Ocular Amyloidosis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Amyloidosis is a diverse, heterogeneous group of disorders characterized by the deposition of hyaline extracellular material into various tissues throughout the body including the eye and ocular adnexa. Ocular Amyloidosis has been reported in almost every part of the eye as well as adnexal and orbital tissues. Although amyloidosis may be suspected clinically, classic histopathological charcteristics can be identified on tissue biopsy for definitive diagnosis. In recent years, concentration has been directed towards standardization of nomenclature given the proliferation of amyloidosis type-specific treatment regimens.
Disease Entity
International Classification of Disease (ICD)
- ICD-9-CM 277.3 Amyloidosis
- ICD-9-CM 277.39 Other Amyloidosis (including inherited systemic amyloidosis, secondary amyloidosis)
- ICD-10-CM E85 Amyloidosis
- ICD-10-CM E85.8 Other Amyloidosis
History
Mathias Schleiden, a German botanist, first used the term “amyloid” in 1838 in his description of plant histology. Shortly thereafter, Virchow began contemporary medical use of this term in neuroanatomy as well as described its diffuse and characteristic extracellular tissue protein deposits observed by light microscopy in liver autopsies.[1] Congo Red dye was first described by Benhold in 1922, with its pathognomonic birefringence described by Divry in 1927.[2] A description of its fibril proteins followed in 1971 by Cohen and Calkins.[3]
Definition
Amyloidosis is a diverse, heterogeneous group of disorders characterized by the deposition of hyaline extracellular material into various tissues throughout the body including the eye and ocular adnexa.[4] The amyloid proteins are deposited as insoluble fibrils as a consequence of abnormal protein folding,[1] detected on electron microscopy as nonbranching, rigid, and mostly extracellular. Binding of the Congo Red dye in addition to the “apple green” birefringence on polarized light microscopy are diagnostic.[1]
Ocular involvement of amyloidosis has been reported in multiple compartments, including the adnexa, extraocular muscles, levator palpebrae muscle, conjunctiva, cornea, lens and capsule, anterior uvea and trabecular meshwork, as well as vitreous and retina.
Nomenclature
Definition and classification of the set of diseases included in amyloidosis continues to be refined. The International Society of Amyloidosis has released several revised nomenclature recommendations as recently as 2010 and 2012.
Historical guidelines promoted a classification system based on clinical presentation and consisted of four primary subtypes:[5]
- Primary localized amyloidosis (most common)
- Primary systemic amyloidosis
- Secondary localized amyloidosis
- Secondary systemic amyloidosis
While this naming system is still occasionally used, with advances in protein sequence analysis, recent guidelines recommend greater classification based on the specific precursor (A-) of each individual amyloid protein (abbreviated).[1][5][6][7] For example, transthyretin amyloidosis is described as ATTR amyloidosis, with specific mutations being further designated, e.g. ATTRV30M.5 According to the official 2012 guidelines, mutations are named “according to the substitution or deletion in the mature protein,”[1] meaning that ATTRV30M describes the most common transthyretin amyloidotic variant protein with a substitution of methionine for valine at residue 30.[2]
Standardization of nomenclature is of critical importance given continually evolving amyloidosis type-specific treatment regimens.[5][8] Nomenclature guidelines are reviewed biennially by the International Society of Amyloidosis and are published in Amyloid, the official journal of the International Society of Amyloidosis. The 2012 guidelines describe 30 distinct human and 10 animal fibril proteins.[1] To be included on this list, a protein “must have been unambiguously characterized by protein analysis,” and “described in a peer review journal.”
Diagnosis
Systemic amyloidosis is frequently diagnosed by family history and physical exam.
Diagnosis of ocular amyloidosis includes careful history taking, family history, systemic physical exam, slit lamp biomicroscopy, indirect biomicroscopy, and, sometimes, orbital imaging and tissue biopsy. Definitive diagnosis of any ocular lesion requires confirmational biopsy and specific histological examination.
Physical Examination
Many ocular signs and symptoms can be caused by amyloidosis including lid malpositions, globe displacement, abnormal motility, diplopia, ptosis, recurrent subconjunctival hemorrhage, conjunctival mass, corneal opacity, increased intraocular pressure (IOP), vitreous opacities/floaters, and abnormal fundus appearance.
