Conjunctival Biopsy in the Diagnosis of Ocular Sarcoidosis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Ocular Sarcoidosis
Sarcoidosis is a granulomatous disease that affects multiple organ systems. As a multi-system disease, it can present with a variety of symptoms which often makes diagnosis challenging. Ocular involvement occurs in approximately 25-38% of cases of sarcoidosis[1] [2] [3] and is the first sign of disease in about 20% of cases[4]. Typical ocular signs of sarcoidosis include granulomatous iridocyclitis, retinal periphlebitis, and/or chorioretinitis[5]. However, other diseases may present with similar findings, including tuberculosis, syphilis, and primary intraocular lymphoma[6] [7] [8].
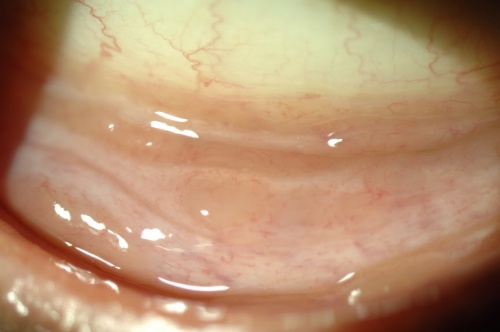
Conjunctival Nodules
Performance of a thorough slit lamp examination can identify conjunctival nodules in 7-17% of patients with ocular sarcoidosis[1][9]. These conjunctival findings appear as small, yellow or tan nodules primarily in the lower cul-de-sac. They may also appear on the lacrimal gland. Classically, the lesions are described as having a size and appearance similar to that of a millet seed[10].
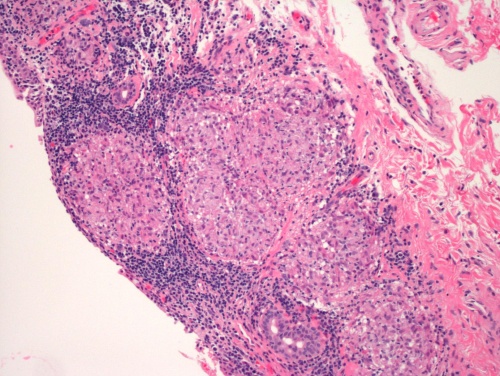
Histopathology
To definitively diagnose sarcoidosis, histologic evidence of granulomatous inflammation is required. Classically, non-caseating granulomas (aggregates of epithelioid histiocytes) may be found within the substantia propria[11]. A minimal cuff of lymphocytes and plasma cells surround the lesions. Multinucleated giant cells may or may not be present within the granuloma. Two other microscopic features often present, yet not pathognomonic, in the granulomas include Schaumann bodies and asteroid bodies. Schaumann bodies are laminated concretions composed of calcium and proteins, while asteroid bodies are stellate inclusions enclosed within giant cells[12].
The American Academy of Ophthalmology's Pathology Atlas contains a virtual microscopy image of Granulomatous Conjunctivitis [13]
Diagnostic Yield of Conjunctival Biopsy
Since the practice of obtaining conjunctival biopsy began, much debate has ensued regarding performing directed versus non-directed biopsies, and little consensus exists concerning the optimal method of histologic sectioning. Reported diagnostic yield of blind conjunctival biopsy ranges from 20% to 70%[14] [15] [16] [17] while directed biopsy ranges from 36% to 75%[18] [19] [20] [21]. The recovery of granulomas with conjunctival biopsy using careful sectioning technique approaches the yield obtained from other tissue sites[10][22], especially when conjunctival pathology such as nodules, follicles or fibrous scarring is present[8][17][23]
Biopsy Technique: Standard Sectioning vs. Multi-Plane Sectioning
Different tissue sectioning and analysis techniques may explain the wide range of conjunctival biopsy yield obtained; however, few studies actually describe their histologic methodology. A retrospective case series conducted at the University of Illinois at Chicago reported the diagnostic yield of directed conjunctival biopsy and compared an institutional standard tissue sectioning method to a multi-plane sectioning technique[24]. The surgical technique is described below:
- After identifying and marking conjunctival nodules, 1% lidocaine was injected into the subconjunctival space, ballooning up the area for biopsy.
- The lower eyelid was then retracted and the inferior fornix was grasped away from the identified nodules with 0.12 forceps.
- Strips of the involved conjunctiva were then excised using Westcott scissors, flattened and placed onto a piece of filter paper.
- Hemostasis was achieved by applying pressure for 2-3 minutes and prophylactic antibiotic drops were then instilled into the lower fornix.
Following a few seconds of air-drying, the paper was placed into 10% neutral buffered formalin. Tissue samples were then embedded in paraffin, sectioned and stained with hematoxylin and eosin. Two different sectioning techniques were then used: a standard technique and a multi-plane sectioning technique. For the standard technique, a ribbon of tissue with 5 sections was cut from a block at 1 level and placed on a glass slide. For the multi-plane technique, the standard sectioning process was repeated at 3 different levels 15 microns apart. This method allows for an increased amount of sections per tissue sample for analysis when compared to standard tissue sectioning technique[24].
A positive result was defined as the presence of discrete non-caseating granulomas identified in at least one section. If the initial biopsy result using the standard technique was negative, the tissue block underwent repeat sectioning using the multi-plane technique.
The report found that directed conjunctival biopsy using standard histologic processing method produced a yield of 43%. Of the biopsies that were negative via the standard histologic method, one additional positive case was identified when re-sectioned using the multi-plane method. When both sectioning techniques were taken into consideration, there was a cumulative yield of 63%. None of the patients with biopsies consistent with sarcoidosis were on topical corticosteroids at the time of biopsy, while several with negative biopsies were in patients on topical corticosteroid drops for at least one month before biopsy. There were no complications of biopsy in this series[24].
