Intranasal and Sinus Anatomy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
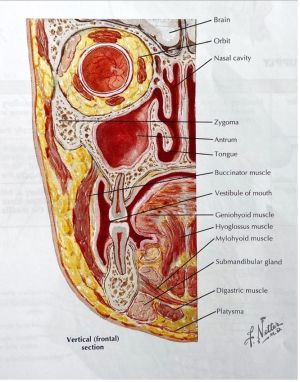
Orbit has a close anatomical relationship to paranasal sinuses
- Optic canal: sphenoid
- Roof: frontal
- Medial: ethmoid
- Floor: maxillary
A good understanding of sinus anatomy and their relationship to the critical ophthalmic structures is paramount in the management of orbital pathology and trauma, as well as some orbital or lacrimal procedures.
General Overview[1][2]
The paranasal sinuses are pairs of air-filled cavities with variable morphologies located within the bones of the skull. They are lined by a respiratory epithelium and have drainage at specific places on the lateral wall of the nasal cavity. The four of them- the maxillary, the frontal, the ethmoid and the sphenoid sinuses- are named based on their corresponding bones and are respectively (and approximately) inferior, superior, medial and posterior to the orbits. The sinuses are innervated by the ophthalmic and maxillary divisions of trigeminal nerve and their vasculature derives from the ophthalmic and maxillary arteries. Their functions include lightening the skull while severing as a buffer against fractures, resonating the voice, increasing the humidity and heat of inspired air, and insulating against sudden temperature changes. They also have immunological function.
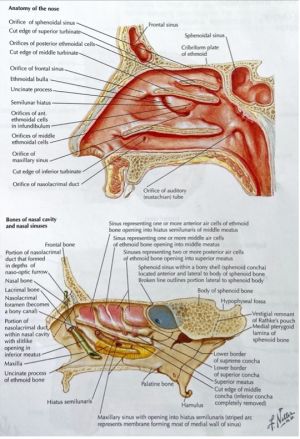
Nasal Cavity[1][3]
The sinuses as well as the nasolacrimal duct all have drainage into the nasal cavity, which is anatomically complex and bordered by multiple bones (and cartilage) of the cranium and face:
- Superior: nasal, frontal, body of the sphenoid, cribriform plate of the ethmoid (associated with olfactory epithelium and the olfactory bulb)
- Inferior: palatine process of the maxilla, horizontal plate of the palatine
- Septum: perpendicular plate of the ethmoid, vomer, septal (cartilage)
- Lateral: maxilla, ethmoid, palatine, medial pterygoid plate of the sphenoid, inferior nasal concha, lacrimal
The piriform aperture and choanae make up the anterior and posterior openings of the nasal cavity. In addition, the nasal cavity communicates with the pterygopalatine fossa through the sphenopalatine foramen, located posteriorly on the lateral wall.
Relations to surrounding structures are as follows :
- Superior: frontal sinus, sphenoid sinus, anterior cranial fossa
- Inferior: palate, oral cavity
- Medial: other half of nasal cavity
- Lateral: maxillary sinus, ethmoid sinuses, orbit, and pterygopalatine fossa
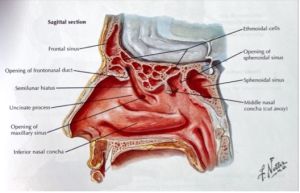
The lateral wall of the nasal cavity is of great significance in respect to the paranasal sinuses. Three large shelf-like protrusions, called nasal conchae (also known as turbinates) serve as landmarks for locating drainage of each of the sinuses (more details in the subsequent sections). Inferior to each concha is an air space called meatus. The posterior ethmoid sinus drains into the superior meatus, which is inferior to the superior concha. The middle and anterior ethmoid, maxillary and frontal sinuses drain inferior to the middle concha into the middle meatus. The nasolacrimal duct drains into the inferior meatus. The sphenoidal sinus drains into the sphenoethmoidal recess superior to the superior concha. In up to 52% of cases, the supreme nasal concha is present superior to the superior nasal concha.