Initial patient presentation of ocular amyloidosis may be a mass lesion of unknown origin. These mass lesions can resemble or occur secondary to malignant processes. A case series performed by Aryasit et al. demonstrated that a mass lesion was the presenting feature in 5 out of 6 patients (83.3%).[9] Therefore, these lesions should be followed and likely warrant a biopsy for pathologic diagnosis.
Systemic Amyloidosis
Symptoms of nephrotic-range proteinuria (nondiabetic), cardiomyopathy (no ischemic history), hepatomegaly (no contrast dye filling defect by imaging) and/or peripheral neuropathy (nondiabetic) should prompt an investigation for extraocular amyloidosis.[10] Diagnosis can be narrowed and confirmed with a combination of additional tests including but not limited to urine/serum examination for monoclonal proteins, subcutaneous fat aspirate, bone marrow biopsy, rectal biopsy, 2D Doppler echocardiography, electrocardiography and skeletal survey.[9][10]
Histological Diagnostic Procedures
Biopsy with histological examination is diagnostic. Common staining characteristics listed below are described in the Basic and Clinical Science Course, Section 8: Cornea and External Disease:[3]
- Positive staining with Congo Red dye (link)
- Dichroism (link) and birefringence (link) (Often described as “apple-green”)
- Metachromasia with crystal violet dye
- Fluorescence in ultraviolet light with thioflavine T stain
- Typical filamentous appearance by electron microscopy
Orbit and Extraocular muscles
Orbital amyloidosis is frequently benign, localized, and associated with primary disease.[9][11][12][13] Lacrimal gland involvement can be unilateral or bilateral.[13]Signs and symptoms commonly involve mass/tissue infiltration, ptosis, diplopia, irritation and epiphoria and can mimic other orbital masses and diseases leading to delayed diagnosis.[11][12][14][15][16]
Amyloid deposits in the levator palpebrae muscle commonly presents with ptosis and may precede other orbital or conjunctival signs for several years.[14]
Isolated extraocular muscle involvement is highly variable with symptoms of combined proptosis (unilateral or bilateral), diplopia, or restrictive ophthalmoplegia.[12][15] A study of 24 patients with extraocular muscle involvement had evidence of extraocular muscle enlargement based on CT interpretation.[11]
Optic neuropathy (compressive or infiltrative) is uncommon but has been reported with documented visual field loss.[17]
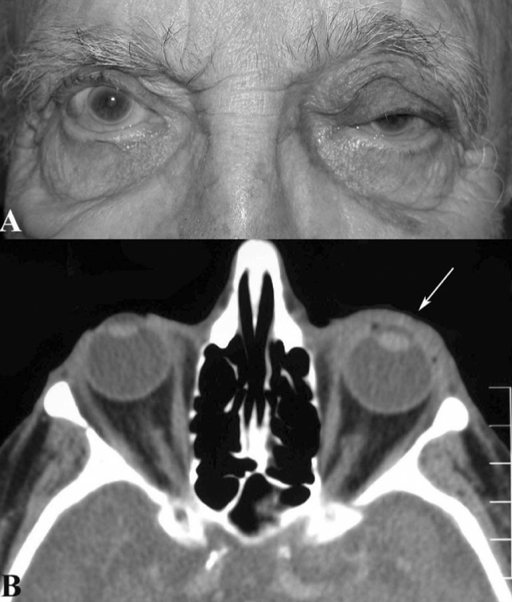
Figure 1: Orbital amyloidosis
Diffuse infiltration by amyloidosis seen throughout patient’s left anterior orbit (white arrow) without any posterior orbital involvement. (Reprinted from Periocular and Orbital Amyloidosis: Clinical Characteristics, Management, and Outcome. Ophthalmology 2006;113:1657-64 with permission from Elsevier.)[11]
Conjunctiva
A review of conjunctival specimens sent for pathological examination by Grossniklaus and colleagues showed only 5 of 2,455 (0.002%) specimens were positive for amyloidosis.[18] Conjunctival amyloidosis most commonly presents as a primary, localized process,[3] although in some cases may represent systemic amyloidosis.[19]
Clinical presentation occurs as a mass. A case series of 6 patients by DeMirci and colleagues showed a circumscribed lesion in two patients (33%) and a diffuse lesion in four patients (67%).[19] Another report of 50 patients included 44 (88%) that were localized, nonsystemic conjunctival amyloidosis.[19] Secondary, localized conjunctival amyloidosis has been reported after blunt ocular trauma.[20]
Gross examination commonly reveals a yellowish, “waxy” lesion described as “confluent fusiform lesions or polypoidal papules.”[19]
Diagnosis is typically confirmed by excisional biopsy for circumscribed lesions and incisional biopsy for diffuse lesions.
