Extraocular Muscles
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Diagnostic Intervention
Description/Overview
Introduction
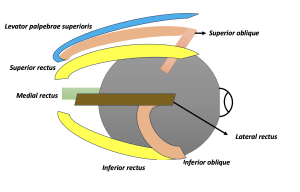
Extraocular muscles are the most specialized skeletal muscles in the human body. These are broadly divided into voluntary and involuntary muscles. The voluntary muscles include seven extraocular muscles that control the movements of the eye and eyelids, and are important for binocular single vision. These include four recti muscles, two oblique muscles, and levator palpebrae superioris. The four recti include the superior, inferior, medial, and lateral rectus. The two oblique muscles include the superior oblique and inferior oblique. These six muscles are responsible for the movement of eyes into different gazes. The levator palpebrae superioris is responsible for eyelid elevation. The involuntary muscle group include superior tarsal muscle (Muller's muscle), inferior tarsal muscle and orbitalis. Understanding the principles of extraocular muscle movements plays a key role in the diagnosis of various strabismus pathologies.[1]
Embrology
The orbit and the extraocular muscles are embryologically derived from the mesoderm and the neural crest cells. The extraocular muscles per se are derived from the mesoderm, and the connective tissue surrounding the muscles is derived from the neural crest cells.[2] The extraocular muscles are thought to arise from two different subsets of mesenchymal cells including the paraxial and prechordal head mesoderm.[3] The lateral rectus and superior oblique arise from the unsegmented paraxial head mesoderm, whereas the superior, inferior, medial rectus and the inferior oblique are thought to arise from the prechordal head mesoderm.[4]
Blood Supply
Arterial Supply
The extraocular muscles (EOM) receive their major blood supply from the ophthalmic artery's medial and lateral muscular branches. The medial muscular branch supplies the medial rectus, inferior rectus, and inferior oblique.[5] The lateral muscular branch supplies the lateral rectus, superior rectus and oblique, and the levator palpebrae superioris. The superior, inferior, and medial rectus muscles receive blood supply via two anterior ciliary arteries that communicate with the anterior circle of the ciliary body. The lateral recti muscle receives blood supply from a single branch of the lacrimal artery. The inferior rectus and inferior oblique also receive partial blood supply from the infraorbital artery, a branch of the maxillary artery.[6]
Venular Supply
Venous drainage occurs through the vortex veins into the superior and inferior orbital veins. Vortex veins are located along the lateral and medial aspects of the superior and inferior rectus muscles. These vortex veins then drain into the orbital venous system.[7]
Applied Aspects
There is a risk of iatrogenic damage to the vortex veins during surgery on IR or SR. The blood supply of EOM also supplies most of the anterior segment. Thus, procedures involving damage to vascular supply should be limited to a maximum of two rectus muscles at a time given the increased risk of anterior segment ischemia.[8]
Nerve Supply
The chief nerve supply of the extraocular muscles is received from the third, fourth, and sixth nerves. The third (Oculomotor) nerve supplies multiple extraocular muscles, while the fourth (Trochlear) and the sixth (Abducent) nerve supply individual extraocular muscles.[9] Details of the nerve supply of different extraocular muscles are mentioned in Table 1.
| S.No | Nerve Supply | Extraocular Muscles Supplied |
|---|---|---|
| 1 | Oculomotor nerve – Superior division | Superior rectus, Levator palpebrae superioris |
| 2 | Oculomotor nerve – Inferior division | Medial rectus, Inferior rectus, Inferior oblique |
| 3 | Trochlear nerve | Superior oblique |
| 4 | Abducens nerve | Lateral rectus |
Origin of Extraocular Muscles
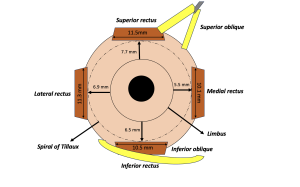
The rectus muscles originate from the annulus of Zinn, which is a common tendinous ring lying in the back of the orbit.[10] The superior rectus originates from the upper part of the annulus of Zinn, which is attached to the dura mater of the optic nerve.[11] The levator palpebrae superioris arises medial and superior to the origin of the superior rectus muscle. The other recti muscles, i.e., the medial, inferior, and lateral recti, also arise from the annulus of Zinn. Each of the recti muscles courses anteriorly along the orbit’s walls and gets inserted into the sclera at varying distances, as shown in Figure 1. The four recti muscles form the muscle cone within the orbit.[12] The apex of the muscle cone is at the annulus of Zinn, the point of origin of the recti muscles. The cone widens as the muscles progress anteriorly, forming its base at the points of muscle penetration into the tenon’s sheath. Each muscle is enclosed by the fibrous capsule, which is attached by a thin continuous membrane called an “intermuscular septum”. The intermuscular septum divides the orbital fat pad into intraconal and extraconal fat.[13]
The medial rectus inserts closest to the limbus, around 5.5mm, followed by the inferior rectus, which inserts at 6.5mm; the lateral rectus at 6.9mm and the superior rectus inserts farthest from the limbus, which is 7.7mm.[1] These insertion distances may vary from individual to individual. The spiral formed by joining the insertion points of the four recti muscles is referred to as the Spiral of Tillaux, as shown in Figure 2. The origin and insertion of each muscle are discussed under separate headings below.
