centered in both eyes, the patient does not have a manifest misalignment. If the light reflex is displaced, it shows a manifest misalignment. The amount of decentration can be used to estimate the degree of the misalignment. 1 mm of displacement is roughly 7 degrees or 15Δ. For example, the light reflex at the pupillary margin is about 2 mm from the center (with a normal 4 mm pupil). This corresponds with 15 degrees or about 30Δ. The mid-iris region is about 4mm from the center of the pupil, which is about 30 degrees or 60Δ. A reflex at the limbus is about 45 degrees or 90Δ.
If the light reflex is displaced nasally, the patient has an exotropia. If the light reflex is displaced temporally, the patient is esotropic. If the light reflex is displaced inferiorly, the eye is hypertropic. If the light reflex is displaced superiorly, the eye is hypotropic.
Krimsky (K) Test
Procedure/Interpretation
As in the Hirschberg test, a light is shone from 1/3 meter and the patient is asked to fixate on the light. If the light reflex is decentered a prism is placed in front of the deviating eye or the fixating eye (modified Krimsky test) to correct the deviation of the corneal light reflex. The strabismus measurement is equal to the amount of prism necessary to center the corneal light reflex on the pupil of the deviating eye. A base-in (BI) prism is used to neutralize an exotropia. Base-out (BO) prism is used to neutralize an esotropia. Base-down (BD) is used to neutralize a hypertropia. Base-up (BU) is used to neutralize a hypotropia.
Angle Kappa: The angle between the visual axis and the anatomical pupillary axis is called the angle kappa. When the fovea is temporal to the pupillary axis, it is called a positive angle kappa and simulates an exotropia. When the fovea is nasal to the pupillary axis, it is called a negative angle kappa and simulates an esotropia.[2] It is important to note the light reflex is usually slightly nasal, even in an orthophoric patient.
Latent deviations: For patients without manifest strabismus initially upon evaluation with a corneal light reflex test, each eye can be covered for several seconds to see if a deviation can be brought out and quickly followed by quantification of the angle of deviation with Hirschberg or Krimsky testing.
Cover-Uncover (Single Cover) Testing
https://eyewiki.aao.org/Cover_Tests
In patients who have a deviation and are able to fixate on a distance and near target, cover tests offer the most accurate measurement of the degree of misalignment.
A cover-uncover test picks up manifest deviations (deviations that are always present).
Procedure/Interpretation
The patient is asked to fixate on an object. A cover is introduced over the first eye for 1-2 seconds. As the eye is covered the uncovered eye is observed for movement. The cover is removed and again shift in fixation is noted. The same is repeated, covering and uncovering the contralateral eye.
The following observations can be made:
- No shift of either eye with cover of each eye: orthotropia, the patient has no manifest deviation
- Shift of one uncovered eye: unilateral manifest deviation (tropia)
- Shift of both uncovered eyes: alternating manifest deviation (tropia). [2][1]
Assessment of Control
In patients with manifest strabismus, assessment of control of the strabismus can be helpful in determining management of the patient.
Aspects of control include:
1) The percent of time the strabismus is manifest prior to dissociation
2) How many covers does it take to dissociate the patient on alternate cover testing
3) How long does it take the patient to recover normal alignment after dissociation with alternate cover or occlusion
Different scales exist to help quantify control. The intermittent exotropia clinical control score developed by Dr Mahoney and Dr. Holmes is a commonly used example.
Intermittent Exotropia Clinical Control Scale[3]
5= Constant exotropia
4= Exotropia >50% of the exam before dissociation
3= Exotropia <50% of the exam before dissociation
2= No exotropia unless dissociates, recovers in >5 seconds
1= No exotropia unless dissociated, recovers in 1-5 seconds
0= No exotropia unless dissociated, recovers in <1 seconds (phoria)
This is performed in primary gaze at distance and near fixation. Levels 5 to 3 are assessed during an initial 30 second period of observation. Levels 2 to 0 are graded as the worst of the three rapidly successive trials. An occluder is placed over the right eye for 10 seconds and then removed, measuring the length of time it takes for fusion to become re-established. The left eye is then occluded for 10 seconds and the time to re-fusion is measured. A third trial of 10 seconds of occlusion is performed, covering the eye that required the longest time to re-fuse. The worse level of control observed following the 3, 10-second periods of occlusion should be recorded for that visit.
