Medial Spindle Procedure
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
A medial spindle procedure addresses involutional medial ectropion with punctal eversion through a diamond shaped excision of the medial conjunctiva and eyelid retractors followed by re-insertion. This is often used as an adjunct to other horizontal tightening procedures to achieve stabilization of the lower eyelid with improved punctal inversion.
Surgical Procedure
| CPT Code | Name of Procedure |
|---|---|
| 67917 | Correction of everted punctum and ectropion repair |
Background
Historical Perspective
The medial spindle procedure, first described in 1985 by Nowinski and Anderson, is used to correct involutional ectropion of the lower eyelid caused by medial laxity involving the punctum.[1] The term ectropion, derived from the greek etymology of ektrepein (ex- out, trepein- to turn) is characterized by horizontal laxity resulting in an outward turning of the eyelid, most often seen on the lower lid. Poor eyelid to globe apposition can cause exposure keratopathy because of poor lubrication of conjunctiva and corneal surface leading to irritation, with subsequent risk of corneal abrasion, exposure keratopathy, infectious keratitis, corneal thinning to perforation, and corneal scarring. [2]
When the punctum is involved, patients will also experience epiphora due to improper drainage. Further, repair of lower lid ectropion using a lateral canthal tendon tightening procedure without addressing medial canthal laxity can lateralize the punctum resulting in chronic epiphora. To prevent permanent damage to conjunctiva and vision loss, repair of a symptomatic medial ectropion is recommended.
Types of Ectropion
Ectropion can be classified into congenital, involutional, paralytic, cicatricial and mechanical. Surgical options for each type of ectropion is typically a customized combination that is very patient-specific. The following is primarily aimed for lid malpositions of the lower eyelid.
Involutional Ectropion
Involutional ectropion occurs due to horizontal laxity of the lower eyelid and disinsertion of the lower eyelid retractors.
Risk Factors
- Age (decreased elasticity in the skin, gravitational forces)
- Mechanical pressure on the eyelids through pulling or rubbing of eyes (allergies, contact lens, behavioral)
- Floppy eyelid syndrome - sleep apnea with CPAP machine use, and trauma
Goal of Intervention
- Lower eyelid laxity - horizontal tightening achieved through a lateral tarsal strip procedure
- Lower eyelid retractor disinsertion - re-attach the lower eyelid retractors to the tarsus (Jones procedure)
- Punctal ectropion - re-appose the punctum to the bulbar conjunctiva through the medial spindle procedure
Surgical Option
- Medial spindle procedure
- Lateral tarsal strip
- Jones procedure
Cicatricial Ectropion
Cicatricial ectropion occurs from shortening of the anterior lamella (skin and orbicularis muscle) due to fibrosis from chronic inflammation, infection, trauma, burns, radiation, or postsurgical.
Risk Factors
- Burns
- Trauma
- Prior eyelid surgery
- Laser skin resurfacing
- Medical/skin condition affecting the eyelid skin (ex. Keloid)
Goal of Intervention
- Release scar bands from chronic inflammation or injury
- Extend area of the anterior lamella with a skin graft to improve mobility of the lid
- If tarsal support is needed for additional apposition of the lower eyelid, a cartilage graft can be used.
Surgical Options
- Full-thickness versus split thickness skin graft
- Cartilage graft for tarsal support (ear, hard palate, synthetic tissue)
- Z-plasty, S-plasty, and/or a W-plasty
Paralytic Ectropion
Paralytic ectropion occurs due to decreased orbicularis muscle tone due to facial nerve palsy (CN VII).
Risk Factors
- Stroke
- Infection
- Idiopathic
- Iatrogenic (ex. tumor debulking)
Goal of Intervention
- Decreased or absent eyelid closure - can be addressed with a horizontal tightening procedure, a lateral tarsorrhaphy to reduce the interpalpebral fissure distance
- Punctal eversion - re-appose with punctum to the conjunctiva for improved anatomical position for tear drainage
- Brow ptosis - depending on the form of ptosis (temporal versus temporal and medial) and presence of rhytids, a brow lift or a forehead lift can be performed.
Surgical Options
- Horizontal tightening with or without tarsorrhaphy,
- Correction of punctal ectropion
Mechanical Ectropion
Mechanical ectropion occurs from lesions or tumors that physically lower the eyelid or can occur from facial ptosis.