Applied Anatomy
The Trochlear nerve passes above the annulus of Zinn and does not lie within the muscle cone. Thus, the retrobulbar anesthesia, directed into the muscle cone, spares the trochlear nerve and, therefore, the superior oblique muscle.[14]
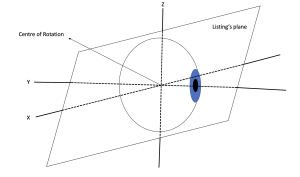
Listing Plane and Fick’s Axis
The listing plane is an imaginary equatorial plane containing the globe's center of rotation.[15] Fick’s axis is the axis around which the globe rotates. X and Z axis are included in the Listing plane, and the Y axis is a sagittal axis that lies perpendicular to the Listing plane. Vertical rotations occur around the X-axis, horizontal movements around the Z-axis, and torsional around the Y-axis.[16] The different Fick’s axis and movements around each axis are demonstrated in Figure 3.
Description of Individual Muscles
Medial Rectus (MR)
Course: The medial rectus originates from the medial part of the annulus of Zinn at the orbital apex and passes forward to get inserted at around 5.5mm away from the limbus. The medial rectus has the shortest tendon (4.5mm) among all the recti muscles. This is the only rectus muscle with no oblique muscle running tangentially.[17]
Action – Adduction[5]
Innervation – Oculomotor nerve (Third cranial nerve)[18]
Applied aspects – In case the medial rectus muscle gets lost or slips following trauma or iatrogenic causes such as during squint or pterygium surgery, there is no reference point to retrieve this muscle.[19]
Lateral Rectus (LR)
Course: The lateral rectus originates from the lateral part of the annulus of Zinn and progresses forwards to get inserted approximately 6.9mm from the limbus. The lateral rectus muscle has the broadest arc of contact, i.e., 12mm, among all the recti muscles.[20] The lateral rectus is the thinnest extraocular muscle having a width of only 9.2 mm. The intermuscular septa attach the lateral rectus to the inferior oblique muscle.
Action – Abduction
Innervation – Abducens nerve (Sixth cranial nerve)
Applied aspects - During recession or resection procedures, the lateral rectus must be separated from the inferior oblique fibers. Otherwise, there might be an inadvertent shifting of the inferior oblique tendon with the lateral rectus.[21]
Superior Rectus
Course: The superior rectus muscle originates from the superior part of the annulus of Zinn and proceeds anteriorly along the orbital wall to get inserted into the sclera at a distance of approximately 7.7mm from the limbus. The superior rectus is attached to the fibers of the levator palpebrae superioris that courses above this muscle from the point of origin. The superior oblique muscle lies between the superior rectus and the sclera.[22] Both the muscles are connected to each other by the intermuscular septa.
Action – Primary action is elevation. Additional actions include incyclotorsion and adduction.
Innervation – Oculomotor nerve (Third cranial nerve)
Applied aspects – A pseudoptosis may appear in a hypotropic eye as the upper eyelid follows the superior rectus muscle. A squint surgery involving superior rectus resection can result in drooping of the upper lid.[23]
Inferior Rectus (IR)
Course: The inferior rectus muscle originated from the inferior part of the annulus of Zinn and then proceeds anteriorly to get inserted at an approximate distance of 6.5mm from the limbus. The inferior oblique muscle passes beneath the inferior rectus.[24] The inferior rectus muscle is also strongly connected to the lower eyelid retractors.
Action – Primary action is depression. Additional actions include excyclotorsion and adduction.
Innervation – Oculomotor nerve (Third cranial nerve)
Applied Aspects – Recession or resection procedures involving the inferior rectus muscle may result in widening or narrowing of the lower eyelid, respectively.[23]
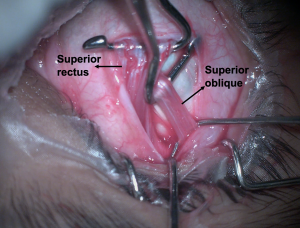
Superior Oblique
Course: The superior oblique muscle originates from the periosteum of the sphenoid bone, superomedial to the optic foramen, and the common tendinous ring. It then progresses anteriorly, parallel to the medial wall of the orbit, to reach the trochlea.[25] The trochlea is a cartilaginous loop attached to the frontal bone's nasal part. After looping through the trochlea, the muscle becomes a tendon, turning posterolateral and passing beneath the superior rectus. It finally gets inserted posterior and lateral to the insertion of the superior rectus, as shown in Figure 4. The superior oblique is the longest muscle of all the extraocular muscles.
Action – Primary action is incyclotorsion. Additional actions include depression and abduction.
