Laser Vitreolysis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Laser Vitreolysis is a medical procedure that involves the application of nanosecond pulses of laser to evaporate and dissect the vitreous opacities.
Vitreous opacities, also known as floaters, are among the most common ocular conditions. In some patients, symptoms of floaters can adversely affect the quality of life, interfere with reading or driving, and may persist for a long time.[1][2] A study by Wagle and coworkers addressed the impairment of vision quality associated with floaters in 311 outpatients. This study demonstrates that floaters have as much influence on the quality of life as other ocular and systemic diseases. The utility values of floaters were equal to age-related macular degeneration, and similar to glaucoma, mild angina, stroke, and asymptomatic HIV.[1] A study by Webb and coworkers demonstrated that floaters are common in the general population, irrespective of age, race, gender, and eye color.[3] In a review of 603 smartphone users, 76% (n=458) indicated that they notice floaters, with 199 of these individuals citing noticeable vision impairment as a result of their floaters. Myopes and hyperopes were 3.5 and 4.4 times, respectively, more likely to report moderate or severe floaters. [3] A study by Garcia and coworkers showed that there was a 52.5% reduction in contrast sensitivity function following posterior vitreous detachment.[4]
Three management options exist for symptomatic floaters: patient education and observation, pars plana vitrectomy, and laser vitreolysis. The most common advice to patients by ophthalmologists is “try to ignore them” and “learn to live with them”. Twenty-three-gauge vitrectomy can be successful, but it is an invasive procedure and most retinal specialists are reluctant to accept this procedure for floaters due to potential risks, including retinal tears and detachments, proliferative vitreoretinopathy, choroidal bleeding, macular shrinkage, and cataract progression.[5] [6][7][8][9]
YAG (yttrium-aluminum-garnet, 1064 nm) laser vitreolysis has been performed with variable success since the 1980s. These conditions included vitreoretinal tractions due to proliferative diabetic retinopathy, sickle cell retinopathy, vitreous cysts, and rhegmatogenous retinal detachment.[5] The first report of YAG laser vitreolysis for floaters was published in 1993.[10] In that study, Tsai and collaborators used the YAG laser to treat 15 patients with localized prepapillary or central vitreal opacities. All patients were satisfied with the treatment and stated that their floaters disappeared immediately after the operation. During the 12-month follow-up period, no patient showed any significant visual deterioration or recurrence of subjective floaters.[10] Other older data sets suggested only modest efficacy and possible safety concerns that made many doctors skeptical about the procedure.[11] It is essential to note that these older studies used laser technology not optimized for laser floater treatment. The latest developments and achievements in lasers, optics, and illumination systems that use the same optical pathway allow for simultaneous visualization of both the retina and the floater for more accurate treatment.
Principle of action
The mechanism of action is called “plasma formation” and “optical breakdown”, which are terms used to describe laser physics.[12] Optical breakdown requires a very high-frequency electrical field in the electromagnetic spectrum's optical region confined to a tiny area. The temperature at the center of the area of optical breakdown has been calculated to be several thousand degrees. The laser performs photoconversion of the solid floater into a gas with a combination of photochemical, thermal, thermoacoustic, and electromagnetic optical field effects. The laser must be firing in the range that obtains optical breakdown to change the form of matter from a solid to a liquid and, to some extent, to a gas. The gas bubbles that form float away and gradually dissolve. The dissolved gases can then pass across cell membranes and be carried away by the blood vessels. The smaller the focal area and the shorter the pulse width, the less energy is needed to create the plasma and associated shockwave. Due to the short duration of the pulse (4 ns), heat is dissipated before the next shot is fired. If the laser is fired into the vitreous below the optical breakdown level (normally about 2.2 mJ), the floaters will only be fragmented, and the success rate will be quite low.[13]
Indications
Most specialists are guided by the following criteria for selecting patients for laser vitreolysis for vitreous floaters:
- Patient has significant symptoms of floaters such as difficulty in driving, reading, computer use, significant annoyance, or their concentration significantly affected. [13][14][15][16] Since the procedure is performed to improve the patient's quality of life, it is not indicated for asymptomatic opacities.
