Dilated Superior Ophthalmic Vein in Ophthalmology
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease
Superior ophthalmic vein (SOV) enlargement is a radiographic finding that might be associated with potentially sight- or life-threatening disorders. These include orbital trauma, inflammation, compressive lesions, vascular malformations, and thrombosis [1],[2]. The normal SOV has a mean diameter of 2 millimeters (mm); however, in cases of SOV dilation, the SOV may be greater than or equal to 3.0 mm [1].
Pathology
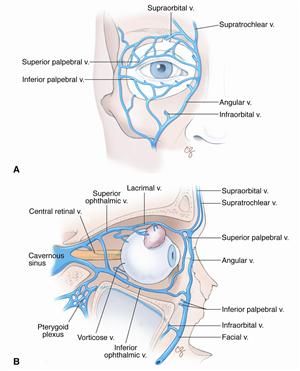
The orbital cavity is drained by the ophthalmic veins with the SOV being the largest in diameter and caliber [3][4]. Originating in the anterior medial orbit from the junction of the supraorbital, supratrochlear, and angular veins, the SOV travels posteriorly to drain into the cavernous sinus [3].
Enlargement of the SOV can be due to alteration in orbital vascular hemodynamics including SOV thrombosis or orbital or cavernous sinus vascular malformations (e.g., arteriovenous malformations (AVM) or dural fistulas). SOV dilation in orbital/cavernous vascular lesions is due to high-pressure retrograde flow with back pressure into the SOV. Impaired venous outflow with congestion from intraluminal obstruction such as SOV thrombosis can also lead to SOV dilation radiographically. External mechanical compression of the SOV and/or orbital vasculature due to a mass or local inflammation (e.g., idiopathic orbital inflammatory syndrome or orbital cellulitis) can also result in SOV dilation. The most common cause of SOV enlargement is a carotid-cavernous sinus fistula or orbital vascular lesion or arteriovenous malformation (AVM) but orbital hemorrhage, thrombosis, orbital lymphoma, thyroid eye disease, and orbital cellulitis are also possible causes [1].
Etiology and Incidence
| Etiologies | Known risk factors reported in the literature | |
|---|---|---|
| Vascular Malformations | Dural- cavernous fistula, carotid-cavernous fistula, orbital AVM, facial AVM | Hypertension, pregnancy, atherosclerotic vascular disease, trauma, hypercholesterolemia, dissection, or spontaneous rupture of a carotid artery aneurysm |
| Hematology | SOV thrombosis, cavernous thrombosis | Myelodysplastic syndrome, chronic myelomonocytic leukemia, systemic lupus erythematous, orbital cellulitis, suprasellar meningioma, multiple abscesses, sinusitis, Factor V Leiden |
| Traumatic hemorrhage | Intracranial hemorrhage, orbital hemorrhage | Trauma |
| Systemic/Inflammatory | Thyroid eye disease, idiopathic orbital inflammation | Superior rectus myositis, Tolosa-Hunt syndrome, Graves Disease |
| Malignancy | Orbital lymphoma, Para-sellar meningioma, orbital pseudotumor | |
| Infectious | Orbital cellulitis | |
| Other | Increased intracranial pressure | Intubation |
Dilated SOV is most commonly found in vascular malformations including dural-cavernous fistula or carotid-cavernous fistula (CCF), and orbital or facial AVM [1]. AVMs can prove fatal as the pressure of the high-arterial flow can damage venous wall integrity [7]. Although brain AVM origins are unclear, they are assumed to be a developmental abnormality [8][9]. SOV thrombosis can be idiopathic (primary) or secondary to hypercoagulable state, myelodysplastic syndrome, chronic myelomonocytic leukemia, systemic lupus erythematosus (SLE), orbital cellulitis, or compressive lesions (e.g., meningioma) [1].
Epidemiology
Adam et al. reported on 113 patients with SOV dilation, 66% were women with a mean age of 49 +/- 24 years (range 0.4 – 90 years) [1]. The epidemiology of SOV enlargement is most related to the underlying etiology.
Diagnosis
History and Physical
Patients with SOV dilation radiographically (CT or MRI) can produce orbital and ocular symptoms and signs due to high-pressure orbital retrograde flow or impaired venous outflow and venous congestion [1]. Common symptoms include decreased vision, diplopia, periorbital swelling, pulsatile tinnitus, headache, eye redness, eye pain, tearing, oral/nasal bleeding, nausea, and vomiting. On exam, depending on the etiology of disease, findings could show ophthalmoplegia, periorbital swelling, conjunctival injection, chemosis, proptosis, ptosis, and decreased visual acuity [1].
Imaging
Imaging modalities utilized to diagnose SOV dilation include magnetic resonance imaging (MRI), magnetic resonance (MR) angiography, computed tomography (CT), and ultrasound [1],[10][11]. Coronal T2 weighted MRI is the most common approach for recognizing the 3D architecture of the SOV as a report in 2015 by Tsutsumi et al. detected the SOV in 100% of the cases [11]. Additional imaging using CT, DSA, and ultrasound were commonly used to further characterize the vasculature. The conventional catheter angiogram is the gold standard for defining a vascular etiology for SOV enlargement seen on CT or MRI.
Management
General Treatment
The management of SOV depends upon the underlying condition. Early diagnosis and treatment of SOV dilation may be necessary to prevent vision- and life-threatening outcomes. Depending on the etiology of disease, possible treatments can include observation, topical medication, anticoagulation therapy, chemotherapy, antibiotics, steroids, and surgery [1].