Innervation – Trochlear nerve (Fourth cranial nerve)
Applied aspects - The superior oblique is the only muscle that receives innervation from the Trochlear nerve. The trochlear nerve is the only cranial nerve that emerges from the posterior aspect of the brainstem.[26]
Inferior Oblique (IO)
Course: It originates from the orbital floor lateral to the nasolacrimal groove. The muscle then runs along the orbit floor and crosses below the inferior rectus muscle. It then ascends posterolateral to pass between the lateral rectus and the orbit floor. It then inserts posterior to the equator in the inferolateral quadrant onto the sclera. The fascial sheath of the inferior oblique blends with the sheath of the inferior rectus, which then blends with the medial and lateral check ligaments.[27] The fusion of all these forms the suspensory ligament of the eyeball, which is a hammock-like sling that supports the eyeball. The inferior check ligament is an anterior expansion from the fused sheaths of the inferior rectus and oblique muscles that attach to the tarsus muscle of the lower eyelid.[28]
Action – Primary action is excyclotorsion. Additional actions include elevation and abduction.
Innervation – Oculomotor nerve (Third cranial nerve)
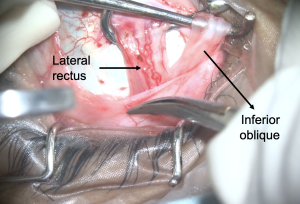
Applied Aspects – Inferior oblique muscle overaction is commonly associated with congenital squints, especially congenital esotropias.[29] The inferior oblique is the only muscle that must be retrieved from the tenons, not directly from the scleral insertion point. Since the fibers are closely associated with the lateral rectus, isolating the inferior oblique while operating on the lateral rectus muscle is important, as shown in Figure 5.
Levator Palpebrae Superioris (LPS)
Course: The LPS is a thin triangular muscle extending along the bony orbit’s roof. It originates from the inferior aspect of the lesser wing of the sphenoid, superior to the annulus of Zinn. The muscle originates as a short and narrow tendon, which fans out and gradually widens as it courses anteriorly.[30] Once it reaches the Whitnall’s ligament, a transverse suspensory ligament, the LPS muscle becomes more tendinous and changes its direction to become vertical, called the vertical levator aponeurosis. The levator aponeurosis has multiple insertions. The aponeurosis has medial and lateral wings which attach to the medial and lateral canthal tendons, respectively. It inserts anteriorly into the upper eyelid skin, inferiorly into the anterior surface of the upper tarsal plate, and has few extensions to the superior conjunctival fornix.
Action- Elevates upper eyelid
Innervation- Oculomotor nerve (Third cranial nerve)
Applied Aspects- Myogenic or neurogenic problems related to LPS can lead to ptosis.[31] It is essential to separate the LPS from the superior rectus during squint or ptosis surgery to avoid iatrogenic side effects on the lid position.
Arc of Contact
All the rectus muscles arise from the annulus of Zinn and proceed anteriorly to reach the globe. The point of tangency is where the muscle first comes in contact with the globe. This point of first contact is defined as the effective insertion point of muscle that determines the vector of force exerted by the muscle.[32] The arc of contact is defined as the circular area the muscle travels from the first point of contact (point of tangency) to the anatomical insertion point. Applied aspects: Recession of muscle acts by shortening its effective length and arc of contact. Resection has a strengthening effect as it increases the effective length as well as the arc of contact.[33]
Actions of Extraocular Muscles
All the extraocular muscles are responsible for the eye’s movement in different gazes. There are a few basic concepts that are important to understand muscle actions. The extraocular muscles have different actions in different eye positions.[34] The primary action of the muscle is the major action of muscle in the primary position. Subsidiary actions are which occur in different positions of the globe. The different muscle actions are listed in Table 2.
| Muscle | Primary Action | Secondary Action | Tertiary Action |
|---|---|---|---|
| Lateral rectus | Abduction | - | - |
| Medial rectus | Adduction | - | - |
| Superior rectus | Elevation | Intorsion | Adduction |
| Inferior rectus | Depression | Extorsion | Adduction |
| Superior oblique | Intorsion | Depression | Abduction |
| Inferior oblique | Extorsion | Elevation | Abduction |
| Levator palpebrae superioris | Elevation of upper lid | - | - |
Types of Eye Movements
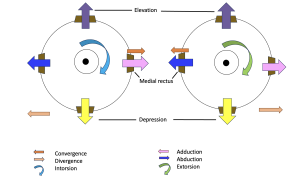
Ductions - These are monocular movements around the Fick’s axis. These include adduction, abduction, elevation, depression, intorsion, and extorsion.
Versions - These are binocular, simultaneous, conjugate movements. These include dextroversion, levoversion, elevation, depression, dextroelevation, dextrodepression, levoelevation, levodepression, dextrocycloversion, or levocycloversion.[35]
Vergences - These are bilateral, simultaneous, disconjugate movements. These include convergence and divergence. These are shown in Figure 6.