The Newcastle or NIDEX Scale[4] takes into consideration parental reports of control at home in addition to an objective control score in the office.
Simultaneous Prism and Cover Test
In patients who have a manifest deviation on cover-uncover testing, the simultaneous prism and cover test can be used to measure the angle of the manifest deviation (without picking up additional latent deviation). This is likely a more accurate measure of the patient’s deviation in real life settings.
Procedure/Interpretation
A prism is placed over the deviating eye at the same time as the fixing eye is covered. The prism can be adjusted until there is no further movement of the deviating eye.
Alternate Cover Testing
Alternate Cover Testing (ACT) determines the total amount of manfiest and latent deviation of the eye. A cover-uncover test is done before moving on to alternate cover testing.
Procedure/Interpretation
The alternate cover test (shifting cover from eye to eye) will bring out the phoric portion. Prisms are used in Alternate Prism Cover Test to measure the degree of the deviation.
On both of these testing methods, it is important to occlude each eye long enough so the patient has time to take up fixation with the uncovered eye as the occluder is shifted back and forth. This is especially true if one eye is amblyopic. An accurate way to measure strabismus correctly is to measure to reversal. [2][1]
Primary and Secondary Deviations
For incomitant deviations, the primary deviation is the deviation when the normal eye is fixating in the primary position. The secondary deviation is the deviation when the misaligned paretic or restricted eye is fixating in primary position. The patient will typically fixate with the eye that does not have the prism over it. The secondary deviation is larger. As stated in Hering’s law, there is equal innervation of the yoke muscles, so that the eyes can move together. The increased innervational impulse needed to bring the paretic or restricted eye straight also leads to a greater innervational impulse to the yoke muscle in the contralateral eye, which leads to a greater deviation than when the normal eye is fixating.
Three Step Test for Cyclovertical Muscle Palsy
The three-step test, also known as the Parks-Bielschowsky three-step test or the Parks-Helveston three-step test, is a diagnostic test used to identify which muscle is paretic in the case of an acquired hypertropia. It is designed for the diagnosis of a single paretic vertical muscle. Many other causes of vertical strabismus can result in a positive three step test, including contracture of the vertical recti, paresis of more than one vertical muscle, dissociated vertical divergence, previous vertical muscle surgery, skew deviation, myasthenia gravis, and small nonparalytic vertical deviations associated with horizontal strabismus.[5]
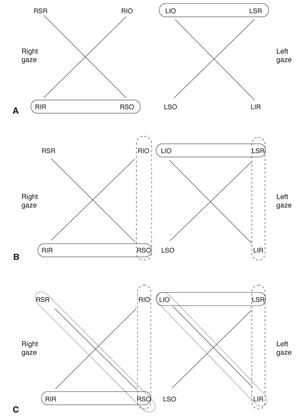
Procedure/Interpretation
The prism and alternate cover test is used to quantify misalignment of the eyes in primary position, side gazes, and head tilts. Smaller deviations may be quantified using prisms and a Maddox rod or red filter. [6]
Using these measurements:
- Determine which eye is hypertropic in primary position.
- The impacted muscle will be a depressor of the higher eye (inferior rectus or superior oblique) or an elevator of the lower eye (superior rectus or inferior oblique)
- Determine whether the hypertropia increases on right or left gaze.
- If worse in left gaze, for a paretic muscle, the superior or inferior oblique muscle in the right eye or the superior or inferior rectus in the left eye is affected
- If worse in right gaze, for a paretic muscle, the superior or inferior oblique muscle in the left eye or superior opr inferior rectus muscle in the right eye is affected
- Determine if the hypertropia increases upon left head tilt or right head tilt.
- If worse in right tilt, the right eye intorters (superior oblique and superior rectus) or left eye extorters (inferior oblique and inferior rectus) are affected
- If worse in left tilt, the left eye intorters (superior oblique and superior rectus) or right eye extorters (inferior oblique and inferior rectus) are affected
An easy way to isolate the paretic muscle is to draw the field of action for the vertial recti and oblique muscles in each eye. As you go through steps 1-3 above, circle the candidate muscles in each step. The muscle identified as a candidate in all three steps is the paretic muscle, if the deviation is actually due to a muscle paresis. See Figure 2 for an example. Failure to isolate a muscle should raise concern for a skew deviation.