Arteries supplying the nasal cavity includes anterior and posterior ethmoid (from ophthalmic), sphenopalatine and greater palatine (from maxillary), and superior labial (from facial). Innervation of sensation is by ophthalmic and maxillary divisions of the trigeminal nerve, olfaction by olfactory nerve (CN1) and autonomic functions by postganglionic fibers traveling along the maxillary division of the trigeminal nerve from the pterygopalatine ganglion (parasympathetic) and the superior cervical ganglion (sympathetic).
Clinical significance
A general understanding of the nasal anatomy is useful in nasolacrimal duct procedures (i.e. NLD probing and stenting). Upon entry in the nares, the retrieving device should be directed laterally and inferiorly, and it should run along the junction of the lateral wall and floor of the nasal cavity to be inserted into the inferior meatus.
Ethmoid Sinus
The ethmoid sinuses are composed of 3-18 pairs of air cells within the ethmoid labyrinth and can be divided into anterior, middle and posterior ethmoid cells with distinct drainage locations in the nasal cavity. These thin-walled cavities can invade the other paranasal sinuses. Relations to surrounding structures are as follows:
- Superior: anterior cranial fossa, frontal bone and sinus
- Medial: nasal cavity
- Lateral: orbit
The posterior ethmoid cells drain into the superior meatus or the sphenoethmoidal recess. The middle ethmoid cells account for the ethmoid bulla, a bulge in the middle meatus just inferior to the middle concha, which is also the approximate location of drainage. The anterior cells drain into the semilunar hiatus of the middle meatus through the ethmoid infundibulum or the frontonasal duct.[1]
The most anterior ethmoid cell is called agger nasi cell. It shares its posterior wall with the frontonasal duct, found posteromedially and superiorly, and relates to the lacrimal bone anteriorly. Frontal cells are formed through pneumatization of the anterior wall of frontonasal duct by anterior ethmoid cells and can be found posterosuperiorly to the agger nasi cell.[4]
Practically speaking, four parallel lamellae with oblique orientation make up the complex ethmoid labyrinth and correlate to specific structures found on the lateral wall of the nasal cavity: the uncinate process, the ethmoid bulla, the basal lamella of middle concha, and the superior concha.[4]
The ethmoid sinuses are supplied by the anterior ethmoid and posterior ethmoid branches of the ophthalmic artery as well as the posterior lateral nasal branches of the sphenopalatine artery. More precisely, the anterior and posterior ethmoidal branches enter the sinus from the orbit at the level of fronto-ethmoid suture. The anterior ethmoidal foramen is located approximately 24 mm behind the anterior lacrimal crest, and the posterior ethmoidal foramen, 12 mm behind the anterior lacrimal crest. Innervation is supplied by anterior ethmoid and posterior ethmoid nerves (from the nasociliary nerve), posterior lateral superior nasal nerve (from the pterygopalatine ganglion), and posterior lateral inferior nasal nerve (from the greater palatine nerve). The anterior and middle air cells drain to the submandibular lymph nodes, the posterior air cells to the retropharyngeal lymph nodes.[1]
Clinical significance
Ethmoid sinus has several anatomical variants. The onodi cell is also known as the sphenoethmoidal air cell. A mucocele in this structure can compress the optic nerve, causing an acute retrobulbar optic neuropathy. The agger nasi cell is the most anterior ethmoid air cell, intervenes between lacrimal sac fossa and middle turbinate of the nasal cavity. This structure must be removed in dacryocystorhinostomy (DCR) due to its localisation between lacrimal sac fossa and middle turbinate. The concha bullosa is formed from the pneumatization of middle turbinate, while the haller cell is formed from the pneumatization of medial orbital floor.[5]
Lamina papyracea forms the medial wall of the orbit. This is a thin bony structure that has important clinical relevance. In pediatric patients, paranasal sinusitis most often involves the ethmoid sinus, and it can spread through the thin lamina papyracea of the medial orbital wall into the orbit, resulting in an orbital cellulitis.[6] Furthermore, damage to the lamina papyracea is a potential complication of endoscopic sinus surgery. This can lead to permanent ocular motility disorder and visual impairment due to its proximity to the extraocular muscles and optic nerve.[7]
Frontal Sinus[1][4]
The frontal sinuses are a pair of typically asymmetric and triangular air cavities separated by the frontal septum. Relations to surrounding structures are as follows:
- Superior: anterior cranial fossa
- Inferior: orbit, anterior ethmoidal sinuses, nasal cavity
- Anterior: forehead, superciliary arches
- Posterior: anterior cranial fossa
- Medial: the other frontal sinus
It communicates with the nasal cavity through the frontonasal duct (also known as the frontal recess), which opens into the middle meatus or the ethmoidal infundibulum. The frontonasal duct’s boundaries are agger nasi cell anteriorly, lamina papyracea laterally and middle concha medially.
