Examination Techniques for Lower Eyelid Malposition
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
What constitutes lower eyelid malposition?
Ectropion [1]
- Mechanical: mass, tumor, edema, herniated fat
- Paralysis from facial nerve palsy
- Cicatricial scarring and shortening of the anterior lamella
- Chronic sun exposure
- Involutional changes
- Congenital
Entropion [2]
- Acute spastic entropion from infection, irritation and inflammation
- Tarsoconjunctival contracture
- Cicatricial from burns, trauma, infection, or inflammation
- Involutional changes
- Eyelid Myokymia
- Congenital
Lid Retraction [3]
- Thyroid eye disease
- Cicatricial
- Over-excision during eyelid blepharoplasty
Anatomy of the Lower Eyelid
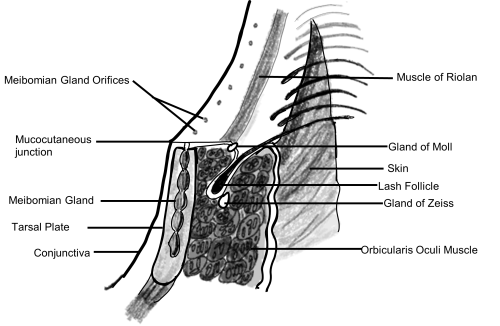
Understanding the anatomy and physiology of the lower eyelid is essential for providing safe and successful cosmetic or reconstructive surgery. The lower eyelid is divided into three lamellae: anterior, middle, and posterior. The anterior lamella is composed of the skin and orbicularis oculi muscle. The middle lamella comprises the orbital septum and the post-septal fat. Lastly, the posterior lamella consists of the tarsal plate, conjunctiva, and the lower lid retractors.[4]
The orbicularis oculi muscle is divided into two parts: the outer orbital portion and the inner palpebral portion. The palpebral part can be further divided into pre-tarsal and pre-septal components. The upper and lower pre-tarsal components are joined medially, making up the medial canthal tendon as they insert onto the lacrimal crest. Lateral components of pretarsal orbicularis inserts onto Whitnall’s tubercle, 3 to 4 mm posterior to the lateral orbital rim, forming the lateral canthal tendon. [5]
The skin of the lower eyelid is less than 1 mm in thickness and lacks subcutaneous fatty layers. The skin is anchored to the orbicularis oculi by delicate connective tissue attachments.
The lower eyelid has three fat pads behind the orbital septum within the orbital cavity: medial, central, and lateral. One important anatomical marker to identify and preserve is the inferior oblique muscle located in between the medial and central fat pads. The medial fat pad contains denser fat, which gives distinct characteristics from the other fat pads.[5]
Orbital Vectors
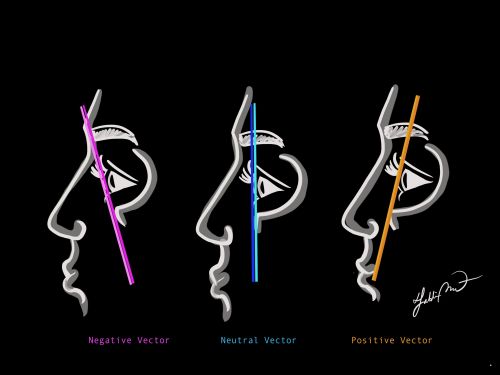
The orbital vector is an imaginary line that denotes the relationship between the corneal apex and the malar eminence.[6] A neutral orbital vector is when the corneal apex and the malar eminence align in a vertical plane. When the corneal apex projects more anteriorly than the position of the malar eminence, it is considered a negative vector. On the contrary, a positive orbital vector is when the malar eminence projects more anterior to the corneal apex.
Patients with negative orbital vectors have been shown to be more correlated with the development of ectropion, while those with positive vectors are more likely to develop an entropion.[7] An important complication to take into consideration is that patients with negative vectors can develop bowstringing of the globe from over-tightening of the lower lid and excess skin excision, leading to a higher incidence of lower lid malposition.[8]
The effect of aging on lower eyelid malposition
The changes in the fat pads and the complex lower-eyelid anatomy contribute significantly to the appearance of aging in the face. For instance, the medial and lateral canthal tendons become weakened with aging and result in lower-lid laxity.[9] Additionally, the aging process of the lower eyelid could be manifested with clinical features, including dermatochalasis, fat prolapse, and a change in orbicularis oculi muscle tone.