- Patient has the floater longer than 2 months without significant improvement. Any debris associated with acute posterior vitreous detachment may disappear by the time of the treatment, which increases the probability of the patient remaining symptom-free after this period. In addition, posterior vitreous detachment becomes more complete which brings the floater forward for easier, safer treatment.[13][17]
- The opacity is at least 2 millimeters from the lens and retina. The laser focus should be set manually at a certain distance from the lens and retina. In most studies, a safety distance of 2-5 mm from the crystalline lens and 2-4 mm from the retina was determined.[13][16][18][19] In cases where the 2 mm threshold distance is not preserved, complications concerning the lens or retina can possibly occur.
Contraindications
The following contraindications for the procedure have been identified:[5][13][17]
- Floaters too numerous to treat
- Floaters caused by recurrent inflammation
- Floaters from fresh vitreous or pre-retinal hemorrhage
- Floaters associated with untreated, symptomatic retinal tears or untreated retinal detachment
- Floaters off the central visual axis to the point they are untreatable
- A floater that is so large that it could not be eliminated with reasonable laser power, a reasonable number of shots, and less than 5 treatment sessions.
- Corneal scars, irregularity, edema, or excessive lenticular astigmatism preclude adequate visualization of the target aiming beam
- Patients with a history of significant psychiatric problems that may recur or worsen if there is no improvement with treatment or if there were a complication.
- Uncompensated glaucoma or high intraocular pressure
Preoperative Management
A comprehensive eye exam includes:
- Special test questionnaires such as the Vitreous Floaters Functional Questionnaire (VFFQ) or the National Eye Institute Visual Functioning Questionnaire (VFQ) may be used to assess subjective feelings. A number of authors have shown the possibility of their effective use in patients with vitreous floaters.[20]
- [21] The patient can also draw opacities that interfere with him so that the surgeon can differentiate between symptomatic and asymptomatic opacities.
- Slit lamp biomicroscopy can be used to examine the anterior segment and central and posterior vitreous structure. For better visualization of the middle vitreous body special contact lenses can be used. Optimal visualization is key to performing laser floater treatment. Appreciating spatial context is crucial for safety and efficacy.
- The approximate refraction (helpful because it gives a general idea of the axial length of the eye, which may affect which surgical contact lens to choose).
- Measurement of intraocular pressure.
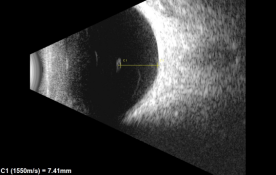
- B-scan ultrasound Ultrasound can be used to image opacities within the vitreous body. Quantitative ultrasonography of the vitreous provides a measure of floater severity.[22] [23]It is also used as the main method for determining the location of the opacity in relation to the retina and lens.
- Optical coherence tomography (OCT) This technology is helpful for the objective assessment of artifactual shadows of vitreous floaters.[16][24][25]
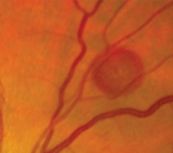
- Scanning Laser Ophthalmoscope (SLO) can be used to determine the position, size, and motility of the vitreous floaters with respect to the patient's visual axis. It is useful to perform image analysis of such SLO photos with the aim of quantifying the umbra and penumbra effects cast by vitreous opacities as a way of indexing floater size and density. Recent imaging studies have combined SD-OCT with scanning laser ophthalmoscopy to better evaluate the vitreomacular interface in various disease states, including vitreous floaters; [7][25][26]
Procedure
The following steps should be performed for successful laser vitreolysis: [10][13][17][18][19][27]
- Explain the purpose and nature of the procedure and obtain informed consent.
- Apply mydriatic drops.
- Apply topical anesthesia.
- Apply contact lens for vitreolysis: The contact lens is the best instrument to reveal the relationship of the floater to the patient’s retina and lens. These lenses increase the cone angles anterior and posterior to the contact lens and compress the diameter of the focus, increasing its irradiance.
- Set defocus to zero. The aiming beams of the laser are placed on the floater, and the laser is fired. This vaporizes a small part of the floater, frequently producing a gas bubble. The power setting is 3 to 10 millijoules with the larger setting used in the posterior vitreous and on the denser floaters. Most isolated floaters require less than 100 shots. It should be noted that the treatment efficiency and the required degree of laser exposure (the number of pulses and the total energy per session) depend on the initial type of opacity, structure, size, and density.
- No post-operative topical medication was prescribed.
