Iris Cysts
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Iris cysts
- ICD-9 364.60
- ICD-10 H21.302
Etiology
An iris cyst is an epithelial-lined cyst that involves a layer of the iris. A primary iris cyst does not have a recognizable etiology. A secondary iris cyst has a recognizable etiology, such as surgical or nonsurgical trauma.[1]
Classification of Iris Cysts:[2]
- Primary Cysts
- Iris pigment epithelium cysts
- Iris stromal cysts
- Secondary Cysts
- Epithelial downgrowth
- Post-surgical
- Post-traumatic
- Cysts secondary to intraocular tumors
- Medication-induced
- Miotics (phospholine iodide, pilocarpine)
- Prostaglandins including latanoprost[3]
- Epithelial downgrowth
Epidemiology
Primary iris cysts are congenital and occur sporadically. Iris pigment epithelium cysts occur more commonly in adults while iris stromal cysts occur more in children.
General Pathology
Primary iris cysts are nonkeratinized squamous epithelial-lined structures that arise either from the posterior iris layer or stroma. Epithelium from stromal cysts contains goblet cells.[4]
Pathophysiology
The pathogenesis of primary iris cysts is not entirely understood, and proposed mechanisms in the literature are controversial. Iris pigment epithelial cysts are thought to be remnants of the marginal sinus of the iris that have not been obliterated. The presence of goblet cells in iris stromal cysts suggest that they are formed by entrapped surface ectoderm tissue likely during formation of the lens vesicle (4th week of embryogenesis).[5][6][7]
Primary iris cyst are most commonly of posterior pigment epithelial cell origin and located in the peripheral iris.[8]
Diagnosis
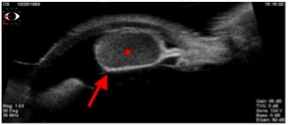
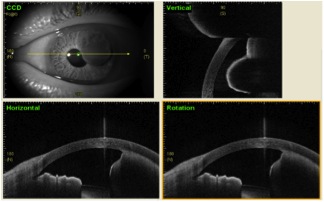
The diagnosis of iris cysts is based on the slit lamp exam and imaging by ultrasound biomicroscopy (UBM) or anterior segment optical coherence tomography (AS-OCT). Despite the high-resolution imaging of AS-OCT, UBM remains the gold-standard imaging due to ability to better characterize the interior of the cystic structurs.[9] UBM (35 MHz) has increased depth of penetration and visualizes ciliary body well. However, UBM (50 MHz) has higher resolution than 35 MHz probe.
History
Iris cysts are often found incidentally. Though they may be congenital, they may not be detected until late into the first or second decade of life. Patients may notice a “spot” on their iris.[10]
Rare reports exist in the literature describing an inheritance pattern of iris cysts, which may present as multiple or bilateral iris cysts in successive generations.[11]
Symptoms
The majority of patients are asymptomatic, however if there is progressive enlargement of the cyst, there is a higher likelihood of having symptoms. Symptoms may include blurry vision, photophobia, redness, and eye pain.
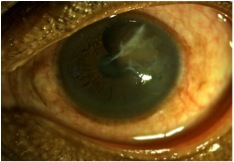
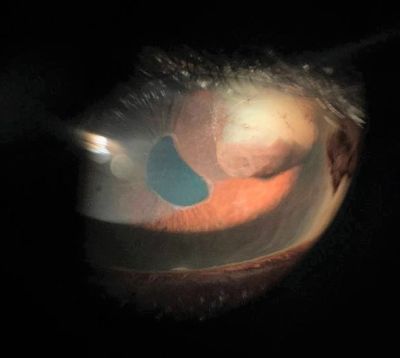
Physical examination
Cysts may have a round or collapsed appearance. Iris pigment epithelial cysts can be located on the anterior or posterior surface of the iris. They have a brown/black, velvety appearance and typically do not transilluminate. Iris stromal cysts appear as clear masses on the anterior surface of the iris and do transilluminate.[12]
Iris cysts secondary to trauma and subsequent epithelial implantation appear as serous or solid in continuity with the wound with or without membranes on the anterior iris surface.