With aging, the facial skeleton is noted to remodel and rotate in a way that the frontal bone moves anteriorly and inferiorly, and the maxilla moves posteriorly and superiorly. These changes were predicted to decrease the distance of globe-to-orbital roof and increase the distance of globe-to-orbital floor measurements. This rotation results in the bony angle becoming more acute, affecting the position of overlying soft tissues. This rotation causes an increased downward vector on the lower eyelid. Furthermore, the inferior orbital rim was noted to be displaced more inferiorly and posteriorly in aging patients, which may place tension inferiorly on the lower eyelid. These structural changes in aging could lead to increased scleral show, lateral canthal tendon laxity, and ectropion and entropion pathogenesis.[10]
Targeted Physical Examination for Proper Evaluation Lower Eyelid Malposition
- Hertel Exophthalmometer
- MRD2 (Margin to Reflex Distance 2)
- Punctal position (inverted, everted, apposition)
- Snapback Test
- Pinch Test
- Eyelid Distraction Test (Medial distraction test, lateral distraction test)
- Orbicularis Muscle Strength test
- Size of the tear lake
- Presence or Absence of Trichiasis
- Ocular surface examination
Physical Examination Techniques
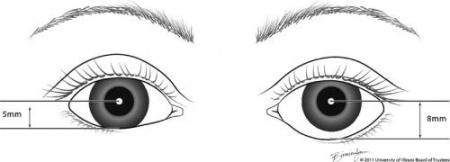
Hertel Exophthalmometer
Purpose
- Bony morphology affects the overlying soft tissue and lid. Patients with certain bony morphologies, such as a condition that causes a negative orbital vector, are at an increased risk for post-operative lower eyelid malposition[10].
- The Hertel exophthalmometer is used to measure the relationship between the lateral orbital rim and the apex of the cornea.
How to perform
- This device is composed of a horizontal calibrated bar with carriers holding sliding mirrors and scale reading at both ends. The mirrors are inclined at 45 degrees to enable visualization of both the scale reading and the apex of the cornea. Notches at the front of the carriers that hold the mirrors are placed on the bony part of the lateral orbital rim of a patient. While the patient is looking straight and fixated on a point, the examiner can visualize and measure the apex of the cornea by using the millimeter scale reading aligned with the eye in the carrier. The measurement of the patient’s right eye should be done with the examiner’s left eye and vice versa.
- Additionally, the distance on the horizontal bar is recorded as the baseline measurement for the distance of the bilateral lateral orbital rims, which can be used for future comparisons and measurement consistency.[11]
Interpretation
- The normal range is 12-21 mm, however interpreting the measurement should be done with caution as it can vary with different racial and age groups.[12]
- If a patient has injury to their lateral orbital rim, then the Hertel measurement will be unreliable and a Naugle exophthalmometer should be used instead which relies on the superior and inferior orbital rim.
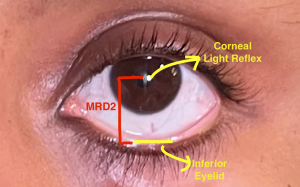
Margin to Reflex Distance 2 (MRD2)
Purpose
- The margin reflex distance 2 (MRD2) is a useful measurement in determining the amount of lower lid retraction.[13]
How to perform
- The examiner aligns their eyes on the same plane as the patient’s eyes. A muscle light is held between the examiner’s eyes and is directed at the patient’s eyes, inducing the corneal light reflex. The eyebrows should be maintained in a neutral position. The distance between the light reflex and the central portion of the lower eyelid is measured.
Interpretation
- The amount of unilateral retraction is calculated by subtracting the MRD2 of the abnormal eyelid from the MRD2 of the normal eyelid. In bilateral retraction, the amount of retraction is calculated by subtracting the MRD2 from 5.5 mm (the normal MRD2).
- The MRD1 plus the MRD2 should equal the palpebral fissure width.
Punctal Position
Purpose of evaluation
- Lacrimal puncta are small openings located at the nasal end of the palpebral margin of the eyelids. Due to its association with the lower eyelid, the position of the lacrimal puncta could be used to evaluate the position of the lower eyelid.[14]
Interpretation
- The normal punctum on the lower lid is found positing backward in the medial tear lake which is termed appositional punctal position. Slight changes in punctal position could indicate an early sign of lower eyelid disease. For instance, the lower punctum can be seen pointing inwards (punctal entropion) or outwards (punctal ectropion) under a biomicroscope in early lower eyelid laxity and ectropion, even if the position of the lower eyelid appears to be normal on examination.[14]
Snapback Test
Purpose
- The Snapback test is a technique used to grade lower lid laxity, allowing one to test the tone of the orbicularis oculi muscle.
