Role of Intrastromal Injections in Fungal Keratitis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Treatment of fungal ulcers is one of the most challenging tasks in treating corneal infections. The incidence of fungal keratitis is higher in developing countries as compared to developed countries, with Aspergillus being the most common species isolated worldwide. Fungal ulcers typically involve the deep stroma, and topical medications are larger molecules that have poor stromal penetration. Therefore, direct drug delivery system in the form of intrastromal injections are helpful in the management of these deep recalcitrant fungal ulcers. Commonly used antifungal drugs for intrastromal injections include voriconazole, amphotericin B , fluconazole and natamycin.
Antifungal Drugs
The various antifungal drugs used in cases of fungal keratitis fall in the following categories
- Polyenes
- Large polyenes - Nystatin, amphotericin B
- Small polyenes - Natamycin
- Azoles
- Imidazoles - Miconazole, ketoconazole, clotrimazole
- Triazoles - Fluconazole, itraconazole, voriconazole, posaconazole
- Pyrimidines - Flucytosine
Polyenes
This class of antifungal agents includes amphotericin B, nystatin and natamycin . Nystatin has not been used to treat eye infections for several decades due to its low tissue penetration, toxicity, and reports of resistance. Amphotericin B and natamycin have been used intrastromally in the management of recalcitrant fungal keratitis.
Azoles
Azoles act on fungal cytochrome P450 enzymes by blocking the synthesis of ergosterol in the plasma membrane, thus inhibiting fungal growth. Azoles are divided into two major classes - imidazoles were the first to be introduced, followed by triazoles. Both have similar antifungal spectra, but triazoles have the advantages of being metabolized more slowly and exerting less influence on the metabolism of steroids in humans . These drugs are metabolized primarily in the liver, therefore control of liver enzymes is recommended. They have teratogenic activity (class C) and should not be used during pregnancy. The imidazoles used more often include miconazole ,econazole and ketoconazole. Among the first-generation triazoles, the most commonly used are itraconazole and fluconazole. Second-generation triazoles were introduced into clinical practice in the past decade and include voriconazole and posaconazole.
Pyrimidine
Pyrimidines are represented by 5-fluorocytosine (5-FC) or flucytosine, which is the only antifungal agent with intracellular action. After being absorbed by the fungus it is converted into 5-fluorouracil which is a powerful antimetabolite and acts by inhibiting the synthesis of DNA. Its use in eye infections is restricted due to its narrow antifungal spectrum and low penetration into ocular tissues.
Commonly used Intrastromal Antifungal Drugs
Amphotericin B
AMB belongs to the family of polyene macrolide antibiotics and was the first broad-spectrum antifungal agent to be discovered. Isolated in the 1950s, AMB is produced by the actinomycete Streptomyces nodosus and became popular after approval by the FDA in the 1960s due to its great efficiency in controlling disseminated fungal infections.[1]
Mechanism of action
AMB acts by increasing cell permeability through the formation of pores in the fungal cell membrane by binding to ergosterol and by promoting oxidative action on cells, thus altering their metabolic functions.
Pharmacokinetics
Amphotericin derives its name from its amphoteric properties and is effective in both extremes of acidic and basic Ph. It has low water solubility and needs to be diluted in deoxycholate for administration. It is photo- and thermosensitive and should be stored in a dark and refrigerated place (2-8°C).[1][2]
Antifungal spectrum
AMB acts on both yeasts and filamentous fungi. It has an excellent spectrum, being effective against Candida., Aspergillus sp, Penicillium marneffei and to a lesser extent, against Fusarium species.[1]
Intrastromal injections of amphotericin B in humans have not shown any toxicity. However, in animal models concentration of amphotericin B above 20ug/0.1 ml caused corneal edema, epithelial erosions and neovascularization.[3]
Voriconazole
Mechanism of Action
Voriconazole acts by inhibiting the synthesis of ergosterol and is much more effective than 1st generation triazoles.
Antifungal spectrum
Effective in the treatment of keratitis by Candida, Aspergillus, Fusarium, Scedosporium and Paecilomyces[4][5]
Its advantages compared to polyenes include its greater stability to light and temperature, remaining effective for up to 30 days.[6][7]
Preparation of intrastromal drug concentration
Intrastromal dose of Amphotericin B is 5-10ug/0.1 ml.
Preparation of intrastromal Amphotericin B is done by reconstituting 50mg powder of Amphotericin B in 10ml dextrose 5% to give concentration of 5mg/ml and 500 ug/0.1ml. Further this concentration is diluted with 9.9 ml dextrose 5% in a tuberculin syringe to give concentration of 500ug/10 ml and 50ug/ml and 5 ug/0.1 ml.