Figure 2: Conjunctival amyloidosis.
Smooth, waxy, yellow, relatively circumscribed masses are seen at bilateral medial canthi. Visualization of the lesions is improved with lateral gaze. (Image courtesy of Gary S. Lissner, MD)
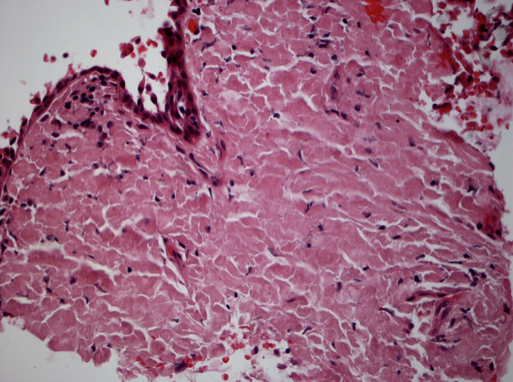
Figure 3: Conjunctival amyloidosis.
Same patient in Figure 2, showing hematoxylin and eosin stain of conjunctival tissue biopsy. Extensive hyalinization and diffuse eosinophilic extracellular material consistent with amyloidosis. (Image courtesy of Paul J. Bryar, MD)
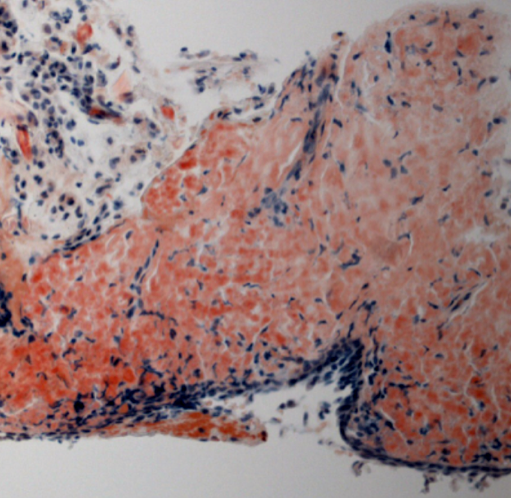
Figure 4: Conjunctival amyloidosis: Congo Red stain.
Same patient as in Figures 2 and 3, showing conjunctiva with acellular eosinophilic deposits in the stroma. The deposits stain with Congo Red and are birefringent. (Image courtesy of Paul J. Bryar, MD)
Cornea
Corneal amyloidosis is demonstrated in several of the corneal dystrophies.[3]
Gelatinous droplike corneal dystrophy (subepithelial amyloidosis) is characterized by subepithelial and anterior stromal amyloid deposition demonstrated by either light or transmission electron microscopy.[3]
Stromal corneal dystrophies involving amyloid proteins include type I and III lattice corneal dystrophy, lattice corneal dystrophy, gelsolin type II (Meretoja syndrome), granular corneal dystrophy type II (granular-lattice dystrophy, Avellino corneal dystrophy).