How to perform
- The middle portion of the lower eyelid is pulled inferiorly away from the globe until the lid is fully displaced. After releasing the lid, it should immediately return to contact the globe in a healthy lower eyelid.
Interpretation
The grading scale depends on how long the lower lid takes to spring back into the globe.
- Grade 0: takes less than 2 seconds
- Grade I: takes 2 or 3 seconds
- Grade II: takes 4 or 5 seconds
- Grade III: takes more than 5 seconds but returns to its normal position with blinking
- Grade IV: never returns back to the normal position
Pinch Test
Purpose
This test is used to evaluate the generalized laxity of the skin only of the lower eyelid.
How to perform
- The examiner instructs the patient to look up with an open mouth. The skin of the lower eyelid below the lashes is grasped using either smooth forceps or the fingers of the examiner. The distance the lid can be distracted from the globe is then measured.
Interpretation
- A healthy lid will not distract more than 6 mm from the globe.
Lid Distraction Test:
Purpose
The lid distraction test is used to assess the eyelid laxity of both the medial and lateral canthal tendon.
How to perform
Medial distraction test is used to assess the laxity of the lateral canthal tendon by pulling the canthus medially along a horizontal line until it is no longer pulled. Lateral distraction test is used to assess the laxity of the medial canthal tendon by pulling the canthus laterally along a horizontal line until it is no longer pulled.[15]
Interpretation
There is no universally approved grading, scale, or guideline for lid distraction test to quantify the laxity. It is commonly recorded as being present if the displacement is more than 1 to 3 mm or absent. Few studies have been done to create a grading system for lateral distraction test to quantify the laxity of the medial canthal tendon. In 2001, Olver et al. described a simple grading system for measuring medial canthal tendon laxity in relation to a constant ocular landmark. [16]
The distracted position of the lower punctum was visually graded from its resting position ranging from grade 1 to 6 in relation to the plica semilunaris (grade 0), medial corneal limbus (grade 2), and the mid pupil (grade 4).
They additionally provided a guideline for appropriate surgical intervention based on grading: For grades 0-1, no surgery was indicated, and a medial canthal tendon stabilization suture may be indicated for grade 3 or 4 laxity.[16] Another study used a grading system based on the distance of displacement in mm. Fante and Elner classified laxity as normal in 0 to 2 mm of lateral distraction, mild laxity as 2 to 4 mm lateral distraction, moderate laxity as 4 to 6 mm, and lastly severe if greater than 6 mm laxity.[17]
Orbicularis Muscle Strength Test
Purpose
As the name describes, the orbicularis muscle strength test is performed to assess how strong the orbicularis muscle can contract.
How to perform
The subject is asked to close their eyes. The observer gently places the index finger on the subject’s upper lid and the thumb on the lower lid. Then, the subject is instructed to squeeze their eyes closed as tightly as possible while the observer tries to spread their index and thumb on the eyelids to open the eye. While the subject is resisting the force of opening by squeezing their orbicularis muscle, the observer feels how much effort needs to be put in to open their eyes.[18]
Interpretation
The strength of orbicularis muscle can be graded from 0 to 4. This grading has been shown to be useful when planning and monitoring botulinum toxin treatment for blepharospasm and hemifacial spasm.[19]
- Grade 0: incomplete eye closure.
- Grade 1: Lids are minimally closed with minimal resistance to overcome.
- Grade 2: lids are closed well with some resistance but can be easily overcome.
- Grade 3: Strong closure with moderate resistance.
- Grade 4: Very strong lid disclosure with very strong resistance that is extremely difficult to overcome.
Size of Tear Lake
Purpose
The tear lake is a collection of tears below the conjunctival sac, and its size can be measured in volume (uL) pooled in the conjunctival sac or height (mm) of the tear exposed from the eyelid margin, which is more commonly known as the tear meniscus height (TMH). The primary purpose of this test is to diagnose and evaluate the severity of dry eye, however it could be used to assess the laxity of the lower eyelid.[20][21] In a study by Yokoyama et al, TMH was also used to monitor tear drainage after correction of horizontal laxity in involutional lower eyelid entropion.[22]
How to perform
The volume of the tear can be measured with the Schirmer test and Strip meniscometry.[23] The TMH can be measured with a slit lamp microscope and optical coherence tomography (OCT), which has been shown to be the most reliable method to measure TMH.[24]
Interpretation
- The normal average test value for the Schirmer test ranges from 8 mm to 33 mm, but the accepted normal value is greater than 10 mm.
- TMH of a normal patient has a height of 0.2 to 0.5 mm, and less than 0.2 indicates dry eye.[25]
- As people age and their eyelids become loose, the size and volume of the tear lake is expected to get larger, which may lead to dry eye due to incomplete closure of eyelids.
