Light-Near Dissociation
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Entity
Light-Near dissociation
Description
Light-near dissociation (LND) is a pupillary sign that occurs when the pupillary light reaction is impaired while the near reaction (accommodative response) remains intact. LND can occur unilaterally or bilaterally.[1] This is clinically significant, because since the efferent pathway is shared for both reactions, there are limited mechanisms for the dissociation of the two pathways. The afferent pathway is more commonly affected (disrupting the light response) as a cause of LND but the efferent pathway can also be affected in a lesion of the ciliary ganglion or postganglionic nerve with subsequent aberrant regeneration. This article will discuss the causes and implications of LND.
Etiology
LND may result from a lesion in the afferent pupillary pathway (e.g., retinal ganglion cells, optic nerve, chiasm, tract, lateral geniculate body), a pretectal lesion (e.g. dorsal midbrain syndrome, Argyll-Robertson pupil, pineal tumor, Wernicke’s encephalopathy), or a lesion in the efferent pathway (e.g., ciliary ganglion, post-ganglionic nerve) with subsequent aberrant regeneration.[2]
Risk Factors
Risk factors for LND are determined by the etiology of the lesion.
Anatomy and localization
Unilateral LND
The lesion could be in either afferent pathway, or it could be in the ciliary body or post-ganglionic nerve. If it is in the afferent pathway, the light reaction will be poor, but the near reaction will be spared, because it enters the Edinger-Westphal nucleus in the brainstem ventrally and then proceeds down the efferent pathway with no dependence on the afferent pathway. In general, unilateral or bilateral but asymmetric afferent lesions produce a relative afferent pupillary defect (RAPD). Bilateral and symmetric afferent defects involving the pupil pathway may not demonstrate an RAPD and LND may be the best demonstration of the bilateral afferent defect. If the lesion is in the efferent pathway, in general both the light and near reactions will be poor at the time of initial injury to the nerve. However, if the postganglionic nerve that previously innervated the iris regenerates aberrantly to the ciliary body, the light reaction will remain poor, but the near reaction would recover, creating an efferent pathway LND.[3]
Bilateral LND
The lesion could either be caused by a bilateral afferent pathway lesion or a lesion of the dorsal midbrain (e.g., pineal tumor, Parinaud syndrome). If it is a bilateral afferent lesion, both light reactions will be poor with a preserved near reaction. If the lesion is in the dorsal midbrain damaging the pre-tectal nuclei, the light reaction will also be poor bilaterally. These lesions will not affect the near pathway, because it enters the Edinger-Westphal more ventrally.[3]
Diagnosis
Physical examination
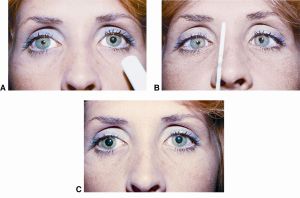
An adequate pupillary exam must be performed in the light and in the dark. If the light reaction is poor in one or both eyes, but the near reaction is intact, the patient has unilateral or bilateral light-near dissociation, respectively. In other words, the pupil(s) do not constrict in response to light, but they do constrict with accommodation.
Diagnostic workup
Assessment of LND is focused on localizing the lesion, if possible, to distinguish central, more sinister causes (e.g., dorsal midbrain syndrome) from benign causes (e.g. Adie’s tonic pupil). Syphilis serology is generally recommended for bilateral simultaneous tonic pupils or the Argyll Robertson pupil (small pupils which are regular which accommodate but do not react to light). The first step is to determine the laterality, as central causes are more likely to be bilateral. If it is unilateral, the next step is to ensure it is not a third nerve palsy with pupillary involvement by examining for ptosis and motility. If a third nerve palsy is suspected or the LND is bilateral, the patient could be imaged to look for central lesions and screened for syphilis.[1][3] If this is not the case, looking for sector paresis with vermiform movement of the iris helps diagnostically, indicative of Adie’s tonic pupil.[1] The presumptive diagnosis of Adie’s tonic pupil can be supported by testing pharmacologically with 0.1% pilocarpine which will only cause an eye to constrict in the context of denervation super-sensitivity.
Prognosis
The patient’s prognosis depends on the etiology of the LND.
Additional resources
Video description of this entity by Dr Andrew Lee [1]
A video example by JA Moran Eye Institute is available [2]
References
- ↑ Jump up to: 1.0 1.1 1.2 Thompson S. Light-Near Dissociation of the Pupil. Ophthalmologica [Internet]. 1984 [cited 2019 Jul 16];189(1–2):21–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6472802
- ↑ Lee AG, Brazis PW. Clinical pathways in neuro-ophthalmology : an evidence-based approach. Thieme; 2003. 486 p. page 434.
- ↑ Jump up to: 3.0 3.1 3.2 Shams PN, Bremner FD, Smith SE, Plant GT, Matthews TD. Unilateral Light-Near Dissociation in Lesions of the Rostral Midbrain. Arch Ophthalmol [Internet]. 2010 Nov 1 [cited 2019 Jul 16];128(11):1486. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21060053