It is important to rule out iris melanoma when evaluating an iris cyst. Iris melanomas appear as a brown lesion arising from the stroma. Unlike primary iris pigment epithelium cysts, they can be variably colored, maintain stable contour even after dilation. Presence of sentinel vessels and intrinsic vessels within the lesion are suggestive of a solid tumor rather than a benign cyst. UBM is very important to analyze the content of the iris cyst and to exclude malignancy.
Secondary complications
Depending on the size, location and compression of adjacent structures, the following complications may occur secondary to iris cysts:
- Angle-closure glaucoma
- Plateau iris syndrome
- Pigment dispersion syndrome
- Corneal edema
- Focal cataract
- Lens subluxation
- Iritis
Imaging
Ultrasound biomicroscopy (UBM) is the gold standard for imaging large iris cysts. Iris cysts appear round or ovoid with a thin, hyperechoic wall (due to the epithelial cell lining) and a hypoechoic interior (due to its fluid contents). [13]
Anterior segment optical coherence tomography (AS-OCT) may be of utility for small anterior iris lesions such as iris nevi but because of increased posterior shadowing, it is inferior to UBM for visualizing iris cysts.[9]
Differential diagnosis
The following may be considered in the differential diagnosis of iris masses[8]:
- Cystic
- Primary iris pigment epithelial cyst
- Primary iris stromal cyst
- Epithelial downgrowth
- Solid
- Melanocytic
- Nevus
- Melanocytoma
- Melanocytosis
- Lisch nodules
- Iris/ciliary body melanoma
- Leiomyoma
- Xanthogranuloma
- Metastasis to iris
- Epithelial
- Iris pigment epithelium adenoma
- Medulloepithelioma
- Melanocytic
Management
Medical treatment
Iris cysts secondary to miotics (phospholine iodide) are treated with phenylephrine 2.5%. Cysts also resolve with discontinuation of phospholine iodide or the implicated medication. [4]
General treatment
Iris cysts that are stable and not causing symptoms or secondary complications require no treatment but should be followed regularly. Iris cysts that involve the visual axis, particularly in children at risk for amblyopia, necessitate intervention.[14] Most authors recommend treating iris cysts using a step-wise approach, starting with less-invasive treatment prior to proceeding to surgical excision whenever possible.[11]
Surgery
- Laser Treatment
- Argon laser photocoagulation - photocoagulation of the cyst epithelium may be able to halt production of cystic fluid contents. This may be performed to shrink the cysts; though recurrence is common. Its utility is limited in cases of large cysts and when visualization is difficult.[15][16]
- Nd:YAG - photodisruption (laser cystostomy) of the cyst wall may allow perforation of the cyst and release of contents into the anterior chamber.[17]
- Cyst aspiration with injection of sclerosing agent- Aspiration of the cyst contents with subsequent injection of absolute alcohol to induce sclerosis and closure of the cystic cavity has demonstrated good success in a minimally-invasive method. Methods may vary, but a 27g infusion/aspiration needle can be used to first aspirate cyst contents, then infuse alcohol until the cyst wall turns grey, after which the alcohol is removed. [18] While recurrence is not common, this procedure can be repeated if it does occur.[19] Other sclerosing agents published in the literature include trichloroacetic acid, 5-fluorouracil, and mitomycin C.[19]
- En bloc excision - A more aggressive surgical approach is en bloc excision of the iris cyst with or without light cryotherapy. While this procedure has a good success rate, there is greater risk of causing collateral damage to ocular structures.[15]
- Secondary iris cysts due to epithelial downgrowth may require more aggressive surgical excision and devitalization of the epithelial tissues with vitrectomy, lensectomy, and cryodestruction of residual cells at the excision site.
Post operative complications
Postoperative complications depend on the amount of tissue removed. Complications can include cataract formation, corneal edema, glaucoma, and transient anterior segment inflammation.[10]
Prognosis
The prognosis of primary iris cysts is good, as the majority do not require treatment. Recurrence after excision is more common in stromal cysts than pigment epithelial cysts. The prognosis of secondary iris cysts is much more variable and those as a result of epithelial downgrowth typically carry a poor prognosis.
Acknowledgements
- Images courtesy of The Robert Cizik Eye Clinic, Houston, TX.
References
- ↑ Shields JA. 1981. Primary cysts of the iris. Trans Am Ophthalmol Soc 79: 771-809.