Positions of Eye
Primary - This is defined as the eye position when one is looking straight ahead with an erect head and body, the object of regard at infinity, and lies at the intersection of the sagittal plane of the head and a horizontal plane passing through the center of rotation of two eyeballs.[36]
Secondary - These include eye positions obtained with movement around the X and Z axis. These include adduction, abduction, elevation, or depression.[37]
Tertiary - These include movement of the globe around the Y axis, that is, detroelevation, dextrodepression, levoelevation, and levodepression.
Positions of Gaze
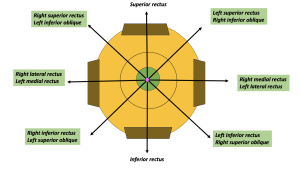
Cardinal positions - There are six cardinal positions. In each eye, one principal muscle is responsible for moving the eye into that position.[38]
Diagnostic positions - There are a total of nine diagnostic positions. These include the six cardinal positions (highlighted green), primary position (pink circle), elevation, and depression, as depicted in Figure 7.
Laws of Ocular Motility
Agonist-Antagonist
These are muscles that move the eye in opposite directions. Agonist is the primary muscle of the eye that moves it in a particular direction. An antagonist is a muscle in the same eye that moves it in the opposite direction.[39] For example – the left medial rectus adducts the eye, and its antagonist’s muscle is the left lateral rectus which abducts the same eye.
Synergist
These are muscles of the same eye that move the eye in the same direction.[21] For example – the left inferior rectus and the left superior oblique are synergists for depression.
Yoke Muscles (Contralateral synergist)
These are pairs of muscles, one in each eye, that produce conjugate eye movements. Example- right superior rectus and left inferior oblique.
Donder’s Law
States that for any gaze direction, the eye’s spatial orientation is unique and independent of previous eye orientation/gaze directions.[40]
Listing’s Law
As per this law, all eye orientations can be achieved starting from a primary eye position. Different gazes can be achieved by moving around the axis within the Listing’s plane.[41]
Hering Law
This is the law of equal innervation. This law states that equal and simultaneous innervation flows to the yoke muscles for conjugate eye movement.[42]
Example – For levoversion, equal and simultaneous innervation is received by the left lateral rectus and right medial rectus. An exception to this law is dissociated vertical or horizontal deviation.
Applied aspects: In patients with paralytic strabismus, an excess innervation is required to fixate with the eye with paralyzed muscle. This leads to a similar concomitant excess supply to the yoke muscle leading to a greater secondary deviation than the primary deviation.
Sherrington’s Law
This is the law of reciprocal innervation. As per this law, the increased innervation to one muscle is accompanied by a reciprocal decrease in innervation to the antagonist’s muscle. For example - during levoversion, there is an increased innervation to the left lateral rectus, accompanied by a simultaneous decrease in innervation received by the left medial rectus.[43] An exception to this law is Duane’s retraction syndrome.
Muscle Orientation
Vertical recti
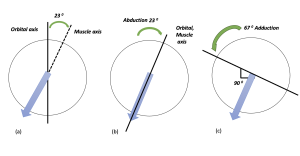
The vertical recti muscles (superior, inferior rectus) form an angle of 23° with the visual axis, as shown in Figure 8. The visual and the orbital axis coincide once the eye is 23° abducted. The eye has no subsidiary actions in this gaze, and recti muscles act as pure elevator/ depressor. Once the eye is 67° adducted, the visual axis forms an angle of 90° with the orbital axis. In this position, the recti muscles act as pure torsional muscles.[12]
Oblique muscles
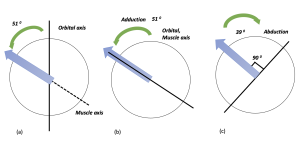
The oblique muscles form an angle of 51°with the visual axis, as shown in Figure 9. When the globe is 51° adducted, the visual and the orbital axis align, and the oblique muscles act as pure elevators/depressors. In 39° abduction, the visual axis and the orbital axis are at 90° to each other, and the oblique muscles work as pure torsional muscles.[44]
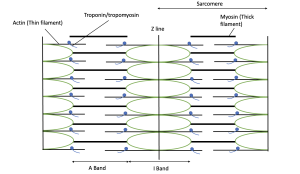
Extraocular Muscle Microscopy in Normal Eyes
The extraocular muscle fibers are skeletal muscles that histologically show tight and normally arranged striations. The transmission electron microscopy consists of skeletal muscle fibers with intact basal membrane and sarcolemma, tightly aligned myofibrils with well-arranged sarcomeres, Z line, and H zone, along with normal distribution of mitochondria.[45] These are depicted in Figure 10.