Directed conjunctival biopsy is an easy procedure that may allow for tissue diagnosis of sarcoidosis. Conjunctival biopsy carries a low risk of morbidity and, if possible, should be considered before more invasive procedures. Because a biopsy may include normal conjunctiva in addition to nodules, and granulomas are not uniformly distributed, the increase in the number of sections through different levels at different depths obtained when using the multi-plane sectioning technique may enhance the likelihood of detecting granulomas.
References
- ↑ Jump up to: 1.0 1.1 Obenauf CD, Shaw HE, Sydnor CF, et al. Sarcoidosis and its ophthalmic manifestations. Am J Ophthalmol. 1978;86(5):648-655.
- ↑ James DG, Anderson R, Langley D, Ainslie D. Ocular sarcoidosis. Br J Ophthalmol. 1964;48:461-470.
- ↑ Jabs DA, Johns CJ. Ocular involvement in chronic sarcoidosis. Am J Ophthalmol.1986;102(3):297-301.
- ↑ Heiligenhaus A, Wefelmeyer D, Wefelmeyer E, et al. The eye as a common site for the early clinical manifestation of sarcoidosis. Ophthalmic Res. 2011;46(1):9-12. Epub 2010 Nov 23.
- ↑ Takase H, Shimizu K, Yamada Y, et al. Validation of international criteria for the diagnosis of ocular sarcoidosis proposed by the first international workshop on ocular sarcoidosis. Jpn J Ophthalmol. 2010 Nov;54(6):529-36.
- ↑ Choi DE, Birnbaum AD, Oh F, et al. Pediatric uveitis secondary to probable, presumed, and biopsy-proven sarcoidosis. J Pediatr Ophthalmol Strabismus. 2011;48:157-62.
- ↑ Birnbaum AD, Huang W, Sahin O, et al. Ocular sarcoidosis misdiagnosed as primary intraocular lymphoma. Retina. 2010;30:310-6.
- ↑ Jump up to: 8.0 8.1 Birnbaum AD, Oh FS, Chakrabarti A, et al. Clinical features and diagnostic evaluation of biopsy proven ocular sarcoidosis. Arch Ophthalmol. 2011;129:409-13.
- ↑ Jabs DA, Johns CJ. Ocular involvement in Chronic Sarcoidosis, Am J Ophthalmol. 1986;102:291-301.
- ↑ Jump up to: 10.0 10.1 Leavitt JA, Campbell RJ. Cost-effectiveness in the diagnosis of sarcoidosis: the conjunctival biopsy. Eye. 1998;12:959-62.
- ↑ Wertheim MS, Mathers WD, Suhler EB, et al. Histopathological features of conjunctival sarcoid nodules using noninvasive in vivo confocal microscopy. Arch Ophthalmol. 2005 Feb;123(2):274-6.
- ↑ Gupta N, Rajwanshi A, Gupta D. Schaumann body in a case of sarcoidosis diagnosed on transbronchial FNAC. J Cytol. 2011 Apr-Jun; 28(2): 88-89.
- ↑ Ocular Pathology Atlas. American Academy of Ophthalmology Web site. https://www.aao.org/resident-course/pathology-atlas. Published 2016. Accessed December 21, 2016.
- ↑ Nichols DW, Eagle RC Jr, Yanoff M, et al. Conjunctival biopsy as an aid in the evaluation of the patient with suspected sarcoidosis. Ophthalmology 1980;87:287-91.
- ↑ Karcioglu AZ, Brear R. Conjunctival Biopsy in sarcoidosis. Am J Ophthalmol 1985;99:68-73.
- ↑ Hershey JM, Pulido JS, Folberg R, et al. Non-caseating conjunctival granulomas in patients with multifocal choroiditis and panuveitis. Ophthalmology 1994;101:596-601.
- ↑ Jump up to: 17.0 17.1 Chung YM, Lin YC, Huang DF, et al. Conjunctival biopsy in sarcoidosis. J Chin Med Assoc. 2006;69:472-7.
- ↑ Crick RP, Hoyle C. Mather G. Conjunctival biopsy in sarcoidosis. Br Med J. 1955;2:1180-1.
- ↑ Niitu Y, Horikawa M, Suetake T, et al. Comparisson of clinical and laboratory findings of intrathoracic sarcoidosis between children and adults. Ann N Y Acad Sci. 1976;278:532-8.
- ↑ Merritt JC, Lipper SL, Peiffer RL, et al. Conjunctival biopsy in sarcoidosis. J Natl Med Assoc. 1980;72:347-9.
- ↑ Solomon DA, Horn BR, Byrd RB, et al. The diagnosis of sarcoidosis by conjunctival biopsy. Chest 1987;74:271-3.
- ↑ Takayama K, Nagata N, Miyagawa Y, et al. The usefulness of step sectioning of transbronchial lung biopsy specimen in diagnosing sarcoidosis. Chest 1992;102:1441-3.
- ↑ Bornstein JS, Frank Ml, Radner DB: Conjunctival biopsy in the diagnosis of sarcoidosis. NEJM 1962;261:60-64.
- ↑ Jump up to: 24.0 24.1 24.2 Bui KM, Garcia-Gonzalez JM, Patel SS, et al. Directed conjunctival biopsy and impact of histologic sectioning methodology on the diagnosis of ocular sarcoidosis. ARVO E abstract 2012.