- ↑ Shields JA, Kline MW & Ausberger JJ. 1984. Primary iris cysts: a review of the literature and report of 62 cases. Br J Ophthalmol 68: 152-166.
- ↑ Tripathy K, Geetha R. Latanoprost. [Updated 2023 May 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK540978/
- ↑ Jump up to: 4.0 4.1 Primary Iris Cysts. AAO Basic and Clinical Science Course Section 6: Pediatric Ophthalmology and Strabismus. Elsevier, 2013.
- ↑ Grutzmacher RD, Lindquist TD, Chittum ME, Bunt-Milam AH & Kalina RE. 1987. Congenital iris cysts. Br J Ophthalmol 71: 227-234.
- ↑ Naumann G & Green WR. 1967. Spontaneous nonpigmented iris cysts. Arch Ophthalmol 78: 496-500. doi: 10.1002/archopht.1967.00980030498016.
- ↑ Paridaens AD, Deuble K & McCartney AC. 1992. Spontaneous congenital non-pigmented epithelial cysts of the iris stroma. Br J Ophthalmol 76: 39-42.
- ↑ Jump up to: 8.0 8.1 Shields CL, Kancherla S, Patel J, Vijayvargiya P, Suriano MM,Kolbus E, Badami A, Sharma P, Jacobs E, Voluck M, Zhang Z, Kansal R, Shields PW, Bianciotto CG & Shields JA. 2012. Clinically survey of 3680 iris tumors based on patient age at presentation. Ophthalmology 119: 407-414. doi: 10.1016/j.ophtha.2011.07.059.
- ↑ Jump up to: 9.0 9.1 Hau SC, Papastefanou V, Shah S, Sagoo MS, Restori M & Cohen V. 2014. Evaluation of iris and iridociliary body lesions with anterior segment optical coherence tomography versus ultrasound B-scan. Br J Ophthalmol doi: 10.1136/bjoohthalmol-2014-305218.
- ↑ Jump up to: 10.0 10.1 Lois N, Shields CL, Shields JA, Mercado G & De Potter P. 1998. Primary iris stromal cysts. A report of 17 cases. Ophthalmology 105: 1317-1322. doi: 10.1016/S0161-6420(98)97041-5.
- ↑ Jump up to: 11.0 11.1 Ilias Georgalas, MD, PhD*, Petros Petrou, MD, PhD, Dimitrios Papaconstantinou, MD, PhD, et al. Iris cysts: A comprehensive review on diagnosis and treatment. Surv Ophthalmol. 2018; 63:347-364
- ↑ Iris Melanoma. AAO Basic and Clinical Science Course Section 4: Ophthalmic Pathology and Intraocular Tumors. Elsevier, 2013.
- ↑ Marigo FA, Esaki K, Finger PT, Ishikawa H, Greenfield DS, Liebmann JM & Ritch R. 1999. Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology 106: 2131-2135. doi: 10.1016/S0161-6420(99)90495-5.
- ↑ Lois N, Shields CL, Shields JA & Mercado G. 1998. Primary cysts of the iris pigment epithelium. Clinical features and natural course in 234 patients. Ophthalmology 105: 1879-1885.
- ↑ Jump up to: 15.0 15.1 Haller J, Stark W, Azab A, Thomsen R & Gottsch J. 2003. Surgical Management of Anterior Chamber Epithelial Cysts. Am J Ophthalmol 135: 309-313. doi: 10.1016/S0002-9394(02)01960-8.
- ↑ Leung EW, Mehta JR & Croasdale CR. 2005. Laser photocoagulation of primary epithelial iris cysts. Arch Ophthalmol 123: 1276. doi: 10.1001/archopht.123.9.1276.
- ↑ Baranwal VK, Kumar S, Gaur S, et al. An uncommon case of primary iris cyst managed with Nd YAG laser. Med J Armed Forces India. 2015;71:S82e4
- ↑ Behrouzi Z, Khodadoust A. Epithelial iris cyst treatment with intracystic ethanol irrigation. Ophthalmology. 2003;110(8):1601e5
- ↑ Jump up to: 19.0 19.1 Shields CL, Arepalli S, Lally EB, Lally SE & Shields JA. 2014. Iris stromal cyst management with absolute alcohol-induced sclerosis in 16 patients. JAMA Ophthalmol 132: 703-708. doi: 10.1001/jamaophthalmol.2014.160.