Keratoconjunctival amyloid deposition has been reported following blunt trauma, described as midstromal lattice-like lines in the superonasal cornea adjacent to a yellow-pink conjunctival infiltrate.[20]
Iris/Trabecular Meshwork/Lens/Glaucoma
Published reports of ocular amyloidosis include involvement of the iris and pupillary margin, trabecular meshwork, and the anterior surface of the lens.[21][22][23][24]Involvement of the trabecular meshwork and/or uvea may present as rubeotic glaucoma with elevated IOP reported as high as 42 mmHg.[24] Pathogenesis is thought to involve amyloid protein in the aqueous humor that clogs vs. directly infiltrates the trabecular meshwork.[21][22]
Incidence of secondary glaucoma in amyloidotic subtypes has been reported from 17% (Val30Met) to 100% (Ser50Ile, Val30Met, Arg104His).[24] Amyloid involvement of the aqueous humor can resemble anterior uveitis, suggesting a role for aqueous tap and analysis prior to initiating topical steroids.[23]
Retina/Vitreous
Vitreous amyloidosis is classically described as “initially granular with wispy fringes,” growing in size and aggregating to form a “glass wool appearance.”[25] It is frequently visually significant, differentiating it from more common non-hemorrhagic vitreous opacities such as asteroid hyalosis. Deposits are bilateral in most cases, although can be asymmetric or unilateral.[26] Focal arteriolar sheathing may occur in the absence of vitreous involvement,[27] however most cases show an initial retinal tuft adjacent to retinal vessels followed by secondary vitreous involvement.[25] Within the retina, histopathology shows amyloid deposition within the retinal arteriolar walls and “among the photoreceptor inner and outer segments.”[26] In transthyretin-related familial amyloidotic polyneuropathy, the retinal pigment epithelium (RPE), along with the liver, synthesizes mutant amyloidogenic transthyretin protein making the RPE a potential target for treating cases of ocular amyloidosis.[27] Vitreous involvement is most often seen in systemic amyloidosis, although isolated disease has been reported.[24][26][28][29]
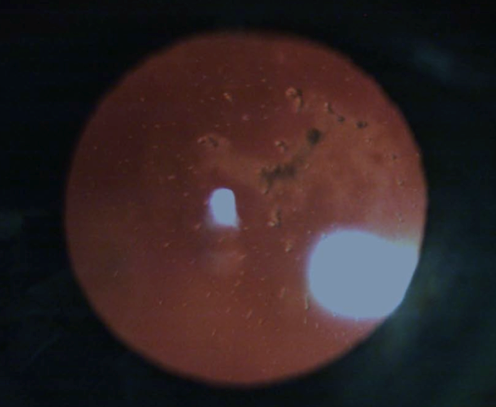
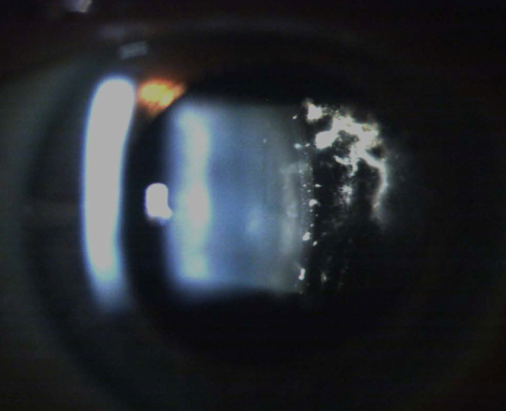
Figure 5: Vitreous amyloidosis.
Retrolenticular vitreous amyloidosis, showing amyloid footplates on posterior lens capsule. (Image courtesy of Anh-Danh Phan, MD)
Figure 6: Vitreous amyloidosis.
Same patient as in Figure 5, showing “glass wool” appearance of retrolenticular vitreous amyloidosis. (Image courtesy of Anh-Danh Phan, MD)
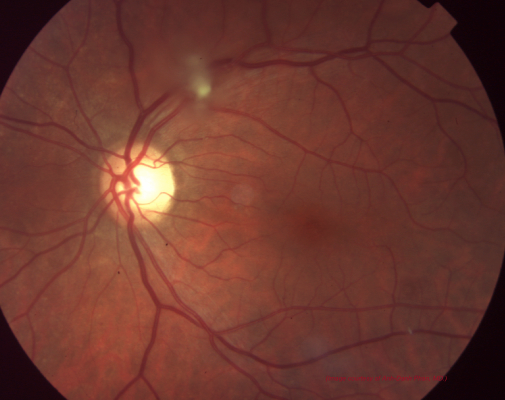
Figure 7: Retinal/Vitreous amyloidosis.
Tuft of vitreous amyloidosis emanating from retina and overlying superior vascular arcade seen in same patient as Figures 5 and 6.(Image courtesy of Anh-Danh Phan, MD)
Differential Diagnosis
- Neoplastic – Lymphoma (most common due to appearance on conjunctiva), leukemia, amelanotic melanoma, sebaceous cell carcinoma, squamous cell carcinoma, Kaposi’s sarcoma, metastases
- Inflammatory – Sarcoidosis, Pyogenic granuloma
- Infectious – Papilloma
- Other – Cholesterolosis, asteroid hyalosis, chronic dehemoglobinized vitreous hemorrhage
Treatment
Management options for ocular amyloidosis vary depending on patient symptoms and visual significance of amyloid protein deposition.