Extraocular Muscle Microscopy in Strabismic Eyes
Martinez et al. studied the myofibrillar structure in the strabismic eyes and found marked variations in muscle fiber shape and size.[46] They also noted small, hypertrophied, whorled, ringbiden fibers in the myofibrils. Sarcomere disruption was also reported in 2-3mm sections. Ultrastructural features revealed vacuoles within myofilament bundles, smearing of Z bands, and nemaline rods. They also found abnormal mitochondria and “Zebra” or “Striated” foreign bodies in a few extraocular muscles. Falki et al. also reported the skeletal muscle fibers to be disarranged, atrophied, swollen, or disintegrated in strabismic patients.[47] Electron microscopy revealed vacuolation and degenerated myofibrils, lipid droplet accumulation, and clustered mitochondria in strabismic eyes.
Developmental Anomalies of Extraocular Muscles
Congenital Absence of Muscle
These patients may present mimicking muscle paralysis. It is difficult to differentiate and diagnose the absence of muscle pre-operatively and comes as a surprise intraoperatively.[48] Surgeons should be prepared with alternative surgical procedures in such cases. These have been more commonly reported in patients with craniofacial dysostosis.[49][50]
Accessory Extraocular Muscle
Three different types of accessory extraocular muscles have been reported in the literature. These include anomalous muscle bands bridging two muscles, fibrous tissues adjacent to muscles that attach to the globe, and muscles arising from posterior orbit and inserting on globe or extraocular muscles.[51] Wahl proposed that these fibromuscular tissue bands represent atavistic retractor bulbi muscles.[52] Dobbs et al reported a case of large exotropia with Gorlin syndrome who was found to have bilateral anomalous extraocular muscles inferolateral to the optic nerves.[53]
Fascial Sheath Anomalies
This is more common. The fascial sheath acts as a check for active and passive movements of the globe. Anomaly of the fascial sheaths may lead to ocular movement abnormality even with normal anatomical and functional muscles. Examples include the Tendon sheath syndrome of Brown syndrome.[54]
Clinical Relevance
Cranial Nerve Palsies
The extraocular muscles receive innervation from three cranial nerves, including the oculomotor, trochlear, and abducens. Damage to extraocular muscles or their innervation can affect ocular motility, resulting in altered ocular alignment or binocular double vision.[55]
Oculomotor Nerve Palsy
An insult to the oculomotor nerve affects most of the extraocular muscles. The patient typically presents with a dropping of the lid, along with the limitation of adduction, elevation, and depression to varying degrees. The eye assumes a down-and-out position, secondary to functional lateral rectus (abduction) and superior oblique (depression).[56][57]
Trochlear Nerve Palsy
An insult to the trochlear nerve that paralyzes the superior oblique muscle. Examination fails to reveal any noticeable difference in the resting position of the eyeballs. Careful slit lamp examination often reveals a limited intorsion. The patient often complains of binocular double vision, which is more troublesome in the downgaze. There is usually an associated head tilt away from the site of the lesion.[58] [59]
Abducens Nerve Palsy
An insult to the abducens nerve paralyzes the abducens muscles. The affected muscle rests in adduction because of the effect of the medial rectus muscle. The patient presents with a face turn towards the side of the affected muscle. Multiple cases have been reported secondary to giant cell arthritis, trauma, and post-COVID-19 vaccination.[60][61] Recently a case of bilateral sixth nerve palsy with subdural hematoma was reported secondary to vitamin B12 deficiency.[62]
Strabismus
Strabismus often referred to as crossed eyes or lazy eye, is abnormal alignment of both eyes. This can occur secondary to defects in extraocular muscles or due to defects in their neurological control. Different types of deviations can be esotropia (crossed eyes), exotropia (wall eyed), vertical deviations (hyper- or hypotropia). A customized surgical approach to correct the misalignments include weakening or strengthening procedures. Few latest modifications include the transposition, or transplantation of muscles to correct the ocular misalignment.[63] [64]
Muscle strengthening procedures include resection, advancement, plication or muscle tucking.[65] Figure 11 shows intraoperative resection of medial rectus in a patient with exotropia.
Muscle weakening procedures include recession, myotomy, myectomy, dissinsertion or denervation.[66] Figure 12 shows intraoperative recession of lateral rectus muscle.
Horner Syndrome
Horner syndrome refers to the triad of symptoms resulting from damage to the sympathetic trunk in the neck. Horner syndrome can occur secondary to a tumor of the apex of the lung (Pancoast tumor), aortic aneurysm, or thyroid carcinoma.[67] The classical triad consists of the following:
Partial ptosis - Secondary to denervation of the superior tarsus muscle.
Miosis - Secondary to denervation of the dilator pupillae muscle.
Ipsilateral anhidrosis - Secondary to denervation of the sweat glands.
