Palinopsia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Palinopsia is the persistence or recurrence of an image after the visual stimulus has been removed [1].
Disease Entity
Disease & Epidemiology
Palinopsia refers to a pathological group of visual symptoms in which there is an abnormal persistence or recurrence of an image in time. Palinopsia derives its name from the Greek word palin which means "again" and opsia which means "seeing.”
Palinopsia is distinct from a physiological after-image, which is a benign, normal response in which an image briefly persists after a person has stopped looking at the original visual stimulus. Images from palinopsia are longer-lasting and more intense than physiological after-images. Whereas physiological after-images appear immediately after removal of the original visual stimulus, palinopsia after-images may appear immediately or after a time interval. Images from palinopsia are positive images, or the same colors as the original visual stimulus, whereas physiological after-images are negative images, or complementary colors of the original visual stimulus [1].
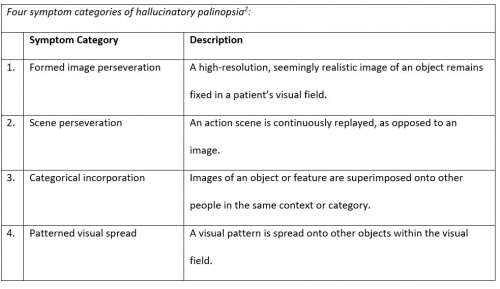
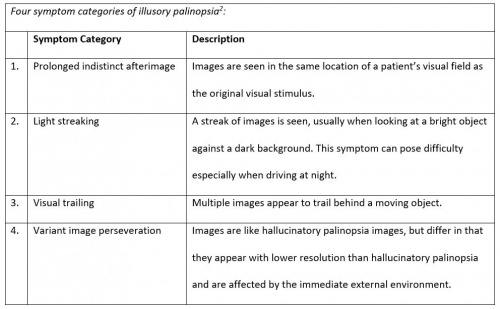
Palinopsia can be categorized into two general categories: hallucinatory palinopsia and illusory palinopsia [2]. Individuals with hallucinatory palinopsia see images that are long-lasting, high-resolution, and occur anywhere within the visual field. Individuals with illusory palinopsia see images that are affected by immediate environmental factors, such as light and motion. The images from illusory palinopsia are short-lasting, low-resolution and indistinct.
There is limited data on the epidemiology of palinopsia. Palinopsia may occur in up to 10% of migraineurs and seem to occur more frequently in migraine with aura than without aura [3]. Although migraines occur more frequently in females than males and more frequently in younger to middle aged populations than elderly populations [4], there have not been significant studies done comparing palinopsia between the categories.
Etiology
Hallucinatory palinopsia is associated with a dysfunction of visual memory. It can be caused by posterior cortical lesions or seizures [5]. Examples of lesions that may cause hallucinatory palinopsia are neoplasms, infarctions, hemorrhages, arteriovenous malformations, aneurysm, abscesses, and tuberculomas. The seizures that cause palinopsia are associated with metabolic imbalances, such as hyperglycemia, carnitine deficiency, ion channel disturbances, and Creutzfeldt-Jakob disease [6].
Illusory palinopsia is associated with alterations in visual perception of a real external stimulus affected by immediate environmental factors. Illusory palinopsia can be caused by changes in neurotransmitter receptors associated with migraines [7], hallucinogen persisting perception disorder (HPPD) [8], trauma to the head, or drugs or other medications. Medications that have been reported to cause illusory palinopsia include trazodone [9], nefazodone, mirtazapine [10], topiramate, clomiphene, oral contraceptives, and risperidone. Palinopsia may also be idiopathic.
Risk Factors
Given that palinopsia has a wide range of etiologies, both genetics and environmental factors may play roles in risk for palinopsia.
Pathophysiology
Hallucinatory palinopsia results from a dysfunction in visual memory. It is thought to occur from localized cortical hyperexcitability or heightened activity in the posterior visual pathway through the mechanisms of cortical deafferentation, focal cortical irritation, and epileptic discharges.
Illusory palinopsia results from a dysfunction in visual perception. It is thought to occur from changes in the excitability of neurons in the visual pathways. Drugs that cause palinopsia (trazodone, nefazodone, risperidone, and mirtazapine) are similar in sharing antagonism at the 5-HT2 receptor which binds the neurotransmitter serotonin, and the hallucinogen LSD is an agonist for 5-HT2A and 5-HT2C. It is therefore proposed that 5-HT2 receptor excitotoxicity may be involved in the mechanism of illusory palinopsia [11]. Illusory palinopsia after-images are affected by environmental light and motion, which indicates changes in neuronal excitability for both pathways.
Primary prevention
There have not been significant studies done on the primary prevention of palinopsia, as palinopsia is a symptom indicating disease rather than a disease itself.
Diagnosis
The diagnosis of palinopsia is made clinically. There are no diagnostic tests or examination findings.
History
A clinical history can help determine whether a patient has hallucinatory or illusory palinopsia, and is especially useful for diagnosing illusory palinopsia. A clinical history can also help identify the cause of a patients palinopsia, and aid in the planning of appropriate treatment. Asking patients about their history of seizure would also help determine the underlying cause of a patient’s hallucinatory palinopsia, as hallucinatory palinopsia is usually caused by seizures or posterior cortical lesions. It is important to distinguish palinopsia from psychiatric-mediated medical conditions. Questions to ask the patient include insight, delusional construct and auditory hallucinations to help differentiate palinopsia from underlying psychiatric conditions.
Symptoms & Signs
Individuals with palinopsia usually have associated symptoms as well, such as photopsias, dysmetropsia, visual snow, oscillopsia, entoptic phenomena, and cerebral polyopia.
