Lower Eyelid Retraction
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Lower eyelid retraction is a malposition of the lower eyelid, where the lid margin is displaced inferiorly, resulting in increased exposure of the surface of the eye to the environment. This can present with dry eye symptoms and can lead to exposure keratitis, corneal ulcer, corneal scarring, and even corneal perforation. [1]
Lower eyelid retraction may present unilaterally or bilaterally, depending on the etiology. Though it most frequently presents due to thyroid eye disease, it can result due to extraocular muscle injury or surgery, facial nerve palsy, age-related loosening of tissues, or as a complication of eyelid or orbital surgery. [2] Treatment options depend on the severity and etiology of the retraction, with mild cases being managed with ocular surface lubrication and more severe cases with dermal filler or surgery. [2]
Anatomy
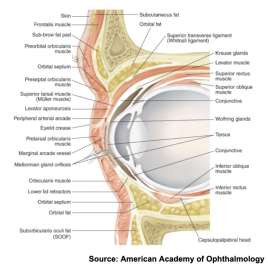
Anatomically, the lower eyelid can be divided into the anterior (skin and orbicularis oculi muscle), middle (orbital septum and orbital fat), and posterior lamellae (tarsus and conjunctiva) sections (See Figure 2). [2]
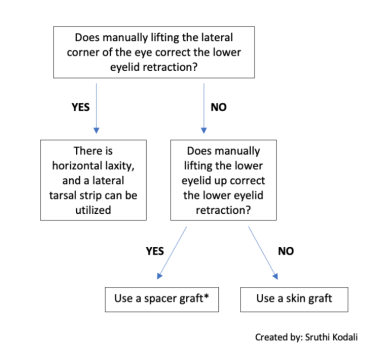
Lower eyelid retraction is due to a deficiency or scarring in one or more of the three lamellae. The location of the deficiency can influence treatment protocol, especially when the retraction is severe. For moderate to severe posterior lamella deficiency, spacer graft can be considered. For moderate to severe cases of anterior and middle lamellae deficiency, spacer grafts can be helpful, but mid-face lifts or skin grafts should also be considered (See “Clinical significance and management”).
Typically, the lower eyelid rests at the level of the inferior corneal limbus, which is the border between the lower cornea and the sclera. The position of the lower eyelid is determined by several factors, which include: horizontal lower eyelid laxity, disinsertion of the lower eyelid retractors, length and degree of tension in the lower eyelid skin or orbital septum, adequacy of the fornix and palpebral conjunctivae, location of the canthal ligament, degree of eyeball protrusion, and degree of orbicularis oculi tension. [2]
Clinical Exam
In lower eyelid retraction, the lower eyelid is inferior to the inferior corneal limbus. This can be measured in two ways. The first is called scleral show. Upon examination of the patient, the presence of visible sclera between the lower eyelid margin and inferior corneal limbus indicates retraction. The corneal limbus at 6 o’clock is typically covered or at the margin of the lower eyelid, so any amount of scleral visible between the two structures can be quantified and documented as a measurement of 'scleral show.'[4]
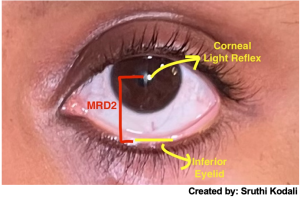
Another method to quantify lower eyelid retraction is the margin reflex distance 2 (MRD2). With the patient’s and examiner’s eyes at the same level, the patient is directed to look at a light held directly in front of them.The distance between the corneal light reflex to the central portion of the lower eyelid is measured in millimeters (See Figure 1). [5] The MRD2 is typically less than 5.5 mm, so any distance greater is indicative of lower eyelid retraction. [4]
Long standing, symmetric lower lid retraction is more likely to be physiologic. Comparison with old photographs can help to determine onset. On the other hand, asymmetric, new, or changing lower eyelid position needs to be evaluated.
Etiologies
Lower eyelid retraction most frequently presents due to thyroid eye disease associated with fibrosis of the capsulopalpebral fascia[2] (the lower lid analogy to the levator palpebrae in the upper lid). [6] This can be seen concomitantly with upper eyelid retraction. Aside from thyroid disease, there exist a multitude of etiologies for lower eyelid retraction. They can be classified through a modified system, first established by Dr. Bartley in 1995[7], into the four following categories: (1) Neurogenic, (2) Myogenic, (3) Mechanical, (4) Congenital.
Neurogenic |
|
Myogenic |
|
Mechanical |
|
Congenital |
Table 1. Etiologies of Lower Eyelid Retraction[11]
Clinical Significance and Management
Lower eyelid retraction often presents with dry eye symptoms, exposure keratopathy, and permanent corneal scarring due to corneal ulceration or even corneal perforation.[12]Thus, it is crucial to treat both the symptoms and underlying cause of the retraction.
