Lacrimal Gland Abscess
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Lacrimal gland abscess is a rare complication of dacryoadenitis. The clinical term acute suppurative dacryoadenitis is sometimes used to encompass lacrimal gland abscess, although with Computed Tomography (CT) imaging becoming more common, lacrimal gland abscess is now the more widely used nomenclature.
Etiology
Bacterial dacryoadenitis is a rare cause of dacryoadenitis and subsequent formation of a lacrimal gland abscess is even more rare. The most common organisms associated with lacrimal gland abscess are Staphylococcus sp., especially S. aureus, and many of these are methicillin-resistant S. aureus (MRSA).[1][2][3] Other associated causative organisms include Streptococcus sp., Klebsiella pneumonia, and Haemophillus influenzae.[1] A lacrimal gland abscess has also been reported with orbital tuberculosis.[4] Fungal and parasitic causes of infectious dacryoadenitis have been reported, and there is a single report of a lacrimal gland abscess where culture and histopathology confirmed a blastomycoses fungal infection.[5]
Epidemiology
Given its rarity, most data on lacrimal gland abscesses come from single case reports or small case series. The incidence of dacryoadenitis (all causes) is reported to be 1:10,000.[6] While the specific incidence of bacterial dacryoadenitis and lacrimal gland abscess has not been published, a 2021 study from a single institution reported that the incidence of bacterial dacryoadenitis as a cause of dacryoadenitis appears to have increased over the previous 15 years.[6]
Lacrimal gland abscesses appears to affect men and woman equally and may occur at any stage of life, with ages ranging from 2 years to >65 years reported in the literature.[1][6] Similar to acute bacterial dacryoadenitis, lacrimal gland abscesses typically present in a unilateral fashion, although there have been reports of bilateral lacrimal gland abscesses.[7][8] There is no data on whether the orbital or palpebral lobes of the lacrimal gland are more commonly affected.
Intravenous drug abuse, diabetes, HIV infection and other immunosuppressed states have been suggested as possible risk factors, however there is no data in the literature to confirm this. There are case reports of lacrimal gland abscesses associated with sinusitis,[9] hematogenous spread,[10] lacrimal gland cysts,[11] and a lacrimal gland ductule stone.[12]
Diagnosis
The diagnosis of lacrimal gland abscess is made based on clinical evaluation and radiographic imaging, and the etiologic agent is confirmed by microbiological or serologic testing. There is significant overlap in symptoms and signs between infectious and noninfectious dacryoadenitis, thus it is important to look for systemic markers of infection to aid in diagnosis.
Symptoms
The symptoms of lacrimal gland abscess follow those of dacryoadenitis and include pain, redness and swelling around the eyelid, difficulty opening the eyelid, pain with eye movements and diplopia. Lacrimal gland abscesses may also present with symptoms of discharge from the lacrimal gland or crusting around the lids.
Signs
On examination there may be periorbital edema and mechanical ptosis of the upper lid, periorbital erythema, conjunctival chemosis, extraocular motility restriction and tenderness to palpation over the lacrimal gland with resistance to retropulsion of the globe may also be found. In most reported cases of lacrimal gland abscess vision was 20/40 or better at presentation with severe vision loss being very rare.[6] Other signs of optic neuropathy such relative afferent pupillary defect and dyschromatopsia are also very rare. Systemically, patients may show fever and malaise. These systemic signs are important to help differentiate between infectious and noninfectious causes of lacrimal fluid collection.
Imaging
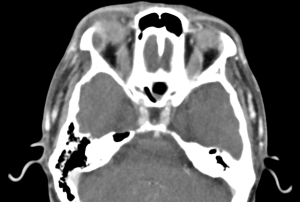
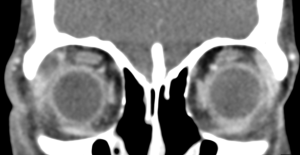
A contrast-enhanced computed tomography (CT) scan of the orbits will show enlargement of the lacrimal gland with a hypodensity and peripheral enhancement consistent with an abscess.[13][14] There may also be loculations of the abscess and fat stranding of the surrounding periorbita. On Magnetic Resonance Imaging (MRI) with diffusion-weighted imaging there may be restricted diffusion within the abscess.[14]
Laboratory test
There are no specific laboratory tests for diagnosis, although conjunctival culture, or culture of fluid collected during drainage may aid in identification of the causative organism and assist in choice of antibiotic therapy. Other work up may depend on the clinical context, but could include blood cultures, complete blood count (CBC) with differential to evaluate for leukocytosis, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level to evaluate for systemic inflammatory response, and where indicated, testing for immunodeficiency such as HIV.
Differential diagnosis
The differential for a lacrimal abscess includes non-infectious dacryoadenitis with a fluid collection, lacrimal gland tumors, lymphoproliferative disorders, foreign body granulomas, and sarcoidosis.[14]
Management
Medical therapy
Systemic broad-spectrum antibiotics with or without surgical drainage are the mainstay of therapy for lacrimal gland abscesses. Depending on the local rates of community-acquired MRSA, coverage for MRSA should be considered. Given the overlap with noninfectious dacryoadenitis, it may also be reasonable to consider a course of systemic steroids after appropriate antibiotic therapy has been initiated.