The dose of Intrastromal Voriconazole is 50 ug/ 0.1 ml and is prepared by adding 19 ml distilled water in 200 mg powder of voriconzole to get 20 ml drug (10mg in 1 ml). 1 ml of drug is taken and 9 ml distilled water is added to get 10 mg in 10 ml . .05 ml of this solution contains 50 ug or 0.1 ml of this solution contains 100 ug.
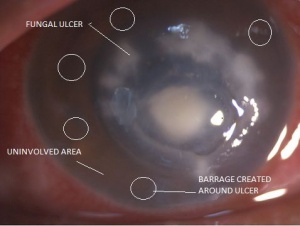
Technique of giving intrastromal injections
Intrastromal injections can be given under topical or peribulbar anesthesia. Under full aseptic conditions, the preloaded drug should be administered under an operating microscope. The bevel down, the needle is inserted obliquely from the uninvolved area to just reach the abscess at mid-stromal level which is the intended area of drug deposition . The drug then is injected and the amount of hydration of the cornea is used as a guide to assess the area covered. Once the desired amount of hydration is achieved, the plunger is withdrawn slightly to ensure discontinuation of the capillary column and thus prevent back-leakage of the drug. Five divided doses are given around the abscess to form a deposit of the drug around the circumference of the lesion. This is done in a way that a centripetally directed progressive wave of fluid appears to encompass the abscess along each meridian. Circumferential injection will ensure the formation of a barrage of intrastromal drug around the entire abscess.[8] Most studies show that at least 2 more injections must be given to obtain an optimal response. [9]
Advantages
- Direct drug delivery.
- Overcomes the problem of poor penetration of drugs .
- Intrastromal drug acts like a depot causing slow release of drug.
- Less epithelial toxicity
Clinical Studies
Several small studies have evaluated the use of intrastromal voriconazole for patients not responsive to topical medications. One study looked at 25 patients not responding to topical Natamycin and Voriconazole. 72% of these patients responded to intrastromal injections of Voriconazole and 15% of these patients needed more than one injection.[10] Of those patients non responsive, the majority were culture positive for Fusarium. Another study looked at 12 patients, of which 10 resolved after injections. Of the two failures, one was positive for Aspergillus and the other Fusarium.[8] An additional study evaluated 20 patients, of which 14 responded to injections.[11] This cohor required an average of 2.65 injections. In these studies, the patients who did not respond required tectonic keratoplasty.
Thus, intrastomal injections are safe and effective way for the treatment of deep and recalcitrant fungal ulcers. The number and interval of injections still needs further evaluation.
References
- ↑ Jump up to: 1.0 1.1 1.2 Bennett J. Agentes antimicrobianos, agentes antifúngicos. In: Brunton L, editor. Goodman & Gilman: as bases farmacológicas da terapêutica.
- ↑ Oliveira PR, Resende SM, Oliveira FC, Oliveira AC. Ceratite fúngica. Arq Bras Oftalmol. 2001;64(1):75-9.
- ↑ Qu L, Li L, Xie H. Curr Eye Res. 2014 Apr;39(4):340-7.
- ↑ Anderson KL, Mitra S, Salouti R, Pham TA, Taylor HR. Fungal keratitis caused by Paecilomyces lilacinus associated with a retained intracorneal hair. Cornea. 2004;23(5):516-21.
- ↑ Bunya VY, Hammersmith KM, Rapuano CJ, Ayres BD, Cohen EJ. Topical and oral voriconazole in the treatment of fungal keratitis. Am J Ophthalmol. 2007;143(1):151-3.
- ↑ 6 Al-Badriyeh D, Neoh CF, Stewart K, Kong DC. Clinical utility of voriconazole eye drops in ophthalmic fungal keratitis. ClinOphthalmol. 2010;4:391-405.
- ↑ Dupuis A, Tournier N, Le Moal G, Venisse N. Preparation and stability of voriconazole eye drop solution. Antimicrob Agents Chemother. 2009;53(2):798-9.
- ↑ Jump up to: 8.0 8.1 Sharma N, Agarwal P, Sinha R, Titiyal J.S., VelpandianT, Vajpayee R, Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: case series Br J Ophthalmol 2011;95:1735-1737 doi:10.1136
- ↑ Maniam A, Yuen GS.Intrastromal antifungal injection as a successful modality of treatment for fungal keratitis: a case series. Int J Res Med Sci 2019;7:288-93.
- ↑ Kalaiselvi G, Narayana S, Krishnan T, et al. Intrastromal voriconazole for deep recalcitrant fungal keratitis: a case series. British Journal of Ophthalmology 2015;99:195-198.
- ↑ Konar P, Joshi S, Mandhare SJ, Thakur R, Deshpande M, Dayal A. Intrastromal voriconazole: An adjuvant approach for recalcitrant mycotic keratitis. Indian J Ophthalmol 2020;68:35-8