- Follow-up treatments may be undertaken on the day after the previous session, although it may take up to a month to truly assess if another session is necessary based on symptoms. Patient symptomatic improvement can vary depending on the type of clinically significant vitreous opacities. The reported number of required sessions ranged between one and six. [10][13][17][18][19][27]
Complications
Cataract
A few small case series have described post-laser vitreolysis cataracts.[28][29][30][31][32]
The disruptive laser energy can subsequently lead to a defect of the posterior capsule, which could result in a cataract formation.
The absence of cataract formation, as a potential complication of laser vitreolysis, could be achieved by the safe distance to the crystalline lens and the low energy applied during laser treatment. It is important to mention that it cannot always be guaranteed to observe this safety distance, for example, due to unexpected patient movements, movement of floater during treatment, or difficulties with focusing the laser beam onto the vitreous opacities. Even if the safety distance was observed, high laser energy can unintentionally affect the lens or retina.
Retinal injury
Laser injury–related transient posterior pole retinal hemorrhages were reported.[13] [28][33][34]In one of these cases, the patient remained asymptomatic, while in the other, a transient scotoma was seen that lasted a few weeks and corresponded to the area of subretinal hemorrhage with nearby retinal whitening.
A few small case series have described post-laser vitreolysis retinal detachment.[19]
There is a report of retinal detachment when patients underwent laser vitreolysis immediately after Nd: YAG capsulotomy. Retinal detachments are associated with posterior capsulotomies probably because with that procedure, the vitreous can herniate through the created capsulotomy into the anterior chamber and thereby increase vitreous traction on the retina. [35]It is suggested that Nd: YAG capsulotomy may be performed first and then Nd: YAG vitreolysis may be performed after a safe interval and a thorough retinal examination.
Elevation of intraocular pressure
The intraocular pressure elevation after YAG laser vitreolysis has been reported.[17][28][36] Some cases had a transient or prolonged elevation of intraocular pressure, while others resulted in secondary glaucoma and trabeculectomy was required. [13][28]Although the pathomechanism explaining elevation in intraocular pressure is unknown, the authors hypothesized that the treatment may have caused the obstruction of the trabecular meshwork by floater debris, by inflammatory cells or macrophages, or by shockwave damage to the trabecular endothelial cells.[13][36]
There are some recommendations to prevent this complication: don’t operate on anyone with elevated pressure or glaucoma; don’t use an excessive number of shots (more than 300 total per eye); try to use fewer shots on any floater that is close to the trabecula; never widen a posterior capsulotomy at the same sitting as the floater treatment.[13]
Outcomes
The U. S. Food and Drug Administration when approving YAG lasers for this procedure classified this as a non-significant risk procedure. The spectrum of complications submitted to the ASRS ReST Committee is consistent with previous reports and indicates that complications remain relevant to laser vitreolysis as currently performed.
In cases of retinal detachment and raised IOP, it is not possible to determine whether there is a causal association between these complications and laser vitreolysis. Prospective studies are warranted to better understand the efficacy of this procedure and the frequency of attendant complications. Until then, practitioners should be aware of the profile of potential complications to properly inform patients during the consent process.
The position of focus and optimal energy applied during laser treatment is an important factor, which if miscalculated could result in complications. Using the patient’s subjective claim of the resolution of floaters as an outcome measure, the success rates claimed by existing publications are highly variable.[11][13][18][37][38][39]
Shah and colleagues were the first to conduct a randomized placebo-controlled trial evaluating the safety and efficacy of laser floater treatment using advanced YAG technology specifically designed for laser-based floater treatment. The study concluded that 54% of patients in the YAG laser group experienced symptomatic improvements compared to 9% of patients in the control group. The YAG laser group also showed greater improvement in the 10-point visual disturbance score than the control group.[18]
Summary
The currently available evidence offers some indications that YAG laser vitreolysis may be a viable option for the symptomatic relief of selected patients with bothersome complaints due to vitreous opacities. The advantages of Nd: YAG laser are that the eye remains closed and that the vitreous component is vaporized. Clearly, the importance of careful case selection, good history taking, detailed counseling, written informed consent, well-documented imaging, and careful postoperative follow-up cannot be overemphasized. [40]
Centrally suspended, single floaters might be the best candidates for vitreolysis or displacement, but this remains to be demonstrated. In particular, cases with chronic Weiss rings or solitary opacities may be the best candidates that will likely benefit the most from this procedure. On the other hand, notwithstanding how annoying the symptoms can be, the safety profile of this treatment seems far from optimal, considering that the presence of vitreous floaters is not a vision-threatening condition.