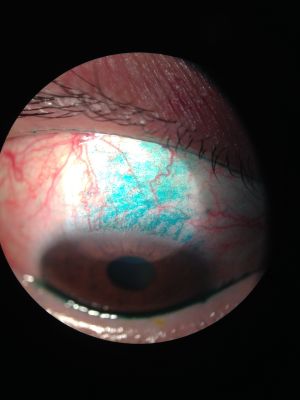
Ocular Surface Assessment
Purpose
Examining the ocular surface allows the examiner to closely assess the lid margins, lashes, surface, glandular corneal epithelium, meibomian glands, lacrimal gland, accessory lacrimal glands, and nasolacrimal duct. By doing so, dysfunction of or injury to any of the structures of the ocular surface, which can lead to cicatrizing disease, blepharitis, and dry eye, can be diagnosed.[26]
Ocular surface assessment is usually done using a slit lamp biomicroscopy with special dyes such as Fluorescein, Lissamine green, and Rose Bengal.
How to perform
Slit lamp examination with dyes can be performed in several ways. The first method is that the dyes can come in a vial and can be directly dropped onto the surface of the eye. The other method is done by applying the dye with normal saline to a strip, which can be gently placed onto the inferior palpebral conjunctiva while the patient is looking up.[27] After asking the patient to blink several times to spread the dye over the corneal surface evenly, the ocular surface can be examined using the slit lamp.
There are three different types of dyes that are specifically used to examine the ocular surface.
- Fluorescein dye can be used to produce a green visual contrast for epithelial injury opposed to a healthy blue epithelial background. This can indicate any corneal conditions, including corneal abrasion, epithelial keratitis, herpes simplex keratitis, or corneal foreign bodies. In the presence of a break in the corneal epithelium, aqueous humor leaks and mixes with the fluorescein dye to highlight areas of epithelium breakdown in yellow-green.[28]
- Lissamine green makes an ideal dye for the bulbar conjunctiva by staining degenerated cells where disruption or damage of mucin coating is present.
- Rose Bengal acts similar to lissamine green by staining dead and damaged cells. This dye has been used less frequently due to a finding that it can also stain normal, healthy living cells and cellular toxicity. Rose bengal can be used to evaluate for numerous ocular pathologies, including herpetic corneal epithelial dendrites, superficial punctate keratitis, meibomian gland dysfunction, and dysplastic cells of conjunctival squamous neoplasms.[29]
Interpretation
Ocular surface findings will greatly vary among various ocular surface diseases. If there is impairment in the lids causing incomplete closure of the eye, staining would typically show up around the inferior of the cornea as it is getting damaged from consequent dry eye. Some possibilities why one may find staining in the superior of the cornea are a foreign body, trichiasis, floppy lid syndrome, superior limbic keratitis, blepharitis, conjunctival concretions, vernal keratoconjunctivitis, and superior entropion.[30]
- ↑ Ozgur O, Kaufman EJ. Ectropion. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441929/
- ↑ Bergstrom R, Czyz CN. Entropion. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470352/
- ↑ Nerad, J.A., Carter, K.D., Alford, M., Section 5 - Disorders of the Eyelid: Blepharoptosis and Eyelid Retraction. In Oculoplastic and reconstructive Surgery. Mosby; 2008.
- ↑ Labib AM, Patel BC, Milroy C. Lower Eyelid Laxity Examination. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 8, 2023.
- ↑ Jump up to: 5.0 5.1 Jacono AA, Malone MH. Chapter 13: Transcutaneous Lower Blepharoplasty. In: Azizzadeh B, Murphy MR, Johnson CM, Massry GG, Fitzgerald R, eds. Master Techniques in Facial Rejuvenation. 2nd ed. Elsevier; 2018::142-151
- ↑ Garip R, Meriç P, Özveren M, Özveren N. Evaluation of Orbit Vector Relationships in Different Types of Skeletal Malocclusions. Meandros Med Dent J 2022;23:162-167.
- ↑ Rajabi MT, Gholipour F, Ramezani K, Hosseini SS, Rajabi MB, Tabatabaie SZ. The influence of orbital vector on involutional entropion and ectropion. Orbit 2018; 37: 53-8.
- ↑ Lam Kar Wai Phoebe, MD 2017. https://www.jcosmetmed.org/journal/view.html?doi=10.25056/JCM.2017.1.1.1
- ↑ Niamtu J. Chapter 2: The Aging Face. In: Niamtu J, ed. The Art and Science of Facelift Surgery. Elsevier; 2019:6-20.