Additional Resources
References
- ↑ 1.0 1.1 Haładaj R. Normal Anatomy and Anomalies of the Rectus Extraocular Muscles in Human: A Review of the Recent Data and Findings. Biomed Res Int. 2019;2019:8909162. Published 2019 Dec 28. doi:10.1155/2019/8909162
- ↑ Bohnsack BL, Gallina D, Thompson H, et al. Development of extraocular muscles requires early signals from periocular neural crest and the developing eye. Arch Ophthalmol. 2011;129(8):1030-1041. doi:10.1001/archophthalmol.2011.75
- ↑ Noden DM, Trainor PA. Relations and interactions between cranial mesoderm and neural crest populations. J Anat. 2005;207(5):575-601. doi:10.1111/j.1469-7580.2005.00473.x
- ↑ Bohnsack BL, Gallina D, Thompson H, et al. Development of extraocular muscles requires early signals from periocular neural crest and the developing eye. Arch Ophthalmol. 2011;129(8):1030-1041. doi:10.1001/archophthalmol.2011.75
- ↑ 5.0 5.1 Shumway CL, Motlagh M, Wade M. Anatomy, Head and Neck, Eye Extraocular Muscles. In: StatPearls. Treasure Island (FL): StatPearls Publishing; October 13, 2022.
- ↑ Gupta N, Motlagh M, Singh G. Anatomy, Head and Neck, Eye Arteries. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 25, 2022.
- ↑ Azzam D, Cypen S, Tao J. Anatomy, Head and Neck: Eye Ophthalmic Vein. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 25, 2022.
- ↑ Olitsky SE, Coats DK. Complications of Strabismus Surgery. Middle East Afr J Ophthalmol. 2015;22(3):271-278. doi:10.4103/0974-9233.159692
- ↑ Joyce C, Le PH, Peterson DC. Neuroanatomy, Cranial Nerve 3 (Oculomotor). In: StatPearls. Treasure Island (FL): StatPearls Publishing; March 28, 2022.
- ↑ Zanganeh T, Legault GL. Extraocular Muscle Management With Orbital and Globe Trauma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 15, 2022.
- ↑ Lacey H, Oliphant H, Smith C, Koenig M, Rajak S. Topographical anatomy of the annulus of Zinn. Sci Rep. 2022;12(1):1064. Published 2022 Jan 20. doi:10.1038/s41598-022-05178-y
- ↑ 12.0 12.1 Shumway CL, Motlagh M, Wade M. Anatomy, Head and Neck: Eye Superior Rectus Muscle. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 30, 2022.
- ↑ Ma C, Zhu X, Chu X, et al. Formation and Fixation of the Annulus of Zinn and Relation With Extraocular Muscles: A Plastinated Histologic Study and Its Clinical Significance. Invest Ophthalmol Vis Sci. 2022;63(12):16. doi:10.1167/iovs.63.12.16
- ↑ Kim SY, Motlagh M, Naqvi IA. Neuroanatomy, Cranial Nerve 4 (Trochlear). In: StatPearls. Treasure Island (FL): StatPearls Publishing; November 7, 2022.
- ↑ Wong AM. Listing's law: clinical significance and implications for neural control. Surv Ophthalmol. 2004;49(6):563-575. doi:10.1016/j.survophthal.2004.08.002
- ↑ Demer JL, Clark RA, Crane BT, Tian JR, Narasimhan A, Karim S. Functional anatomy of the extraocular muscles during vergence. Prog Brain Res. 2008;171:21-28. doi:10.1016/S0079-6123(08)00604-3
- ↑ Lenart TD, Lambert SR. Slipped and lost extraocular muscles. Ophthalmol Clin North Am. 2001;14(3):433-442. doi:10.1016/s0896-1549(05)70241-8
- ↑ Modi P, Arsiwalla T. Cranial Nerve III Palsy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 4, 2022.
- ↑ Lenart TD, Lambert SR. Slipped and lost extraocular muscles. Ophthalmol Clin North Am. 2001;14(3):433-442. doi:10.1016/s0896-1549(05)70241-8
- ↑ Athavale S, Kotgirwar S, Lalwani R. Rectus and oblique muscles of eyeball: a morphometric study of Indian population. Anat Cell Biol. 2015;48(3):201-204. doi:10.5115/acb.2015.48.3.201
- ↑ 21.0 21.1 Helveston EM, Alcorn DM, Ellis FD. Inferior oblique inclusion after lateral rectus surgery. Graefes Arch Clin Exp Ophthalmol. 1988;226(2):102-105. doi:10.1007/BF02173291
- ↑ Knight B, Lopez MJ, Patel BC. Anatomy, Head and Neck: Eye Levator Palpebrae Superioris Muscles. In: StatPearls. Treasure Island (FL): StatPearls Publishing; March 17, 2023.
- ↑ 23.0 23.1 Pacheco EM, Guyton DL, Repka MX. Changes in eyelid position accompanying vertical rectus muscle surgery and prevention of lower lid retraction with adjustable surgery. J Pediatr Ophthalmol Strabismus. 1992;29(5):265-272. doi:10.3928/0191-3913-19920901-03
- ↑ Gupta N, Patel BC. Anatomy, Head and Neck: Eye Inferior Oblique Muscles. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 25, 2022.
- ↑ Lieber S, Fernandez-Miranda JC. Anatomy of the Orbit. J Neurol Surg B Skull Base. 2020;81(4):319-332. doi:10.1055/s-0040-1715096
- ↑ Khanam S, Sood G. Trochlear Nerve Palsy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 27, 2023.