Obviously, appropriate trials will need to be conducted to determine indications and characterize the long-term safety and efficacy of the procedure.
Further reading
For Laser vitreolysis for vitreous wick syndrome please see Vitreous Wick Syndrome.
For Laser hyaloidotomy or membranotomy for preretinal or sub-internal limiting hemorrhage, please see Valsalva Retinopathy and Acquired Retinal Macroaneurysm.
References
- ↑ 1.0 1.1 Wagle AM, Lim WY, Yap TP, Neelam K, Au Eong KG. Utility values are associated with vitreous floaters. Am J Ophthalmol. 2011;152(1):60-5 e1.
- ↑ Zou H, Liu H, Xu X, Zhang X. The impact of persistent visually disabling vitreous floaters on health status utility values. Qual of Life Res 2013;22(6):1507-14.
- ↑ 3.0 3.1 Webb BF, Webb JR, Schroeder MC, North CS. Prevalence of vitreous floaters in a community sample of smartphone users. Int J Ophthalmol. 2013;6(3):402–405.
- ↑ Garcia GA, Khoshnevis M, Yee KMP, Nguyen-Cuu J, Nguyen JH, Sebag J. Degradation of Contrast Sensitivity Function Following Posterior Vitreous Detachment. Am J Ophthalmol. 2016 Dec;172:7-12. doi: 10.1016/j.ajo.2016.09.005. Epub 2016 Sep 12. PMID: 27633841.
- ↑ 5.0 5.1 5.2 Katsanos A, Tsaldari N, Gorgoli K, Lalos F, Stefaniotou M, Asproudis I. Safety and Efficacy of YAG Laser Vitreolysis for the Treatment of Vitreous Floaters: An Overview. Adv Ther. 2020 Apr;37(4):1319-1327. doi: 10.1007/s12325-020-01261-w. Epub 2020 Feb 21. PMID: 32086749; PMCID: PMC7140748.
- ↑ Tan HS, Mura M, Lesnik Oberstein SY, Bijl HM. Safety of vitrectomy for floaters. Am J Ophthalmol. 2011 Jun;151(6):995-8. doi: 10.1016/j.ajo.2011.01.005. Epub 2011 Mar 31. PMID: 21457930.
- ↑ 7.0 7.1 Milston R, Madigan MC, Sebag J. Vitreous floaters: Etiology, diagnostics, and management. Surv Ophthalmol. 2016 Mar-Apr;61(2):211-27. doi: 10.1016/j.survophthal.2015.11.008. Epub 2015 Dec 8. PMID: 26679984
- ↑ Schulz-Key S, Carlsson JO, Crafoord S. Longterm follow-up of pars plana vitrectomy for vitreous floaters: complications, outcomes and patient satisfaction. Acta Ophthalmol. 2011 Mar;89(2):159-65. doi: 10.1111/j.1755-3768.2009.01682.x. PMID: 19860781.
- ↑ Tripathy K. Is Floaterectomy Worth the Risks?. Asia Pac J Ophthalmol (Phila). 2017;6(3):303-304. doi:10.22608/APO.201738
- ↑ 10.0 10.1 10.2 10.3 Tsai WF, Chen YC, Su CY. Treatment of vitreous floaters with neodymium YAG laser. Br J Ophthalmol. 1993;77:485–8
- ↑ 11.0 11.1 Delaney YM, Oyinloye A, Benjamin L. Nd: YAG vitreolysis and pars plana vitrectomy: surgical treatment for vitreous floaters. Eye. 2002;16(1):21-6
- ↑ Zhang AY, Kumar D, Tripathy K. Laser Principles In Ophthalmology. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 20, 2022.
- ↑ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 13.11 Karickhoff JR. Laser Treatment of Eye Floaters. Washington: Medical Publishing LLC; 2005
- ↑ Le Goff MM, Bishop PN. Adult vitreous structure and postnatal changes. Eye (Lond). 2008 Oct;22(10):1214-22. doi: 10.1038/eye.2008.21. Epub 2008 Feb 29. PMID: 18309340.