Extraocular (orbital) amyloidosis is rare. A recent case report of two patients noted biopsy-proven amyloid lacrimal gland involvement.[13] Excision can be attempted, however complete excision of the lacrimal gland can be surgically challenging. There is no conclusive evidence in the literature to recommend complete surgical excision vs. biopsy and observation.
Conjunctival lesions are often conservatively managed with observation or lubrication with artificial tears or gels. If recalcitrant, local excision or surgical debulking may be performed. Demirci et al. reported only a 27% recurrence rate after surgical debulking.[19] A recent article by Fraunfelder enumerated the benefits of liquid nitrogen cryotherapy for conjunctival amyloidosis.[30] The mechanism of action for cryotherapy is speculated to involve induced ischemia of the amyloidotic conjunctiva secondary to damage to small blood vessels. In this report, none of the four study patients demonstrated any systemic signs of amyloidosis. Three of the patients underwent surgical debulking prior to liquid nitrogen cryotherapy, which was applied at the base of the surgical excision site. All participants had relatively good initial symptomatic results; however, two showed recurrence of conjunctival amyloid mass lesions that were subsequently treated with additional adjunctive cryotherapy. Although reports of cryotherapy for conjunctival amyloidosis demonstrate it to be a safe and relatively effective therapeutic option, further study is warranted.
Treatment of increased IOP from amyloid-related secondary glaucoma can be challenging even with maximal topical therapy. Previous studies have demonstrated that IOP may be lowered to satisfactory levels by trabeculectomy,[24] however the effect may be temporary with resultant increases in pressure after several months. Dry eye, friable amyloidotic conjunctiva, angle closure, and diffuse infiltration of the trabecular meshwork by amyloid have been proposed to contribute to postoperative bleb failure and unsatisfactory IOP.[22][31] Tube shunts have been suggested as another treatment for amyloidosis related secondary glaucoma,[22] however they have not yet been reported in the literature. In recalcitrant cases after trabeculectomy, cyclophotocoagulation can be used to further lower IOP to tolerable levels.
Vitreous opacities are often visually significant, particularly in transthyretin-related amyloidosis.[27][32][33] Recent literature suggests that ocular complications from transthyretin-related amyloidosis can be worsened following liver transplantation.[34] Primary treatment for removal of amyloid vitreous opacities is pars plana vitrectomy, demonstrating consistent improvement in visual acuity and patient symptoms with few complications.[35][36] Recurrence, although uncommon, can become visually significant requiring repeat vitrectomy with particular attention to removal of the retrolenticular and cortical vitreous.[26] A recent report by Beirão and colleagues suggests recurrences can be avoided by performing primary complete, extensive vitrectomy with scleral depression, concluding that incomplete vitreous removal is a predictive factor for symptom recurrence.[37]
Based on the theory that the RPE is responsible for production of amyloidogenic transthyretin, panretinal photocoagulation (PRP) is being investigated as a possible therapy for recurrence of vitreous amyloidosis deposits. An initial report of two patients demonstrated a decrease in both vitreous and retinal amyloid deposits in the PRP-treated eyes without significant complications.[27]
Treatment of systemic amyloidosis should be based on the specific amyloidosis mutation type. Therapy may be targeted at the infectious or inflammatory causes in secondary amyloidosis, at the bone marrow production and plasma cell dyscrasia in primary amyloidosis, or disease specific alterations in dialysis in patients with renal involvement. Hereditary forms of amyloidosis may require liver transplantation to stop the production of mutant amyloid, however this may worsen the ocular amyloidosis.
A number of investigative and novel therapies are currently being designed. These include tafamidis, a small molecule stabilizer of the transthyretin tetramer, which is currently being used in Europe to slow the progression of neuropathy.[38] Other agents have been designed to interfere with fibril formation, inhibit amyloid precursors, and enhance degradation of existing amyloid deposits. IV infusions of siRNA formulations have shown in phase 1 trials to reduce both mutant and non-mutant transthyretin.[39] Additionally, new antisense oligonucleotides targeting hepatic production of mutant transthyretin have shown exciting results suppressing mRNA and serum TTR levels by as much as 80% in a transgenic mouse model.[8] These agents offer a promising future for potential treatments of amyloidosis.