- ↑ Qin T, Chun P, Li FF, Yu SB, Hwang K, Sui HJ. Medial and lateral canthal ligaments shown in P45 sheet plastination and dissection. Indian J Ophthalmol. 2021;69(5):1150-1154. doi:10.4103/ijo.IJO_2848_20
- ↑ Zhuang W, Fang S, Fan H, et al. Anatomical study of the extraocular check ligament system. J Plast Reconstr Aesthet Surg. 2019;72(12):2017-2026. doi:10.1016/j.bjps.2019.09.002
- ↑ Ozsoy E, Gunduz A, Ozturk E. Inferior Oblique Muscle Overaction: Clinical Features and Surgical Management. J Ophthalmol. 2019;2019:9713189. Published 2019 Jul 17. doi:10.1155/2019/9713189
- ↑ Shumway CL, Motlagh M, Wade M. Anatomy, Head and Neck, Orbit Bones. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 25, 2022.
- ↑ Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003;27(3):193-204. doi:10.1007/s00266-003-0127-5
- ↑ Haładaj R. Normal Anatomy and Anomalies of the Rectus Extraocular Muscles in Human: A Review of the Recent Data and Findings. Biomed Res Int. 2019;2019:8909162. Published 2019 Dec 28. doi:10.1155/2019/8909162
- ↑ Kushner BJ. How do recessions and resections of extraocular muscles work?. J AAPOS. 2006;10(4):291-292. doi:10.1016/j.jaapos.2006.06.001
- ↑ Demer JL, Clark RA. Functional anatomy of extraocular muscles during human vergence compensation of horizontal heterophoria. J Neurophysiol. 2019;122(1):105-117. doi:10.1152/jn.00152.2019
- ↑ van der Steen J, Dits J. Binocular eye movement control and motion perception: what is being tracked?. Invest Ophthalmol Vis Sci. 2012;53(11):7268-7275. Published 2012 Oct 19. doi:10.1167/iovs.12-9809
- ↑ Hess BJ, Thomassen JS. Kinematics of visually-guided eye movements. PLoS One. 2014;9(4):e95234. Published 2014 Apr 21. doi:10.1371/journal.pone.0095234
- ↑ Moon Y, Lee WJ, Shin SH, et al. Positional Change of the Eyeball During Eye Movements: Evidence of Translatory Movement. Front Neurol. 2020;11:556441. Published 2020 Sep 17. doi:10.3389/fneur.2020.556441
- ↑ Nguyen JD, Duong H. Anatomy, Head and Neck: Eye Nerves. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 25, 2022.
- ↑ Demer JL. Current concepts of mechanical and neural factors in ocular motility. Curr Opin Neurol. 2006;19(1):4-13. doi:10.1097/01.wco.0000198100.87670.37
- ↑ Crawford JD, Ceylan MZ, Klier EM, Guitton D. Three-dimensional eye-head coordination during gaze saccades in the primate. J Neurophysiol. 1999;81(4):1760-1782. doi:10.1152/jn.1999.81.4.1760.
- ↑ Crawford JD, Vilis T. Axes of eye rotation and Listing's law during rotations of the head. J Neurophysiol. 1991;65(3):407-423. doi:10.1152/jn.1991.65.3.407
- ↑ King WM. Binocular coordination of eye movements--Hering's Law of equal innervation or uniocular control?. Eur J Neurosci. 2011;33(11):2139-2146. doi:10.1111/j.1460-9568.2011.07695.x
- ↑ Gonzalez C, Chen HH, Ahmadi MA. Sherrington innervational surgery in the treatment of chronic sixth nerve paresis. Binocul Vis Strabismus Q. 2005;20(3):159-166.
- ↑ Demer JL. Current concepts of mechanical and neural factors in ocular motility. Curr Opin Neurol. 2006;19(1):4-13. doi:10.1097/01.wco.0000198100.87670.37
- ↑ Gillies AR, Lieber RL. Structure and function of the skeletal muscle extracellular matrix. Muscle Nerve. 2011;44(3):318-331. doi:10.1002/mus.22094
- ↑ Martinez AJ, Hay S, McNeer KW. Extraocular muscles: light microscopy and ultrastructural features. Acta Neuropathol. 1976;34(3):237-253. doi:10.1007/BF00688678
- ↑ Al-Falki Y, Al-Shraim M, Alsabaani NA, Eid RA, Radad K. Ultrastructural changes of extraocular muscles in strabismus patients. Ultrastruct Pathol. 2019;43(4-5):145-153. doi:10.1080/01913123.2019.1671927
- ↑ Astle W. F., Hill V. E., Ells A. L., Chi N. T. T., Martinovic E. Congenital absence of the inferior rectus muscle-diagnosis and management. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2003;7(5):339–344. doi: 10.1016/s1091-8531(03)00214-3.