- ↑ Fankhauser F, Kwasniewska S. Laser Vitreolysis. A review. Ophthalmologica. 2002 Mar-Apr;216(2):73-84. doi: 10.1159/000048303. PMID: 11919430.
- ↑ 16.0 16.1 16.2 Shaimova VA, Shaimov TB, Shaimov RB, Galin AY, Goloshchapova ZA, Ryzhkov PK, Fomin AV. Otsenka éffektivnosti YAG-lazernogo vitreolizisa na osnove ob''ektivnoĭ kolichestvennoĭ otsenki plavaiushchikh pomutneniĭ v steklovidnom tele [Evaluation of YAG-laser vitreolysis effectiveness based on quantitative characterization of vitreous floaters]. Vestn Oftalmol. 2018;134(1):56-62. Russian. doi: 10.17116/oftalma2018134156-62. PMID: 29543200.
- ↑ 17.0 17.1 17.2 17.3 17.4 Brasse K (2016) Elegant und wenig invasiv. Behandlung von Glaskörpertrübungen mit der YAG-Laservitreolyse.OphthalmolNachr6/2016:17
- ↑ 18.0 18.1 18.2 18.3 18.4 Shah CP, Heier JS. YAG laser vitreolysis vs sham YAG vitreolysis for symptomatic vitreous floaters: A randomized clinical trial. JAMA Ophthalmol 2017;135:9:918-923
- ↑ 19.0 19.1 19.2 19.3 Little HL, Jack RL. Q-switched neodymium: YAG laser surgery of the vitreous. Graefes Arch Clin Exp Ophthalmol. 1986;224(3):240-6
- ↑ de Nie KF, Crama N, Tilanus MA, Klevering BJ, Boon CJ. Pars plana vitrectomy for disturbing primary vitreous floaters: clinical outcome and patient satisfaction. Graefes Arch Clin Exp Ophthalmol. 2013 May;251(5):1373-82. doi: 10.1007/s00417-012-2205-3. Epub 2012 Dec 19. PMID: 23250478
- ↑ Broadhead GK, Hong T, Chang AA. To Treat or Not to Treat: Management Options for Symptomatic Vitreous Floaters. Asia Pac J Ophthalmol (Phila). 2020 Mar-Apr;9(2):96-103. doi: 10.1097/APO.0000000000000276. PMID: 32097127
- ↑ Oksala A: Ultrasonic findings in the vitreous body at various ages. Alb v Graefes Arch Klin Exp Ophthalmol 1978;207:275-80.
- ↑ Mamou J WC, Yee KM, Silverman RH, Ketterling JA, Sadun AA, Sebag J. Ultrasound-based quantification of vitreous floaters correlates with contrast sensitivity and quality of life. Invest Ophthalmol Vis Sci. 2015;56(3):1611-7.
- ↑ Kennelly KP, Morgan JP, Keegan DJ, Connell PP. Objective assessment of symptomatic vitreous floaters using optical coherence tomography: a case report. BMC Ophthalmol. 2015 Mar 8;15:22. doi: 10.1186/s12886-015-0003-5. PMID: 25884156; PMCID: PMC4355964.
- ↑ 25.0 25.1 Singh IP. Novel OCT Application and Optimized YAG Laser Enable Visualization and Treatment of Mid- to Posterior Vitreous Floaters. Ophthalmic Surg Lasers Imaging Retina. 2018 Oct 01;49(10):806-811.
- ↑ Vandorselaer T, Van De Velde F, Tassignon MJ. Eligibility criteria for Nd-YAG laser treatment of highly symptomatic vitreous floaters. Bull Soc Belge Ophtalmol. 2001;(280):15-9. PMID: 11486460.
- ↑ 27.0 27.1 A.V. Doga, D. A. Buryakov, B. A. Normaev. Clinical and functional results of YAG-laser vitreolysis in different types of vitreous floaters treatment. Available from: https://doi.org/10.25276/0235-4160-2019-1-44-49
- ↑ 28.0 28.1 28.2 28.3 Hahn P, Schneider EW, Tabandeh H, Wong RW, Emerson GG; American Society of Retina Specialists Research and Safety in Therapeutics (ASRS ReST) Committee. Reported Complications Following Laser Vitreolysis. JAMA Ophthalmol. 2017 Sep 1;135(9):973-976. doi: 10.1001/jamaophthalmol.2017.2477. PMID: 28750116; PMCID: PMC6583262.