The frontal sinus gets its arterial supply from the anterior ethmoid, supraorbital and supratrochlear branches of the ophthalmic artery. Its innervation is via the supraorbital and supratrochlear nerves. Its lymphatic drainage is through the submandibular lymph nodes.
Clinical significance
A mucocele developing in the frontal sinus can compress orbital contents inferiorly, causing hypoglobus and ophthalmoplegia.
Frontal sinus fractures are of rare occurrence in adult population, as the frontal bone is very strong and resistant to trauma. Only trauma with significant energy can result in frontal sinus fracture. Therefore, this type of fracture is highly associated with traumatic brain injury due to its association with high-velocity trauma. Other potential sequelae from a frontal sinus fracture include frontal sinusitis secondary to frontal sinus outflow obstruction, as well as traumatic orbital cephalocele. Traumatic orbital cephalocele refers to the herniation of the intracranial contents with displacement of the globe secondary to a large defect in the roof of an orbit.[8]
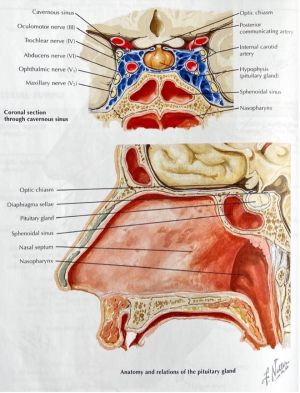
Sphenoid Sinus[1][4]
The sphenoid sinuses are the most posterior of paranasal sinuses. They are of irregular shape and are asymmetric due to the irregular septum. Relations to surrounding structures are as follows:
- Superior: hypophyseal fossa, pituitary gland, optic chiasm (the optic nerve indents the sinus roof anteroposteriorly and in 4% of cases, there is bone dehiscence)
- Inferior: nasopharynx, pterygoid canal
- Medial: other sphenoid sinus
- Lateral: cavernous sinus, internal carotid artery (in 25% of cases, the lateral wall of the sinus adjacent to the artery is dehiscent), cranial nerves III, IV, V1, V2 and VI
- Anterior: nasal cavity
The sphenoethmoidal recess is the location of drainage into the nasal cavity and can be found in the superior meatus or above the superior concha.
Arterial supply comes from the posterior ethmoid branch of the ophthalmic artery as well as the posterior lateral nasal branches of the sphenopalatine artery. The posterior ethmoid nerve (from the ophthalmic division of the trigeminal nerve) and the orbital branch (from the pterygopalatine ganglion) innervate the sphenoid sinus. Lymphatic drainage is to the retropharyngeal lymph nodes.
Clinical significance
Sphenoid sinus is in close relationship with the optic canal. In fact, the optic canal is located superior and lateral to the sinus wall. Sinusitis within the sphenoid sinus and the posterior cell of ethmoid sinus can thus compress the optic nerve, causing an acute retrobulbar optic neuropathy.
Maxillary Sinus[1][4]
The maxillary sinuses are the greatest in size of all the paranasal sinuses. They have thin bony walls and are shaped like pyramids whose base is the lateral wall of nasal cavity and the apex toward the zygomatic process of the maxilla. Relations to surrounding structures are as follows:
- Anteromedial: nasolacrimal duct
- Superior: orbit, infraorbital nerve and vessels
- Inferior: roots of molars and premolars
- Medial: nasal cavity
- Lateral and anterior: cheek
- Posterior: infratemporal fossa, pterygopalatine fossa
The floor of the maxillary sinus can occasionally be interrupted by the protrusion of the roots of upper premolars and molars, and can drop inferiorly via resorption of alveolar bone after tooth loss. Another anatomical feature related to tooth loss is the formation of secondary septa within the sinus; primary septa are developmental. The roof of the maxillary sinus correlates with the orbit floor, where the infraorbital nerve and artery courses through the infraorbital groove, into the canal and exits via the foramen of the same name on the anterior wall of the sinus. The maxillary tuberosity makes up the posterior wall and is in close proximity to the pterygopalatine fossa and its contents. The maxillary sinus communicates with the nasal cavity medially through its ostium in the nasal fontanelle and into the semilunar hiatus of middle meatus .
