SMILE Lenticule Implantation
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
SMILE Background
Small incision lenticule extraction (SMILE) uses a femtosecond laser to create a lenticule within the stroma of the cornea which is then manually removed through a small peripheral incision to correct myopia and myopic astigmatism[1]. Additional information on SMILE can be found at https://eyewiki.aao.org/Small_Incision_Lenticule_Extraction_(SMILE).
Experimental use of the extracted lenticule has been described as an allogenic corneal inlay. This article discusses potential uses of SMILE lenticule implantation as an allogenic corneal inlay.
SMILE Procedure Steps
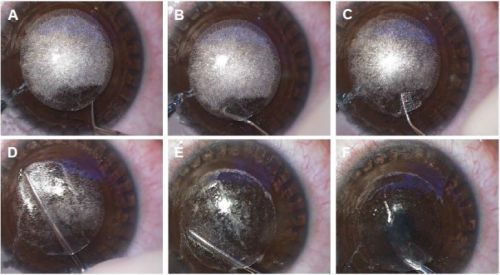
A brief overview of the SMILE procedure steps are included. The surgery is performed with the patient under topical anesthesia. The use of a femtosecond laser forms an intrastromal lenticule with a small incision. The lower interface is first formed, and then the upper interface, which is known as the cap. A tunnel incision of 2-3 mm is created which connects this cap interface with the corneal surface ([3]). The excision of the lenticule is then performed through blunt separation of the anterior and posterior surfaces, followed by removal with retinal micro-forceps or a lenticule stripper instrument ([2][4]). Prior to starting the procedure, the surgeon selects for certain factors, including refractive correction and the diameter and minimum thickness of the lenticule. This ensures the lower and upper interfaces can more easily be separated, leading to higher probability of successful lenticule extraction ([3]).
Complications
Complications of SMILE include corneal epithelial defects, tearing or perforation of the incision, loss of suction with the laser, creation of a bubble layer or black spots, and lenticule remnants within the corneal stroma. After the procedure, corneal haze, ocular inflammation, and delayed recovery of the patient’s vision can occur.[5]
The SMILE Lenticule
Composition
The SMILE lenticule consists of corneal stroma. Within the stroma exists type I collagen, packed into closely arranged fibrils, which then form a greater lamellae unit. Some authors posit that the lack of epithelium and endothelium in the SMILE lenticule reduces the risk of a significant host immune response following implantation of the lenticule.[6]
Lenticule Preservation
Cryopreservation, which involves storing the tissue in cryopreservans at -80 degrees Celsius is the most popular method of lenticule storage, allowing for preserved collagen fibril structure and integrity. Necrotic and apoptotic cells have been found in both fresh and cryopreserved lenticules. However, enough keratocytes are viable within the cryopreserved lenticules to allow for a regular stromal collagen architecture. This allows for maintenance of corneal transparency, thus promoting the lenticule’s role in use for implantation.[7] Unfortunately, the clinical application of the cryopreservation method is limited by its high costs and complexity. Other storage methods include hypothermia, room temperature preservation with glycerol, and use of decellularized lenticules (which are then stored in a medium with room temperature preservation). These were found to be safe and also maintained collagen structure.[6] However, more research is needed to further establish optimal storage conditions and agents specific to the intended use of the lenticule, as well as a generalized framework under which regulation and oversight could be instituted.[8][9]
Applications of SMILE Lenticule Implantation
Presbyopia
Correction of presbyopia is one potential use of implantation of the SMILE lenticule. In one study, LASIK was performed in eyes that underwent autologous lenticule implantation after SMILE. Each refractive procedure created a myopic target, with LASIK aiming for 1D less of myopia, establishing a theoretical monovision between eyes. No difference was seen in corneal tissue response between corneas that had undergone SMILE, lenticule implantation, and then LASIK, versus eyes that only underwent LASIK. This scenario may be useful for treatment of presbyopia. By restoring stromal volume and increasing corneal thickness in patients who are status post refractive surgery and have now developed presbyopia, they are afforded the opportunity to undergo a secondary refractive procedure for creation of a presbyopic monovision. It is unknown whether the SMILE lenticule yields superior results compared to current corneal inlay therapies offered to patients.[10]
Hyperopia

Small amounts of hyperopia may be treated with refractive surgery. Although SMILE is not FDA-approved to treat hyperopia, primate studies show that lenticule implantation can change refractive power to correct hyperopia.[12]. This has been reported in isolated human cases[13] but remains experimental. Small-incision lenticule intrastromal keratoplasty (sLIKE), has been proposed as a novel procedure for patients with moderate to high amounts of hyperopia, but remains to be studied.[11]
Keratoconus
Lenticule implantation in eyes with keratoconus has been reported to improve visual acuity and decrease keratometry.[14][15][16]
Corneal Ulcers, Thinning, and Perforations
A case has been reported where a thrice-recurrent pterygium was successfully treated using lenticule implantation in a patient with critical corneal thinning.[17]
Conclusion
The stromal lenticule procured from SMILE procedures may have clinical benefits in a variety of refractive and corneal conditions, but further research is needed before clinical implementation.
Additional Resources
- Afshari N, Fukuoka H, Harvey J. Small Incision Lenticule Extraction (SMILE). American Academy of Ophthalmology. EyeWiki. https://eyewiki.aao.org/Small_Incision_Lenticule_Extraction_(SMILE). Accessed October 15, 2023.
- Turbert D. What Is Small Incision Lenticule Extraction? American Academy of Ophthalmology. Eye Health A-Z. https://www.aao.org/eye-health/treatments/small-incision-lenticule-extraction-smile. Accessed October 15, 2023.