Hallucinatory palinopsia resembles a complex visual hallucination of an image or scene previously seen by a person. Hallucinatory images may last from minutes to hours. Hallucinatory palinopsia images or scenes may be seen immediately after the original stimulus, or there may be a delay in time before they are perceived [12] (Table 1).
Illusory palinopsia refers to the distortion of a real external stimulus that has not yet been removed. There may be distortions in the shape, color, or size of the image. The perceived image will also remain in the same location in the visual field. Unlike hallucinatory palinopsia, illusory palinopsia images are influenced by immediate environmental factors, such as background contrast, stimulus intensity, and ambient lighting [2]. Illusory palinopsia images are seen immediately after the original stimulus (Table 2).
Physical examination
Physical exams usually come up negative and are non-contributory towards the diagnosis of illusory palinopsia.
Clinical diagnosis
Although palinopsia can be indicative of serious diseases that need treatment, many cases are benign and idiopathic. Hallucinatory palinopsia is less common and usually indicative of more severe diseases than illusory palinopsia. Images and scenes perceived by patients with hallucinatory palinopsia also usually deal greater stress to patients than illusory palinopsia.
Diagnostic procedures
To determine patient whether a patient has hallucinatory or illusory palinopsia, a full ophthalmologic and neurologic history and physical exam should be done. Automated visual field testing and neuroimaging should be performed. These procedures are warranted for hallucinatory palinopsia for its common cause by seizures and posterior cortical lesions. They may also be useful for illusory palinopsia for its common cause by migraines. More often however, epileptiform discharges are usually not seen in EEGs for patients with illusory palinopsia, or palinopsia without structural correlate [2]. Neuroimaging is therefore more useful for patients with hallucinatory palinopsia.
Hallucinatory palinopsia can indicate serious neurological disease, and therefore a patient who reports experience of even one episode of hallucinatory palinopsia should be referred to a neuro-ophthalmologist or neurologist. An MRI should be offered to patients with hallucinatory palinopsia.
Laboratory test
If the neuroimaging is unremarkable for a patient with hallucinatory palinopsia, then directed additional evaluation may be considered.
Differential diagnosis
The differential diagnosis of palinopsia includes toxins (such as illicit hallucinogens and prescribed medication), metabolic conditions (such as hyperglycemia), psychiatric conditions (such as schizophrenia or psychotic depression), and structural cerebral lesions.
Management
General treatment
For hallucinatory palinopsia, treatment of the underlying cause usually resolves the palinopsia [13]. For hallucinatory palinopsia caused by from seizures, treatment of the seizures usually resolves the palinopsia. Hallucinatory palinopsia caused by lesions is directed by treatment of the type of lesion.
For illusory palinopsia, treatment can involve medications that decrease the excitability of neurons, such as clonidine, gabapentin, acetazolamide, magnesium, or calcium channel blockers [2]. However, more studies need to be done on the efficacy of these drugs as they vary from reported cases. Sunglasses or other tinted lenses may also alleviate symptoms of illusory palinopsia. For illusory palinopsia caused by migraines, treatment of the migraine would also be appropriate.
References
- ↑ 1.0 1.1 Bender MB, Feldman M, Sobin AJ. Palinopsia. Brain. 1968;91(2):321–38.
- ↑ 2.0 2.1 2.2 2.3 Gersztenkorn D, Lee AG. Palinopsia revamped: A systematic review of the literature. Survey of ophthalmology. 2014;60:1–35.
- ↑ Belcastro V, Cupini LM, Corbelli I, Pieroni A, D’Amore C, Coproni S, Gorgone G, Ferlazzo E, Palma FD, Sarchielli P, Calabresi P. Palinopsia in patients with migraine: A case-control study. Cephalalgia. 2011;31:999.
- ↑ Younger DS. Epidemiology of Migraine. Neurol Clin. 2016;34:849–861.
- ↑ Auzou P, Ozsancak C, Miret N, Hitzel A, Hannequin D. Palinopsia associated with partial seizures secondary to right parietal hemorrhage. Ann Med Interne (Paris). 1998;149(3),161-163.
- ↑ Purvin V, Bonnin J, Goodman J. Palinopsia as a presenting manifestation of Creutzfeldt–Jakob disease. Journal of clinical neuro-ophthalmology. 1989;9(4):242–6.
- ↑ Belcastro V, Cupini LM, Corbelli I, Pieroni A, D'Amore C, Caproni S, Calabresi P. Palinopsia in patients with migraine: a case-control study. Cephalalgia. 2011;231(9), 999-1004.
- ↑ Kawasaki A, Purvin V. Persistent palinopsia following ingestion of lysergic acid diethylamide (LSD). Arch Ophthalmol. 1996;114(1):47-50.
- ↑ Hughes MS, Lessell S. Trazodone-induced palinopsia. Arch Ophtalmol. 1990;108:399-400.
- ↑ Ihde-Scholl T, Jefferson JW. Mitrazapine-associated palinopsia. The Journal of Clinical Psychiatry. 2001;62(5):373.
- ↑ Lauterbach EC, Abdelhamid A, Annandale JB. Posthallucinogen-like visual illusions (palinopsia) with risperidone in a patient without previous hallucinogen exposure: possible relation to serotonin 5-HT2A blockade. Pharmacopsychiatry 2000;33:38-41.
- ↑ Kinsbourne M, Warrington E. A study of visual perseveration. J Neurol Neurosurg Psychiatry. 1963;26:468-475.
- ↑ Khan AN, Sharma R, Khalid S, McKean D, Armstrong R, Kennard C. Palinopsia from a posteriorly placed glioma – an insight into its possible causes. BMJ Case Reports. 2011.