The maxillary sinus is supplied by the anterior superior alveolar, middle superior alveolar and posterior superior alveolar branches of the maxillary artery, diverging from the external carotid artery; the posterior lateral nasal artery also contributes to the blood supply of the sinus. Its innervation is by the infraorbital nerve (from the maxillary division of the trigeminal nerve) as it branches into the anterior superior alveolar and middle superior alveolar nerves. The posterior superior alveolar nerve branching directly off from the maxillary division also innervates part of the sinus. The lymphatic drainage of the maxillary sinus is through the submandibular lymph nodes.
Clinical relevance
The roof of sinus forms floor of orbit. The infraorbital neurovascular bundle travels along roof of sinus, therefore an orbital floor fracture can damage the infraorbital nerve, resulting in paresthesia or numbness of the infraorbital distribution. The bone is thinner medial to the infraorbital canal, therefore blow-out fractures usually involve the medial part of the orbital floor.[5]
Nasolacrimal duct travels anteromedial to sinus. Therefore, a secondary acquired nasolacrimal duct obstruction can occasionally occur in cases of midfacial trauma (e.g. naso-orbito-ethmoid fracture) or sinus mucoceles causing mechanical compression. For more information on secondary acquired nasolacrimal duct obstruction, please visit: Secondary Acquired Nasolacrimal Duct Obstruction
Silent sinus syndrome is associated with asymptomatic chronic maxillary sinusitis. It is initiated by an impaired outflow through the ostiomeatal complex. This obstruction results in the chronic fluid accumulation, resorption, and thus negative pressure in the maxillary sinus. The final pathogenesis pathway leads to maxillary sinus atelectasis and collapse of orbital floor. Clinical manifestations include unilateral enophthalmos, ptosis, hypoglobus and vertical diplopia. The CT scan reveals unilateral maxillary sinus hypoplasia and opacification, orbital expansion, lateralization of uncinate process. [9]For more information on secondary acquired nasolacrimal duct obstruction, please visit: Silent Sinus Syndrome
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Norton NS, Netter FH. Netter’s Head and Neck Anatomy for Dentistry.; 2017
- ↑ St-Amant M. Supreme nasal concha. Radiopaedia. doi:10.53347/rID-59452
- ↑ Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy.; 2017. Accessed March 2, 2022. http://public.eblib.com/choice/PublicFullRecord.aspx?p=6280165
- ↑ 4.0 4.1 4.2 4.3 4.4 Cappello ZJ, Minutello K, Dublin AB. Anatomy, Head and Neck, Nose Paranasal Sinuses. In: StatPearls. StatPearls Publishing; 2022. Accessed March 2, 2022. http://www.ncbi.nlm.nih.gov/books/NBK499826/
- ↑ 5.0 5.1 Flint PW, Haughey BH, Lund VJ, et al., eds. Cummings Otolaryngology-Head and Neck Surgery. 7th ed. Elsevier; 2020.
- ↑ Yen MT, Yen KG. Effect of corticosteroids in the acute management of pediatric orbital cellulitis with subperiosteal abscess. Ophthalmic Plast Reconstr Surg. 2005;21(5):363-366; discussion 366-367. doi:10.1097/01.iop.0000179973.44003.f7
- ↑ Ramadan HH, Allen GC. Complications of endoscopic sinus surgery in a residency training program. Laryngoscope. 1995;105(4 Pt 1):376-379. doi:10.1288/00005537-199504000-00007
- ↑ Doonquah L, Brown P, Mullings W. Management of frontal sinus fractures. Oral Maxillofac Surg Clin North Am. 2012;24(2):265-274, ix. doi:10.1016/j.coms.2012.01.008
- ↑ Annino DJ, Goguen LA. Silent sinus syndrome. Curr Opin Otolaryngol Head Neck Surg. 2008;16(1):22-25. doi:10.1097/MOO.0b013e3282f2c9aa