Additional Resources
- International Society of Amyloidosis (ISA): http://www.amyloidosis.nl/
- Amyloid Official Journal of the ISA: http://informahealthcare.com/amy
- Amyloidosis Center at Boston University School of Medicine: http://www.bu.edu/amyloid/
- Amyloidosis Center at Mayo Clinic: http://www.mayoclinic.com/health/amyloidosis/DS00431
- Amyloidosis Research Foundation: http://www.amyloidosisresearchfoundation.org/
- Amyloidosis Support Groups: http://www.amyloidosissupport.com/
- Registry of Mutations of Amyloidosis Proteins: http://amyloidosismutations.com/
- European Amyloidosis Research Consortium (EURAMY): http://www.euramy.org/
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Sipe JD, Benson MD, Buxbaum JN, et al. Amyloid fibril protein nomenclature: 2012 recommendations from the Nomenclature Committee of the International Society of Amyloidosis. Amyloid 2012;19:167–170.
- ↑ 2.0 2.1 Picken MM, Dogan A, Herrera GA eds. Amyloid and Related Disorders: Surgical Pathology and Clinical Correlations. Humana Press; 2012.
- ↑ 3.0 3.1 3.2 3.3 3.4 AAO. Basic and Clinical Science Course: External Disease and Cornea. 2012–2013 ed. American Academy of Ophthalmology
- ↑ Westermark P, Benson MD, Buxbaum JN, et al. Amyloid fibril protein nomenclature -- 2002. Amyloid 2002;9:197–200.
- ↑ 5.0 5.1 5.2 Anon. Nomenclature of amyloid and amyloidosis. WHO-IUIS Nomenclature Sub-Committee. Bull World Health Organ 1993;71:105–12.
- ↑ Sipe JD, Benson MD, Buxbaum JN, et al. Amyloid fibril protein nomenclature: 2010 recommendations from the nomenclature committee of the International Society of Amyloidosis. Amyloid 2010;17:101–4.
- ↑ Westermark P, Benson MD, Buxbaum JN, et al. A primer of amyloid nomenclature. Amyloid 2007;14:179–83.
- ↑ 8.0 8.1 Benson MD, Kluve-Beckerman B, Zeldenrust SR, et al. Targeted suppression of an amyloidogenic transthyretin with antisense oligonucleotides. Muscle Nerve 2006;33:609–18.
- ↑ 9.0 9.1 9.2 Aryasit O, Preechawai P, Kayasut K. Clinical presentation, treatment, and prognosis of periocular and orbital amyloidosis in a university-based referral center. Clin Ophthalmol 2013;7:801–5.
- ↑ 10.0 10.1 Gertz M, Lacy M, Dispenzieri A. Amyloidosis. Hematol Oncol Clin North Am 1999;13:1211–33, ix.
- ↑ 11.0 11.1 11.2 11.3 Leibovitch I, Selva D, Goldberg R a, et al. Periocular and orbital amyloidosis: clinical characteristics, management, and outcome. Ophthalmology 2006;113:1657–64.
- ↑ 12.0 12.1 12.2 Erie J, Garrity J, Norman M. Orbital amyloidosis involving the extraocular muscles. Arch Ophthalmol 1989;107:1428–9.
- ↑ 13.0 13.1 13.2 Ghazi NG, Bowman AM, Shields MD. Bilateral lacrimal system involvement by sclerosing extramedullary hematopoietic tumor. Ophthal Plast Reconstr Surg 2006;22:296–8.
- ↑ 14.0 14.1 Dithmar S, Linke RP, Kolling G, et al. Ptosis from localized A-lambda-amyloid deposits in the levator palpebrae muscle. Ophthalmology 2004;111:1043–7.
- ↑ 15.0 15.1 Lett KS, Shah A, Gottlob I. External ophthalmoplegia as the presenting feature of systemic amyloidosis. Strabismus 2007;15:153–6.
- ↑ Hill VE, Brownstein S, Jordan DR. Ptosis secondary to amyloidosis of the tarsal conjunctiva and tarsus. Am J Ophthalmol 1997;123:852–4.
- ↑ Finlay K, Rootman J, Dimmick J. Optic neuropathy in primary orbital amyloidosis. Can J Ophthalmol 1980;15:189–92.
- ↑ Grossniklaus H, Green W, Luckenbach M, Chan C. Conjunctival lesions in adults. A clinical and histopathologic review. Cornea 1987;6:78–116.