The Upright-supine test
This test is used to differentiate between a skew deviation from other causes of vertical strabismus and is sometimes considered as a fourth step in the three step test described above. A skew deviation is a vertical misalignment of supranuclear origin (brainstem or cerebellum) that may or may not have associated head tilt or fundus torsion.
Procedure/Interpretation
The deviation is measured in primary position using the prism and alternate cover test with fixation at 1/3 meter both upright and supine. A vertical strabismus that decreases by 50% of more is considered a positive test for a skew deviation and may prompt neurological work-up, in the appropriate clinical setting. Reported sensitivity for a skew deviation is 80% and specificity is 100%.[7]
Sensory Testing
Sensory tests determine the fusional status and binocularity of the patient.
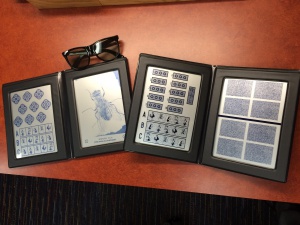
Titmus or Randot
Introduction
These tests are used the most often to quantify stereopsis, it can also be used to detect ARC (abnormal retinal correspondence). The level of dissociation is moderate. This test should be done on all patients who are bi-foveal and can be used as a quick screening to see if the patient is using two eyes together. Patients with deviations of 8Δ or less should also be tested as well as patients with constant tropias, as the presence of stereopsis indicates that the deviation is actually intermittent. The test can also uncover malingering in a patient claiming severe vision loss or blindness in one eye. [8][9]
Procedure
The patient is directed to put on polarized glasses. They are then shown a book with stereoscopic images (3-dimensional) and 2-dimensional images. The patient is asked to identify which pictures are stereoscopic. The book either has a titmus fly or a randot stereogram. The other side of the book has stereoscopic animals and circles. It is typical to ask the patient to identify the animals after the fly or shapes and the circles last.
Interpretations
The “titmus fly” is considered to be 3000 seconds of arc where as the “9th circle” is about 40 seconds of arc. Some could argue that the titmus fly gives off monocular clues that allow patients with reduced stereo to able to identify the image. One way to verify if the patient truly has stereopsis is to flip the book at a 90 degree angle, the image should appear 2-dimensional. Falsely good stereopsis is very common when using the titmus fly because it is the most commonly used stereopscopic test.[8][9] Conditions such as strabismus and amblyopia can reduce stereopsis, however, some degree of stereopsis can be seen in patients with anisometropic amblyopia or small angle strabismus of 8 prism diopters or less (as noted in Park’s Monofixation Syndrome).[9] If a patient has reduced stereopsis, it would be beneficial to then test them with the Worth 4 Dot to confirm fusion status or if in fact they have a central suppression scotoma consistent with Monofixation Syndrome.
4Δ Base Out Test
Introduction
The purpose of this test is to detect a small central suppression scotoma (or foveal suppression). The level of dissociation is mild. It can be used with patients who have decreased stereopsis but are orthophoric on cover testing. This test can also be used on patients with small to intermediate angle deviations, and with patients with Monofixation Syndrome.[8]
Procedure
Instruct the patient to look at a distance target. A 4-BO prism is quickly placed over one eye and the movements of both eyes are observed.
Interpretations
Normal response: Both eyes shift in the direction of the apex of the prism followed by convergence of the eye without prism. A sudden displacement of the image onto the parafovea in the eye with the prism will cause the eye to shift toward the apex of the prism. Due to Hering’s law of equal innervation, the fellow eye will shift the same magnitude in the same direction at the same time. The fellow eye will then converge to avoid diplopia.
Foveal suppression scotoma: Failure of the eye with the prism to shift in response to prism placement indicates suppression of ipsilateral eye. Failure of the contralateral eye to converge indicates foveal suppression of the contralateral eye.[8][1]
Bagolini Glasses
Introduction
Bagolini glasses do not have dioptric power but have narrow striations running parallel in one meridian. This test is used to determine the direction of a pseudofovea, abnormal retinal correspondence (ARC), and suppression. This test also is able to tell the examiner if the patient has peripheral-sensory fusion. This test is mildly dissociating so it will detect small ARC even in large angle strabismus. The Bagolini glasses also simulate life-like testing conditions, which makes it the least dissociating. A disadvantage to this test is that it is difficult for young children to appreciate because it requires reliable subjective responses.[10]
Procedure
If the examiner does not have access to a Bagolini Lens, Bagolini trial frames are placed at 135 degrees OD, 45 degrees OS. Patient is asked to look at muscle light or pen light. They will see a band of light perpendicular to the striations of the lens.