- ↑ Koo EH, Haddock LJ, Bhardwaj N, Fortun JA. Cataracts induced by neodymium-yttrium-aluminium-garnet laser lysis of vitreous floaters. Br J Ophthalmol. 2017 Jun;101(6):709-711. doi: 10.1136/bjophthalmol-2016-309005. Epub 2016 Aug 29. PMID: 27574177. Case series.
- ↑ Noristani R, Schultz T, Dick HB. Cataract formation after YAG laser vitreolysis: importance of femtosecond laser anterior capsulotomies in perforated posterior capsules. Eur J Ophthalmol. 2016 Nov 4;26(6):e149-e151. doi: 10.5301/ejo.5000854. PMID: 27646329.
- ↑ Huang KH, Weng TH, Chen YJ, Chang YH. Iatrogenic Posterior Lens Capsule Rupture and Subsequent Complications due to Nd: YAG Laser Vitreolysis for Vitreous Floaters: A Case Report. Ophthalmic Surg Lasers Imaging Retina. 2018 Nov 1;49(11):e214-e217. doi: 10.3928/23258160-20181101-21. PMID: 30457659.
- ↑ O'Day R, Cugley D, Chen C, Fabinyi D. Bilateral posterior capsule injury after Nd:YAG laser vitreolysis: unintended consequence of floaters treatment. Clin Exp Ophthalmol. 2018 Nov;46(8):956-958. doi: 10.1111/ceo.13190. Epub 2018 Apr 6. PMID: 29573082.
- ↑ Baillif S, Paoli V, Francheschetti C, Gastaud P. Impact rétinien au cours d'une vitréolyse de corps flottants au laser ND-Yag [Retinal injury following ND-Yag laser treatment of symptomatic vitreous floaters]. J Fr Ophtalmol. 2011 Oct;34(8):589-91. French. doi: 10.1016/j.jfo.2010.12.001. Epub 2011 Apr 19. PMID: 21507513.
- ↑ Shields RA, Cheng OT, Wolfe JD. Iatrogenic Vitreous Hemorrhage, Subretinal Hemorrhage, and Branch Retinal Vein Occlusion after YAG Laser Vitreolysis for Symptomatic Vitreous Floaters. Ophthalmology. 2021 Apr;128(4):616. doi: 10.1016/j.ophtha.2020.10.026. PMID: 33745529.
- ↑ Liu X, Wang Q, Zhao J. Acute retinal detachment after Nd: YAG treatment for vitreous floaters and posterior capsule opacification: a case report. BMC Ophthalmol. 2020 Apr 19;20(1):157. doi: 10.1186/s12886-020-01428-7. PMID: 32306922; PMCID: PMC7168856
- ↑ 36.0 36.1 Cowan LA, Khine KT, Chopra V, Fazio DT, Francis BA. Refractory open-angle glaucoma after neodymium-yttrium-aluminum-garnet laser lysis of vitreous floaters. Am J Ophthalmol. 2015 Jan;159(1):138-43. doi: 10.1016/j.ajo.2014.10.006. Epub 2014 Oct 13. PMID: 25308785
- ↑ Aron-Rosa D, Greenspan DA. Neodymium:YAG laser vitreolysis. Int Ophthalmol Clin. 1985;25(3):125-34.
- ↑ Luo J, An X, Kuang Y. Efficacy and safety of yttrium-aluminum-garnet (YAG) laser vitreolysis for vitreous floaters. J Int Med Res. 2018 Nov;46(11):4465-4471. doi: 10.1177/0300060518794245. Epub 2018 Sep 10. PMID: 30200800; PMCID: PMC6259370.
- ↑ Shah CP, Heier JS. Long-Term Follow-Up of Efficacy and Safety of YAG Vitreolysis for Symptomatic Weiss Ring Floaters. Ophthalmic Surg Lasers Imaging Retina. 2020 Feb 1;51(2):85-88. doi: 10.3928/23258160-20200129-04. PMID: 32084280.
- ↑ Singh IP, Modern Vitreolysis - YAG Laser Treatment Now a Real Solution for the Treatment of Symptomatic Floaters, Survey of Ophthalmology (2020), doi: https://doi.org/10.1016/ j.survophthal.2020.02.006.