- ↑ Jump up to: 10.0 10.1 Richard, M.J., et al., Analysis of the anatomic changes of the aging facial skeleton using computer-assisted tomography. Ophthalmic Plast Reconstr Surg, 2009. 25(5): p. 382-6.
- ↑ Stein, H. A., Stein, R. M., & Freeman, M. I. Chapter 10: Understanding ophthalmic equipment. In The ophthalmic assistant: A text for Allied and associated ophthalmic personnel. Elsevier; 2018:114-174
- ↑ Migliori, M.E. and G.J. Gladstone, Determination of the normal range of exophthalmometric values for black and white adults. Am J Ophthalmol, 1984. 98(4): p. 438-42.
- ↑ Putterman AM. Margin reflex distance (MRD) 1, 2, and 3. Ophthalmic Plast Reconstr Surg. 2012;28(4):308-311. doi:10.1097/IOP.0b013e3182523b7f
- ↑ Jump up to: 14.0 14.1 Nadeem N, Patel BC. Punctal Stenosis. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560578/
- ↑ Hou, X., et al., Standardized Three-Dimensional Lateral Distraction Test: Its Reliability to Assess Medial Canthal Tendon Laxity. Aesthetic Plast Surg, 2021. 45(6): p. 2798-2807.
- ↑ Jump up to: 16.0 16.1 Olver, J.M., P.J. Sathia, and M. Wright, Lower eyelid medial canthal tendon laxity grading: an interobserver study of normal subjects. Ophthalmology, 2001. 108(12): p. 2321-5.
- ↑ Fante RG, Elner VM. Transcaruncular approach to medial canthal tendon plication for lower eyelid laxity. Ophthal Plast Reconstr Surg 2001;17:16–27
- ↑ Rahman, R., Berry-Brincat, A. & Thaller, V. A new grading system for assessing orbicularis muscle function. Eye 17, 610–612 (2003). https://doi.org/10.1038/sj.eye.6700444
- ↑ Rahman, R., Berry-Brincat, A. & Thaller, V. A new grading system for assessing orbicularis muscle function. Eye 17, 610–612 (2003). https://doi.org/10.1038/sj.eye.6700444
- ↑ Doughty MJ, Laiquzzaman M, Oblak E, Button N. The tear (lacrimal) meniscus height in human eyes: a useful clinical measure or an unusable variable sign? Cont Lens Anterior Eye. 2002 Jun;25(2):57-65. doi: 10.1016/s1367-0484(01)00005-4. PMID: 16303478
- ↑ Weinberg, D.A., Lower Eyelid Malposition: Evaluation and Treatment. Review of Ophthalmology, 2013. https://www.reviewofophthalmology.com/article/lower-eyelid-malposition-evaluation-and-treatment
- ↑ Yokoyama, T., et al., Changes in Lacrimal Punctum Position and Tear Meniscus Height after Correction of Horizontal Laxity in Involutional Lower Eyelid Entropion. J Ophthalmol, 2023. 2023: p. 4113151.
- ↑ Wang, Y., et al., The Role of Different Tear Volume Detection Methods in the Evaluation and Diagnosis of Mild Dry Eye Disease. Transl Vis Sci Technol, 2022. 11(3): p. 15.
- ↑ Niedernolte, B., et al., Evaluation of tear meniscus height using different clinical methods. Clin Exp Optom, 2021. 104(5): p. 583-588.
- ↑ Zeev, M.S., D.D. Miller, and R. Latkany, Diagnosis of dry eye disease and emerging technologies. Clin Ophthalmol, 2014. 8: p. 581-90.
- ↑ Gipson, I.K., The ocular surface: the challenge to enable and protect vision: the Friedenwald lecture. Invest Ophthalmol Vis Sci, 2007. 48(10): p. 4390; 4391-8.
- ↑ Koh, S., et al., Evaluation of ocular surface and tear function - A review of current approaches for dry eye.Indian J Ophthalmol, 2022. 70(6): p. 1883-1891.
- ↑ Pothen, A.G., Parmer, M. Fluorescein. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555957/
- ↑ Abelson, M.B., Ingerman, A. The Dye-namics of Dry-Eye Diagnosis. Review of Ophthalmology, 2005.https://www.reviewofophthalmology.com/article/the-dye-namics-of-dry-eye-diagnosis
- ↑ Beckman, K., Diagnosing Ocular Surface Disease. Review of Ophthalmology, 2019.https://www.reviewofophthalmology.com/article/diagnosing-ocular-surface-disease