Interpretation
When a patient sees only one line at a time, the patient is suppressing. If patient sees two lines in an “A” or “V” arrangement, the patient is diplopic. You may offset the deviation with a prism and if the patient reports an X this confirms normal retial correspondence (NRC). The fusion response will always be some form of an “X” If the eyes are straight, and they see an X, this means NRC, if they are strabismic and report an X this means ARC.[8]
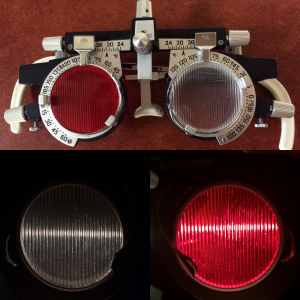
Double Maddox Rod
Introduction
This test is used to determine the presence of a cyclodeviation. This test is very dissociating. Clinically, it is useful to use this on patients who have a suspected 4th Nerve Palsy, or Thyroid Eye Disease.[10] It is also important to note that patients will usually tolerate excyclotorsion more than incyclotorsion.[8]
Procedure
Orient two Maddox rods (one white and one red) at 90 degrees, so the striations are vertical, in trial frames. When shown to the patient with a muscle light at 1/3 of a meter, the patient should see a red line and a white line. Instruct the patient to turn the knobs to rotate the lenses until both lines are horizontal. For a 4th Nerve Palsy, it could be helpful to put the red rod on the eye that is paretic.[8] It can be useful for the examiner to put the glasses on themselves to show the patient the trial frame and demonstrate use of the knobs.
Interpretation
If the lines are horizontal with the rods , there are 0 degrees of torsion. If the lines aren’t parallel, there is torsion present. The patient should be able use the knob to rotate the line until it is parallel line. If the rod has to be rotated inward, the patient has incyclotorsion. If the rod has to be rotated outward, the patient has excyclotorsion. The trial frame has an axis marked, so the examiner can determine the amount of torsion.
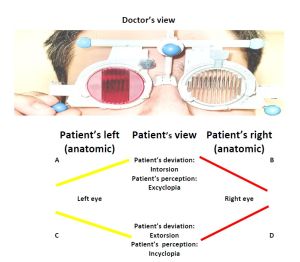
A patient that has globe excyclotorsion, sees incyclotorsion of the horizontal lines (incyclopia). In the other words, the nasal side of the horizontal lines are downward deviated towards his nose. The reverse is also valid, globe incyclotorsion cause excyclopia and the nasal side of horizontal line is seen upward deviated. Please see figure 5 and the videos.
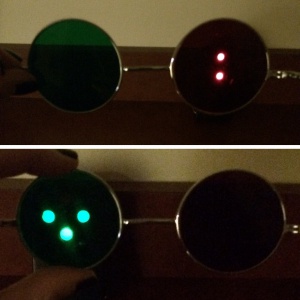
Worth 4 Dot
Introduction
The purpose of this test is used to detect peripheral sensory fusion and foveal suppression. The level of dissociation is high. This test can be used for any verbal child with any angle of strabismus especially with reduced stereopsis.[8]
Procedure
This can be done with the lights on or the lights off depending on what level of dissociation is preferred. With the lights off, the depth of suppression can be measured. Place the red-green glasses on the patient, with the red glass on the right eye. Ask the patient to report how many lights they see at the distance and at near (1/3 of a meter).
Note: With the right eye, thepatient should see two red lights and with the left eye, the patient should see three green lights. The examiner can also measure the boundary of suppression by testing the patient at the end of the room and walking closer to the patient.[8]
Interpretation
- Fusion at distance and near: Patient reports 4 lights. Fusion is only possible when the patient is bifoveal, which implies normal retinal correspondence.
- Suppression at near and distance: Patient sees 3 or 2 lights.
- Suppressing the right eye means the patient is not seeing the lights with the red glass; therefore they will report seeing 3 green lights.
- Suppressing the left eye means the patient is not seeing the lights with the green glass; therefore they will report seeing 2 red lights.