- ↑ Law G., Khan H. M., Lyons C. J., Anderson D. P. Unilateral absence of the superior rectus muscle: an unusually delayed presentation. Canadian Journal of Ophthalmology. 2019;54(6):e297–e300. doi: 10.1016/j.jcjo.2019.03.010.
- ↑ Cuttone J. M., Brazis P. J., Miller M. T., Folk E. R. Absence of the superior rectus muscle in Apert’s syndrome. Journal of Pediatric Ophthalmology and Strabismus. 1979;16(6):349–354.
- ↑ Djordjevic B., Novakovic M., Milisavljevic M., Milicevic S., Malikovic A. Surgical anatomy and histology of the levator palpebrae superioris muscle for blepharoptosis correction. Vojnosanitetski Pregled. 2013;70(12):1124–1131. doi: 10.2298/vsp1312124d.
- ↑ Wahl L, Lee R, Olewnik Ł, et al. Atavistic muscles in human anatomy: Evolutionary origins and clinical implications. Anat Histol Embryol. 2022;51(3):321-331. doi:10.1111/ahe.12796
- ↑ Dobbs MD, Mawn LA, Donahue SP. Anomalous extraocular muscles with strabismus. AJNR Am J Neuroradiol. 2011;32(9):E167-E168. doi:10.3174/ajnr.A2291
- ↑ Olusanya BA. Brown syndrome with severe amblyopia: a case report from Africa. Pan Afr Med J. 2015;20:56. Published 2015 Jan 21. doi:10.11604/pamj.2015.20.56.6050
- ↑ Sanders RD. Cranial Nerves III, IV, and VI: Oculomotor Function. Psychiatry (Edgmont). 2009;6(11):34-39.
- ↑ Kanazawa T, Hino U, Kuramae T, Ishihara M. Idiopathic unilateral oculomotor nerve palsy: A case report. Heliyon. 2020;6(12):e05651. Published 2020 Dec 3. doi:10.1016/j.heliyon.2020.e05651
- ↑ Singh RB, Shergill S, Singh KP, Thakur S. Down and out: acquired oculomotor nerve palsy. BMJ Case Rep. 2019;12(8):e231485. Published 2019 Aug 21. doi:10.1136/bcr-2019-231485
- ↑ Chen WC, Li YS, Huang P. Isolated trochlear palsy as the only presentation of midbrain infarction: a case report. J Int Med Res. 2021;49(4):3000605211008292. doi:10.1177/03000605211008292
- ↑ Hayashi T, Nomura K, Nishiyama Y, Kimura K. Unilateral Isolated Trochlear Nerve Palsy due to Ipsilateral Midbrain Infarction. J Nippon Med Sch. 2021;88(6):561-563. doi:10.1272/jnms.JNMS.2021_88-515
- ↑ Colquhoun M, Alegre Abarrategui J, Shahzad MI, Ellis B. Giant cell arteritis presenting with unilateral sixth nerve palsy. BMJ Case Rep. 2023;16(5):e253484. Published 2023 May 23. doi:10.1136/bcr-2022-253484
- ↑ Kalita IR, Singh HV, Sharma S. Acute abducens nerve palsy with acute disseminated encephalomyelitis-like presentation following COVID-19 vaccination. Indian J Ophthalmol. 2023;71(5):2279-2281. doi:10.4103/ijo.IJO_1778_22
- ↑ Krishna G, Singh M, Gill BS, Kumar V, Aggarwal VK, Singh I. Bilateral sixth nerve palsy with subdural hematoma: a unique presentation of B12 deficiency [published online ahead of print, 2023 May 20]. Childs Nerv Syst. 2023;10.1007/s00381-023-05996-z. doi:10.1007/s00381-023-05996-z
- ↑ Akbari MR, Masoomian B, Mirmohammadsadeghi A, Sadeghi M. A Review of Transposition Techniques for Treatment of Complete Abducens Nerve Palsy. J Curr Ophthalmol. 2021;33(3):236-246. Published 2021 Oct 22. doi:10.4103/joco.joco_42_21
- ↑ Jethani JN, Shah N, Amin S, Jethani M. Stability and effects of muscle transplantation for very large angle esotropia: A study of 22 patients. Indian J Ophthalmol. 2017;65(7):607-609. doi:10.4103/ijo.IJO_54_17
- ↑ Daga D, Pujari A, Sharma P, Phuljhele S, Saxena R. Evaluation of reinforced plication as an alternative to resection in exotropia. Indian J Ophthalmol. 2022;70(3):948-951. doi:10.4103/ijo.IJO_2884_20
- ↑ Aghdam KA, Asadi R, Sanjari MS, Sadeghi A, Razavi M. Comparing Two Inferior Oblique Weakening Procedures: Disinsertion versus Myectomy. J Ophthalmic Vis Res. 2021;16(2):212-218. Published 2021 Apr 29. doi:10.18502/jovr.v16i2.9085
- ↑ Kanagalingam S, Miller NR. Horner syndrome: clinical perspectives. Eye Brain. 2015;7:35-46. Published 2015 Apr 10. doi:10.2147/EB.S63633