- Manche E, Valerio G. Step-by-Step SMILE Surgery. American Academy of Ophthalmology. Clinical and Surgical Videos. https://www.aao.org/education/clinical-video/step-by-step-smile-surgery-2. Accessed October 15, 2023.
References
- ↑ Moshirfar, M., McCaughey, M. V., Reinstein, D. Z., Shah, R., Santiago-Caban, L., & Fenzl, C. R. (2015). Small-incision lenticule extraction. Journal of cataract and refractive surgery, 41(3), 652–665. https://doi.org/10.1016/j.jcrs.2015.02.006
- ↑ Jump up to: 2.0 2.1 Titiyal JS, Kaur M, Shaikh F, Gagrani M, Brar AS, Rathi A. Small incision lenticule extraction (SMILE) techniques: patient selection and perspectives. Clin Ophthalmol. 2018;12:1685-1699. Published 2018 Sep 5. doi:10.2147/OPTH.S157172
- ↑ Jump up to: 3.0 3.1 Reinstein DZ, Archer TJ, Gobbe M. Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye Vis (Lond). 2014;1:3. doi:10.1186/s40662-014-0003-1
- ↑ Liu YC, Pujara T, Mehta JS. New Instruments for Lenticule Extraction in Small Incision Lenticule Extraction (SMILE). Bhattacharya S, ed. PLoS ONE. 2014;9(12):e113774. doi:10.1371/journal.pone.0113774
- ↑ Moshirfar M, Tukan AN, Bundogji N, et al. Ectasia After Corneal Refractive Surgery: A Systematic Review. Ophthalmol Ther. 2021;10(4):753-776. doi:10.1007/s40123-021-00383-w
- ↑ Jump up to: 6.0 6.1 Nemcokova M, Dite J, Klimesova YM, Netukova M, Studeny P. Preservation of corneal stromal lenticule: review. Cell Tissue Bank. 2022;23(4):627-639. doi:10.1007/s10561-021-09990-0
- ↑ Mohamed-Noriega K, Toh KP, Poh R, et al. Cornea lenticule viability and structural integrity after refractive lenticule extraction (ReLEx) and cryopreservation. Mol Vis. 2011;17:3437-3449.
- ↑ Zhang H, Deng Y, Li Z, Tang J. Update of Research Progress on Small Incision Lenticule Extraction (SMILE) Lenticule Reuse. Clin Ophthalmol. 2023;17:1423-1431. Published 2023 May 22. doi:10.2147/OPTH.S409014
- ↑ Riau AK, Liu YC, Yam GHF, Mehta JS. Stromal keratophakia: Corneal inlay implantation. Prog Retin Eye Res. 2020;75:100780. doi:10.1016/j.preteyeres.2019.100780
- ↑ Tomita M, Kanamori T, Waring GO 4th, et al. Simultaneous corneal inlay implantation and laser in situ keratomileusis for presbyopia in patients with hyperopia, myopia, or emmetropia: six-month results. J Cataract Refract Surg. 2012;38(3):495-506. doi:10.1016/j.jcrs.2011.10.033
- ↑ Jump up to: 11.0 11.1 Moshirfar M, Shah TJ, Masud M, et al. A Modified Small-Incision Lenticule Intrastromal Keratoplasty (sLIKE) for the Correction of High Hyperopia: A Description of a New Surgical Technique and Comparison to Lenticule Intrastromal Keratoplasty (LIKE). Med Hypothesis Discov Innov Ophthalmol. 2018;7(2):48-56.
- ↑ Williams GP, Wu B, Liu YC, et al. Hyperopic refractive correction by LASIK, SMILE or lenticule reimplantation in a non-human primate model. PLoS One. 2018;13(3):e0194209. Published 2018 Mar 28. doi:10.1371/journal.pone.0194209
- ↑ Pradhan KR, Reinstein DZ, Carp GI, Archer TJ, Gobbe M, Gurung R. Femtosecond laser-assisted keyhole endokeratophakia: correction of hyperopia by implantation of an allogeneic lenticule obtained by SMILE from a myopic donor [published correction appears in J Refract Surg. 2015 Jan;31(1):60] [published correction appears in J Refract Surg. 2015 Jan;31(1):60]. J Refract Surg. 2013;29(11):777-782. doi:10.3928/1081597X-20131021-07
- ↑ Doroodgar F, Jabbarvand M, Niazi S, et al. Customized Stromal Lenticule Implantation for Keratoconus. J Refract Surg. 2020;36(12):786-794. doi:10.3928/1081597X-20201005-01
- ↑ Mastropasqua L, Nubile M, Salgari N, Mastropasqua R. Femtosecond Laser-Assisted Stromal Lenticule Addition Keratoplasty for the Treatment of Advanced Keratoconus: A Preliminary Study. J Refract Surg. 2018;34(1):36-44. doi:10.3928/1081597X-20171004-04
- ↑ Almodin et. al. Femtosecond laser–assisted intrastromal corneal lenticule implantation for treatment of advanced keratoconus in a child’s eye. J Cataract Refract Surg. 2018;6(2):25-29. https://doi.org/10.1016/j.jcro.2018.01.004
- ↑ Pant OP, Hao JL, Zhou DD, Wang F, Lu CW. A novel case using femtosecond laser-acquired lenticule for recurrent pterygium: case report and literature review. J Int Med Res. 2018;46(6):2474-2480. doi:10.1177/0300060518765303