Risk Factors
- Tumorous growths of anterior lamella of lower eyelid
- Aging
Goal of intervention
- Mechanical descent of lower eyelid - excision of mass with reconstruction of defect.
- Facial ptosis - addressed with face lift with lid tightening procedure
Surgical Options
- Tumor excision
- Horizontal tightening with surgical elevation of the midface
Types of Intervention for Horizontal Ectropion
Horizontal ectropion can be fixed in three ways: lateral repair, medial repair, or a combination. A lateral approach is often performed as it is away from the lacrimal system, decreasing the risk of iatrogenic injury and subsequent complications. When the punctum is involved, a medial spindle procedure is used often in adjunct to a lateral canthal tightening. [3][4]
Surgical Goal
The goal of this procedure is to reverse the laxity of the lower lid to provide improved apposition of the eyelid to the globe. If there is reduced apposition, the corneal surface and conjunctiva develop exposure keratopathy which can result in decreased vision, tearing, photophobia, pain, injection, and an increased risk of infection. The medial spindle procedure, specifically, improves tear drainage by correcting the punctal malposition seen in these patients.[5]
Pre-operative Conditions
Indications
- Punctal eversion: the punctum is no longer in contact with tear lake
- Medial Involutional Ectropion without horizontal laxity: outward turning of the lower lid with palpebral conjunctival exposure without lower lid laxity
- Medial Involutional Ectropion with horizontal Laxity: outward turning of the lower lid with palpebral conjunctival exposure with lower lid laxity
- Cosmesis
Contraindications
This procedure is relatively safe. However, relative contraindications include active inflammation or infection in the eye which should be resolved to prevent post-operative progression and poor surgical outcome. Additionally, patients who cannot tolerate local or general anesthesia should not undergo this procedure. [6][7]
Preoperative Evaluation
Prior to surgical intervention, it is necessary to complete a comprehensive medical and social history, and a full ophthalmic examination. It is imperative to perform a thorough assessment of the etiology of the ectropion must be made in order to determine the correct combination of procedures to improve ectropion induced symptoms.
Review of Historical Conditions
Historical conditions need to be evaluated in a peri-operative setting to determine if surgical repair is the appropriate intervention for a patient’s ectropion. Bell’s palsy results from a cranial nerve VII palsy that can improve over the course of six months to one year. It is necessary to allow sufficient time for recovery prior to any permanent intervention. Similarly, traumatic injury to the facial nerve can result in transient loss of function that requires at least six months to one year to assess for improvement. Blepharospasm induced ectropion can be mitigated with Botox injections to weaken the contraction of the orbicularis oculis through chemodenervation and traditional lid-tightening procedures would not be beneficial. Obstructive sleep apnea has been associated with floppy eyelid syndrome and the lid laxity can result in ectropion. Intervention would need to address the excise the excess skin and re-approximate the eyelid with horizontal lid tightening.
Specialized Testing
Patients should be evaluated for lid laxity, lid malposition, lagophthalmos, lamellar shortening, midface ptosis, globe position, and lacrimal outflow abnormalities. Specialized testing includes:
- Schirmers test to determine severity of dryness should also be included in the exam.
- Assessment of lid laxity and punctal position:
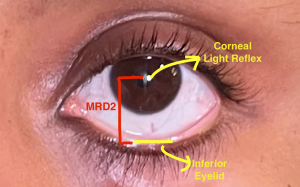
- Margin-to-Reflex Distance 2 (MRD2): First, determine the lower lid position by measuring an MRD2 (pupillary reflex to lower eyelid margin). If the MDR2 is greater than 5 mm, then lower lid retraction is present.
- The snapback test is performed by pulling the lower eyelid inferiorly and releasing to see how long it takes to return to normal position. If it takes >2 seconds, the test is considered positive for lower lid laxity.
- The distraction test is another way to determine the presence of lower lid laxity. This is performed by pinching the lower lid and pulling it away from the globe. If there is more than 5 mm distance measured, there is laxity present.