Surgery
While there are some reports of resolution of the abscess with observation alone, most studies suggest surgical drainage leads to prompt resolution with good outcomes.[1][6][15]
Surgical Technique
Whether the trans-septal or trans-conjunctival approach is preferred has not been studied. As with lacrimal gland biopsy, a trans-septal approach may spare the lacrimal gland ductules, however if the abscess is predominantly in the palpebral lobe, this approach may risk post-septal seeding of the infection and thus a trans-conjunctival approach may be preferred.
Prognosis
Most studies report generally good outcomes with minimal complications from lacrimal gland abscess.[1] With delay of initiation of antibiotics there is a risk of spread to contiguous tissues, however even with delay in diagnosis of weeks, case reports suggest once antibiotics are initiated and surgical drainage occurs, outcomes are still favorable.[6] Late complications may include ptosis and dry eye syndrome, although no rates of these complications have been reported.
Additional Resources
Radiopaedia Lacrimal Gland Abscess: https://radiopaedia.org/cases/orbital-abscess-lacrimal-gland-2?lang=us
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Liu W, Rootman DB, Berry JL, Hwang CJ, Goldberg RA. Methicillin-resistant Staphylococcus aureus dacryoadenitis. JAMA Ophthalmol. 2014;132(8):993-995. doi:10.1001/jamaophthalmol.2014.965
- ↑ Lai THT, Lai FHP, Chan TCY, Young AL, Chong KKL. Lacrimal gland abscess in children: Two case reports and literature review. Orbit Amst Neth. 2017;36(6):468-472. doi:10.1080/01676830.2017.1337197
- ↑ Savoie B, Rodgers R, Gorski M. Lacrimal gland abscesses: Case series and literature review. Orbit Amst Neth. 2017;36(6):428-432. doi:10.1080/01676830.2017.1337205
- ↑ Dalvin LA, Smith WM. Orbital and external ocular manifestations of Mycobacterium tuberculosis: A review of the literature. J Clin Tuberc Mycobact Dis. 2016;4:50-57. doi:10.1016/j.jctube.2015.11.001
- ↑ Kwan CC, Prager AJ, Huang RM, Bryar PJ, Thyparampil PJ. Dacryoadenitis Caused by Blastomycosis: A Case Report. Ophthal Plast Reconstr Surg. 2019;35(5):e116-e118. doi:10.1097/IOP.0000000000001445
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Wai KM, Locascio JJ, Wolkow N. Bacterial dacryoadenitis: clinical features, microbiology, and management of 45 cases, with a recent uptick in incidence. Orbit Amst Neth. 2022;41(5):563-571. doi:10.1080/01676830.2021.1966813
- ↑ Latasiewicz M, Chang-Sotomayor M, Alonso-Caldarelli C, Farias-Plazas F, Leszczynska A, Gonzalez-Candial M. Bilateral self-inflicted infectious dacryoadenitis. Orbit Amst Neth. 2014;33(6):465-467. doi:10.3109/01676830.2014.950292
- ↑ Srivastava, V V. Acute Suppurative Dacryoadenitis. Med J Armed Forces India. 2000;56(2):151-152. doi:10.1016/S0377-1237(17)30134-X
- ↑ Mirza S, Lobo CJ, Counter P, Farrington WT. Lacrimal gland abscess: an unusual complication of rhinosinusitis. ORL J Oto-Rhino-Laryngol Its Relat Spec. 2001;63(6):379-381. doi:10.1159/000055777
- ↑ Chandravanshi SL, Mishra V. Acute suppurative bacterial dacryoadenitis: a rare case report. Eur J Ophthalmol. 2014;24(5):790-792. doi:10.5301/ejo.5000459
- ↑ Eifrig CW, Chaudhry NA, Tse DT, Scott IU, Neff AG. Lacrimal gland ductal cyst abscess. Ophthal Plast Reconstr Surg. 2001;17(2):131-133. doi:10.1097/00002341-200103000-00011
- ↑ Mawn LA, Sanon A, Conlon MR, Nerad JA. Pseudomonas dacryoadenitis secondary to a lacrimal gland ductule stone. Ophthal Plast Reconstr Surg. 1997;13(2):135-138. doi:10.1097/00002341-199706000-00008
- ↑ McNab AA. Lacrimal gland abscess: two case reports. Aust N Z J Ophthalmol. 1999;27(1):75-78. doi:10.1046/j.1440-1606.1999.00131.x
- ↑ 14.0 14.1 14.2 Ginat DT, Glass LRD, Yanoga F, Lee NG, Freitag SK. Lacrimal gland abscess presenting with preseptal cellulitis depicted on CT. J Ophthalmic Inflamm Infect. 2016;6:1. doi:10.1186/s12348-015-0068-6
- ↑ Goold LA, Madge SN, Au A, et al. Acute suppurative bacterial dacryoadenitis: a case series. Br J Ophthalmol. 2013;97(6):735-738. doi:10.1136/bjophthalmol-2012-302302