- Fusion at near, but suppression at distance: this is the classic response for Monofixation Syndrome, but this can also happen with patients who have a large deviation.
- Diplopia: Patient reports 5 lights. It is important to ask if the red and green lights are there at the same time. Patients can rapidly alternate suppression which can give a false diplopic response.
- In patients with NRC, an esotropia deviation should lead to uncrossed diplopia and an exotropia should lead to crossed diplopia. If they are opposite of what is expected with their deviation corrected, the patient likely has ARC.
- If a deviation is corrected by a prism, but the patient still reports diplopia, this indicates ARC. [8]
Red Filter Test
Introduction
The red glass test is used to detect the presence and type of diplopia a patient has. It can also be used to detect suppression, determine retinal correspondence, and to confirm the type of diplopia a patient has (crossed or uncrossed). This is a moderately disassociating test. Clinically, it is most useful to use this test on adults who complain of diplopia who seem orthophoric on cover testing. It is also a good way to fit adults with prisms. Testing children with the red filter can be difficult.[8]
Procedure
Place the red filter on the patient’s preferred eye while they fixate on a target or light, typically at distance. Ask the patient to describe where they see the red version of the fixation target relative to the normal appearing version of the fixation target.
Interpretation
Normal response or suppression: A single image is seen that appears red either indicates that they are fusing both eyes or suppressing the eye without the red glasses. Try switching the glass to the fellow eye. If they now only see a normally colored image, they are suppressing the fellow eye.
Alternating fixation: The red and white images will rapidly alternate.
Horizontal Diplopia: The red and white images are seen simultaneously. In a patient with an esotropia, the diplopia should be uncrossed, meaning that if the red glass is over the right eye, the red image should be to the right of the normal image. In a patient with an exotropia, the diplopia should be crossed, meaning that if the red glass is over the right eye, the red image should be to the left of the normal image. The red glasses test can be useful in determining the degree of ARC in patients who are diplopic at their corrected angle of strabismus.
Vertical diplopia: If the patient reports the red image above the white image, the eye with the red glass is lower/ hypotropic. If the red image is below the white, the eye with the red glasses is higher/ hypertropic.[8]
After Image
Introduction
This test is used to determine retinal correspondence and also can be used to detecting dense suppression. This is the most dissociating test for ARC. It also directly determines the direction of the fovea of the deviating eye. It is most useful for adults that can monocularly fixate precisely. It is useful to check on adults pre-operatively, especially if they have a long-standing intermittent exotropia. It will work with patients with eccentric fixation. This test is also too difficult for children.[8]
Procedure
First, turn out the room lights and occlude the non-dominate eye, orient the light in the direction of the strabismus. The dominant eye should be stimulated first with the horizontal beam for horizontal strabismus and vertical for vertical strabismus (the non dominant eye would get the opposite beam). The patient is directed to fixate on the lighted bar for 10 seconds so that the fovea is stimulated. The patient is instructed to close their eyes and observe the white lines (positive after image). With the lights on, the patient can be instructed to look at the blank wall and blinks to see the black lines (negative after image).[8]
Interpretation
If the patient reports “a cross,” the patient is fusing. This indicates NRC. If the patient reports one line, this indicates dense suppression. The After-Image test is designed to “break through” mild to moderate suppression. If the patient reports “Two lines, but no intersection in the middle,” they are diplopic.[8]
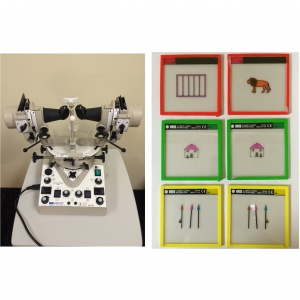
Amblyoscope | Synoptophore
Introduction