- To assess punctal movement, the eyelid is retracted laterally to demonstrate excessive movement. Displacement of the punctum >2mm is positive for punctal laxity and should be surgically improved. [7][8]
- To assess lacrimal system patency, a probe and irrigation of the upper and lower canalicular system can provide insight to any acquired complete nasolacrimal duct obstruction.
Medial Spindle Surgical Technique
- A corneal shield may be placed to protect the globe surface
- 1-2 mL of 2% Lidocaine with epinephrine is injected subcutaneously and subconjunctivally into the medial aspect of the lower eyelid
- A bowman probe is placed into the inferior canaliculus
- Using a toothed forceps, the conjunctiva is lifted and a diamond-shaped excision is made with Wescott scissors. A medial cut is made followed by a lateral cut to create the diamond shape.
- A double armed absorbable 5-0 or 6-0 suture is then used to pass through the lower eyelid retractors from the base to the superior conjunctival edge on either side.
- The needle is reverse mounted through the inferior conjunctival edge and then externalized through the skin at the junction of the eyelid and cheek skin.
- This aims to anchor the lower lid retractors and pull the punctum posteriorly against the globe.
- Perform lateral tarsal strip or other form of lateral cantonal tightening if required
- Tie sutures to invert punctum appropriately. Should be slightly over-inverted against the globe.
- Remove corneal shield
- Sutures may be removed 2 weeks later at follow up appointment
Complications
The medial spindle procedure has risks of bleeding, infection, swelling, and recurrence. Corneal abrasion, poor cosmesis, lacrimal defects, canthal dystopia, or retrobulbar hematoma can also occur. Patients can have allergic reactions to local anesthetic. Additional surgery may be required, and ectropion can be recalcitrant. [4][9]
Outcomes
A medial spindle procedure provides a surgical option for medial involution ectropion with punctal laxity and/or eversion. It can be used alone or as an adjunct with horizontal tightening procedures for ectropion repair. With minimal risks and recovery, this procedure should be considered if symptomatic ectropion with punctal laxity is present. This procedure provides cosmetic and symptomatic relief for ectropion and ectropion induced epiphora, exposure keratitis, and corneal scarring.
References
- ↑ Nowinski TS, Anderson RL. The Medial Spindle Procedure for Involutional Medial Ectropion. Arch Ophthalmol.1985;103(11):1750–1753. doi:10.1001/archopht.1985.01050110146045
- ↑ Barmettler, A. and Yen, M. (no date) Lower eyelid retraction, EyeWiki. Available at: https://eyewiki.org/Lower_Eyelid_Retraction#:~:text=Lower%20eyelid%20retraction%20may%20present,of%20eyelid%20or%20orbital%20surgery.
- ↑ AlHarthi AS. Involutional ectropion: etiological factors and therapeutic management. Int Ophthalmol. 2023 Mar;43(3):1013-1026. doi: 10.1007/s10792-022-02475-3. Epub 2022 Sep 2. PMID: 36053479.
- ↑ Jump up to: 4.0 4.1 4.2 Brodie, S. E. (2020). Oculofacial Plastic and Orbital Surgery Part II: Periocular Soft Tissues Chapter 12: Periocular Malpositions and Involutional Changes. In Basic and clinical science course. essay, American Academy of Opthalmology.
- ↑ Kam, K., Cole, C., Bunce, C. et al. The lateral tarsal strip in ectropion surgery: is it effective when performed in isolation?. Eye 26, 827–832 (2012). https://doi.org/10.1038/eye.2012.34
- ↑ Lee H, Park M, Chang M, Kang DW, Lee JS, Baek S. Clinical Characteristics and Effectiveness of the Lateral Tarsal Strip and Medial Spindle Procedure. Ann Plast Surg. 2015 Oct;75(4):365-9. doi: 10.1097/SAP.0000000000000145. PMID: 24691326.
- ↑ Jump up to: 7.0 7.1 Bergstrom R, Czyz CN. Ectropion Lower Eyelid Reconstruction. [Updated 2023 May 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470449/
- ↑ Skorin L Jr, Lange R. Ectropion: classification, diagnosis, and management. Consultant. 2018;58(6):e180.
- ↑ Themes, U. (2020, May 11). 6 lower eyelid ectropion. Plastic Surgery Key. https://plasticsurgerykey.com/6-lower-eyelid-ectropion/10.1055/b-0039-171449