Medical Therapy
Patients with an infectious (septic) cavernous sinus or SOV thrombosis require antibiotic therapy. Aseptic SOV or cerebral venous thrombosis may be treated with anticoagulation therapy alongside empiric antibiotics but the precise role of anticoagulation in SOV thrombosis is controversial (5). Some cases of venous thrombosis depending on the underlying cause (e.g., inflammation) have been treated with systemic steroids, functional endoscopic surgery, chemotherapy, and observation [1].
Treatment for vascular malformations including dural-cavernous fistulas and carotid-cavernous fistulas includes endovascular embolization of the fistula under general anesthesia [1][12]. Additional treatments include conservative management with observation, topical glaucoma medication, and manual carotid compression maneuvers [1]. Patients diagnosed with an orbital AVM or facial AVM also typically undergo endovascular embolization [1]. Cases presenting with idiopathic orbital inflammation can be treated using systemic steroid therapy and IV anticoagulation if necessary [1].
Surgery and endovascular embolization
SOV dilations with underlying AVM can be treated using advanced endovascular embolization via a transvenous or transarterial approach [1][12]. The SOV itself can be used to provide vascular access for endovascular embolization. [13]Other surgeries that have been done to treat underlying etiologies leading to SOV dilation include functional endoscopic surgery for venous thrombosis. Some patients may have a direct SOV approach to endovascular embolization.
Prognosis
The prognosis depends upon the underlying etiology. Adam et al. showed that visual impairment was present in 26% of all the cases presenting with SOV dilation [1]. Patients with orbital cellulitis, orbital hemorrhage, orbital AVM, cavernous sinus thrombosis, and SOV thrombosis were more likely to have visual impairment upon initial presentation [1].
Summary
SOV enlargement is a radiographic sign of increased intraluminal or extraluminal compression or retrograde flow into the SOV. The finding of SOV enlargement on orbital/cranial CT or MRI is not specific to the underlying diagnosis. Some cases are associated with orbital inflammatory, infectious, metabolic (e.g., thyroid eye disease), ischemic, or compressive etiologies. The gold standard imaging for vascular malformations is a catheter angiogram which may be both diagnostic (e.g., carotid cavernous fistula) and therapeutic (e.g., endovascular closure). Clinicians should be aware of the symptoms and signs of orbital and cranial lesions producing SOV enlargement.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 Adam, C. R. et al. Dilated Superior Ophthalmic Vein: Clinical and Radiographic Features of 113 Cases. Ophthalmic Plastic & Reconstructive Surgery 34, 68–73 (2018).
- ↑ Wei, R., Cai, J., Ma, X., Zhu, H. & Li, Y. Imaging diagnosis of enlarged superior ophthalmic vein. Zhonghua Yan Ke Za Zhi 38, 402–404 (2002).
- ↑ 3.0 3.1 Azzam, D., Cypen, S. & Tao, J. Anatomy, Head and Neck: Eye Ophthalmic Vein. in StatPearls (StatPearls Publishing, 2023).
- ↑ Cheung, N. & McNab, A. A. Venous Anatomy of the Orbit. Invest. Ophthalmol. Vis. Sci. 44, 988 (2003).
- ↑ Nabavizadeh, S. A., Sundararajan, S. H., Schmitt, J. E. & Loevner, L. A. Reversible Dilation of the Superior Ophthalmic Vein in Intubated Patients. AJNR Am J Neuroradiol ajnr;ajnr.A5699v1 (2018) doi:10.3174/ajnr.A5699.
- ↑ Peyster, R. G., Savino, P. J., Hoover, E. D. & Schatz, N. J. Differential Diagnosis of the Enlarged Superior Ophthalmic Vein: Journal of Computer Assisted Tomography 8, 103–107 (1984).
- ↑ Ozpinar, A., Mendez, G. & Abla, A. A. Epidemiology, genetics, pathophysiology, and prognostic classifications of cerebral arteriovenous malformations. in Handbook of Clinical Neurology vol. 143 5–13 (Elsevier, 2017).
- ↑ Byrne, J. V. Cerebrovascular malformations. Eur Radiol 15, 448–452 (2005).
- ↑ Rose, A. L. & Cathey, S. S. Genetic Causes of Vascular Malformations and Common Signaling Pathways Involved in Their Formation. Dermatologic Clinics 40, 449–459 (2022).
- ↑ Rana, K., Juniat, V., Slattery, J., Patel, S. & Selva, D. Dilated superior ophthalmic vein: systemic associations. Int Ophthalmol 43, 3725–3731 (2023).
- ↑ 11.0 11.1 Tsutsumi, S., Nakamura, M., Tabuchi, T. & Yasumoto, Y. The superior ophthalmic vein: delineation with high-resolution magnetic resonance imaging. Surg Radiol Anat 37, 75–80 (2015).
- ↑ 12.0 12.1 Théaudin, M. et al. Diagnosis and treatment of dural carotid-cavernous fistulas: a consecutive series of 27 patients. J Neurol Neurosurg Psychiatry 78, 174–179 (2007).
- ↑ Hunt PJ, Mudie L, Yen MT. Superior Ophthalmic Vein Cannulation for Treatment of Cavernous Sinus-Dural Fistulas, www.EyeWiki.org, last accessed February 4, 2024.