The amblyoscope is used to diagnose anomalies of binocular vision with targets that are presented to each eye. It gives the examiner detailed information of the sensory status of the patient. It can be used to detect and quantify suppression, determine retinal correspondence, measure the size and shape of a suppression scotoma, measure primary/secondary deviations, and determine fusional potential. Angle Kappa, Stereopsis, and Fusional amplitudes can also be measured on the amblyoscope. The level of dissociation can be little or highly dissociating depending on what the objective is. An amblyoscope exam can be given to any adult with a history of childhood onset strabismus pre-operatively, or if they need surgery at all, as with a cyclodeviation. It is also useful for adults who report diplopia, but have a hard time describing it. An amblyoscope exam on children can be difficult due to the need for reliable, subjective answers. It is important to do a full orthoptic work up before putting a patient on the amblyoscope.[8]
Procedure/Interpretations
The patient is instructed to put their chin on the chin rest. Chin rest and IPD can be adjusted accordingly. The examiner should use the toggle switches to show the patient the slide illuminated to right and left eye. The exam will proceed as the examiner switches the toggle from the right eye to the left eye. This is representative of cover testing. The eye that is illuminated is the eye that is fixating. The examiner should be able to see the eye movements and be able to neutralize a horizontal deviation by using the arms at the side of the machine. There is a scale near the arms to note the size of deviation. Neutralizing a vertical deviation requires the use of the R/L Hyper knobs. Cyclo deviations are also neutralized using the appropriate knobs. The goal of the examiner is to have the patient fuse the fusion targets. Near deviations can be neutralized by placing a -3.00 sphere trial lenses in the lens holder in front of the eyepiece. This way, the patient has to exert 3 diopters of accommodation to make the objects clear. There are different slides that can be used. The red slides (pictured above) are simultaneous perception slides that are used to test subjective and motor angles. They are also known as Worth’s Grade 1 slides. Grade 2 slides are green and are used to test motor and sensory fusion. The yellow slides are known has stereoscopic vision slides and are used to test the presence of third grade binocularity.
The amblyoscope is useful to see subjective and objective angles. The objective angle (motor angle) is what is seen on cover testing with the light source. The subjective angle (sensory angle) is noted when there is no shift and the deviation is neutralized, the images should be superimposed. In this case, the subjective angle and objective angle are the same. If the images are not superimposed, the patient is asked to move the left arm until the images are superimposed. This is the subjective angle. If there is a difference between the subjective and objective angle, this is called the angle of anomaly, which indicates ARC.[8]
Acknowledgments
All Images are Courtesy of the Ross Eye Institute and Kyle Arnoldi, CO COMT
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Iacobucci, Ida Lucy. Clinical Approach to Ocular Motility: Characteristics and Orthoptic Management of Strabismus. P.1-10
- ↑ 2.0 2.1 2.2 Cassin, Barbara. Fundamentals for Ophthalmic Technical Personnel. Philadelphia: Saunders, 1995. Page number
- ↑ Mohney BG, Holmes JM. An office-based scale for assessing control in intermittent exotropia. Strabismus. 2006 Sep;14(3):147-50. doi: 10.1080/09273970600894716. PMID: 16950743; PMCID: PMC2699414.
- ↑ Haggerty H, Richardson S, Hrisos S, Strong NP, Clarke MP. The Newcastle Control Score: a new method of grading the severity of intermittent distance exotropia. Br J Ophthalmol. 2004 Feb;88(2):233-5. doi: 10.1136/bjo.2003.027615. PMID: 14736781; PMCID: PMC1772020.
- ↑ Kushner BJ. Errors in the three-step test in the diagnosis of vertical strabismus. Ophthalmology. 1989;96:127-132.
- ↑ "Head Tilt Test." Head Tilt Test. Orbis Telemedicine, 2014. Web. 08 May 2015. <http://telemedicine.orbis.org/bins/content_page.asp?cid=735-2858-4397-2804-3110-3021-3037>.
- ↑ Wong AMF, Colpa L, Chandrakumar M. Ability of an Upright-Supine Test to Differentiate Skew Deviation From Other Vertical Strabismus Causes. Arch Ophthalmol. 2011;129(12):1570–1575. doi:10.1001/archophthalmol.2011.335
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 8.14 8.15 8.16 Arnoldi, Kyle. Orthoptic Evaluation and Treatment. Pediatric Ophthalmology: Current Thought and Practical Guide. By M. Edward. Wilson, Richard A. Saunders, and Rupal H. Trivedi. Berlin: Springer-Verlag, 2009. P.113-40.
- ↑ 9.0 9.1 9.2 Wright, Kenneth W. Pediatric Ophthalmology and Strabismus. St. Louis, MO: Mosby, 1995. P.159-157
- ↑ 10.0 10.1 Arnoldi K, Reynolds JD: “Unmasking Bilateral Inferior Rectus Restriction in Thyroid Eye Diasese: Using Degree of Cyclotropia. Am Orthopt J 2015; 65: 81-86