- ↑ 19.0 19.1 19.2 19.3 19.4 Demirci H, Shields CL, Eagle RC, Shields J a. Conjunctival amyloidosis: report of six cases and review of the literature. Surv Ophthalmol 2006;51:419–33.
- ↑ 20.0 20.1 Khalifa YM, Bloomer MM, Margolis TP. Secondary localized sectoral keratoconjunctival amyloidosis from ocular trauma. Cornea 2010;29:1328–9.
- ↑ 21.0 21.1 Mansour AM, Hidayat AA, Gorevic PD. Case Report Isolated amyloidosis of anterior uvea and trabecular meshwork. 2000:393–394.
- ↑ 22.0 22.1 22.2 22.3 Nelson G, Edward D, Wilensky J. Ocular amyloidosis and secondary glaucoma. Ophthalmology 1999;106:1363–6.
- ↑ 23.0 23.1 Dunlop AA, Graham SL. Familial amyloidotic polyneuropathy presenting with rubeotic glaucoma. Clin Experiment Ophthalmol 2002;30:300–2.
- ↑ 24.0 24.1 24.2 24.3 24.4 Kimura A, Ando E, Fukushima M, et al. Secondary glaucoma in patients with familial amyloidotic polyneuropathy. Arch Ophthalmol 2003;121:351–6.
- ↑ 25.0 25.1 AAO. Basic and Clinical Science Course: Retina and Vitreous. 2012–2013 ed. American Academy of Ophthalmology
- ↑ 26.0 26.1 26.2 26.3 Ciulla T, Tolentino F, Morrow JF, Dryja T. Vitreous amyloidosis in familial amyloidotic polyneuropathy. Report of a case with the Val30Met transthyretin mutation. Surv Ophthalmol 1995;40:197–206.
- ↑ 27.0 27.1 27.2 27.3 Kawaji T, Ando Y, Hara R, Tanihara H. Novel therapy for transthyretin-related ocular amyloidosis: a pilot study of retinal laser photocoagulation. Ophthalmology 2010;117:552–5.
- ↑ Kawaji T, Ando Y, Ando E, et al. A case of vitreous amyloidosis without systemic symptoms in familial amyloidotic polyneuropathy. Amyloid 2004;11:257–259.
- ↑ Salvador F, Mateo C, Alegre J, et al. Vitreous amyloidosis without systemic or familial involvement. Int Ophthalmol 17:355–7.
- ↑ Fraunfelder FW. Liquid nitrogen cryotherapy for conjunctival amyloidosis. Arch Ophthalmol 2009;127:645–8.
- ↑ Miyahara T, Ohta K, Yamamoto Y. 25-gauge Vitrectomy to Treat Ocular Complications of. 2007;16:169–170.
- ↑ Cavallaro T, Martone RL, Dwork AJ, et al. The retinal pigment epithelium is the unique site of transthyretin synthesis in the rat eye. Invest Ophthalmol Vis Sci 1990;31:497–501.
- ↑ Kawaji T, Ando Y, Nakamura M, et al. Transthyretin synthesis in rabbit ciliary pigment epithelium. Exp Eye Res 2005;81:306–12.
- ↑ Ando Y, Ando E, Tanaka Y, et al. De novo amyloid synthesis in ocular tissue in familial amyloidotic polyneuropathy after liver transplantation. Transplantation 1996;62:1037–8.
- ↑ Sandgren O, Stenkula S, Dedorsson I. Vitreous surgery in patients with primary neuropathic amyloidosis. Acta Ophthalmol 1985;63:383–8.
- ↑ Monteiro J, Martins A, Figueira A, et al. Ocular changes in familial amyloidotic polyneuropathy with dense vitreous opacities. Eye (Lond) 1991;5 ( Pt 1):99–105.
- ↑ Beirão NM, Matos E, Beirão I, et al. Recurrence of vitreous amyloidosis and need of surgical reintervention in Portuguese patients with familial amyloidosis ATTR V30M. Retina 31:1373–7.
- ↑ Gorevic P. Overview of amyloidosis. UpToDate 2013. Accessed December 23rd, 2013.
- ↑ Coelho T, Adams D, Silva A, et al. Safety and efficacy of RNAi therapy for transthyretin amyloidosis. N Engl J Med 2013;369:819–29.