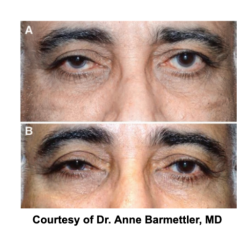
Retraction can first be managed with ocular lubricants, including artificial tears and ointments to temporarily treat the associated dry eye symptoms.[14] For a more permanent solution, a surgical approach is typically utilized. The following flow chart can be useful in determining which surgical approach to take for severe cases of lower eyelid retraction:
Summary
Lower eyelid retraction is a malposition of the lower eyelid that usually presents with dry eye symptoms and can lead to exposure keratopathy and long-term damage to the eye if not appropriately managed. Though most commonly results from thyroid eye disease and post-surgical scarring, there exist a plethora of underlying causes of the condition. Lower eyelid retraction can be managed initially by alleviating the dry eye symptoms and more permanently via surgery, depending upon the location of the defect and the severity.
- ↑ Taylor, D., Hoyt, C. S., & McLeod , S. D. (2005). Chapter 33. In Pediatric ophthalmology and strabismus. essay, Elsevier Saunders.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 Kim, K. H., Baek, J. S., Lee, S., Lee, J. H., Choi, H. S., Kim, S. J., & Jang, J. W. (2017). Causes and surgical outcomes of lower eyelid retraction. Korean Journal of Ophthalmology, 31(4), 290. https://doi.org/10.3341/kjo.2016.0059
- ↑ https://www.aao.org/image/eyelid-anatomy-6
- ↑ Jump up to: 4.0 4.1 Putterman , A. M. (2008). Chapter 3/ Evaluation of the Cosmetic Oculoplastic Surgery Patient . In Putterman's Cosmetic Oculoplastic Surgery (pp. 21–30 ). essay.
- ↑ Putterman AM. Margin reflex distance (MRD) 1, 2, and 3. Ophthal Plast Reconstr Surg. 2012;28(4):308-11.
- ↑ Holland, E. J., Mannis, M. J., & Lee, W. B. (2013). Chapter 2: Eyelid Anatomy and Function . In Ocular surface disease cornea, conjunctiva and tear film (pp. 11–15). essay, Elsevier Saunders.
- ↑ Bartley, G. B. (1996). The differential diagnosis and classification of eyelid retraction. Ophthalmology, 103(1), 168–176. https://doi.org/10.1016/s0161-6420(96)30744-6
- ↑ Thyroid eye disease. EyeWiki. (2021, July 10). Retrieved December 18, 2021, from https://eyewiki.aao.org/Thyroid_Eye_Disease#Diagnostic_procedures
- ↑ Sung, M. S., Lee, M. J., Choung, H.-K., Kim, N. J., & Khwarg, S. I. (2010). Lower eyelid Epiblepharon associated with lower eyelid retraction. Korean Journal of Ophthalmology, 24(1), 4. https://doi.org/10.3341/kjo.2010.24.1.4
- ↑ Richardson, D. R., Gadzala, L. A., Bonsall, D. J., Hogg, J. P., Williams, H. J., & Nguyen, J. (2017). Congenital Paradoxical Lower Eyelid Retraction With Upgaze due to an Anomalous Extraocular Muscle. Ophthalmic plastic and reconstructive surgery, 33(4), e101–e102. https://doi.org/10.1097/IOP.0000000000000809
- ↑ Nelson, E. R. (n.d.). Eyelid Retraction . Eyelid Retraction - American Academy of Ophthalmology. Retrieved December 18, 2021, from https://www.aao.org/oculoplastics-center/eyelid-retraction
- ↑ Krachmer, J., Mannis, M. J. & Holland, E. J. Cornea. Third edn, Vol. 1 (Mosby, 2011)
- ↑ Barmettler, Anne & Heo, Moonseong. (2018). A Prospective, Randomized Comparison of Lower Eyelid Retraction Repair With Autologous Auricular Cartilage, Bovine Acellular Dermal Matrix (Surgimend), and Porcine Acellular Dermal Matrix (Enduragen) Spacer Grafts. Ophthalmic Plastic & Reconstructive Surgery, 34, 266-273. https://doi.org/10.1097/IOP.0000000000000946
- ↑ Patipa, M. (2000). The evaluation and management of lower eyelid retraction following cosmetic surgery. Plastic & Reconstructive Surgery, 106(2), 438–453. https://doi.org/10.1097/00006534-200008000-00033