Angiolymphoid hyperplasia with eosinophilia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease
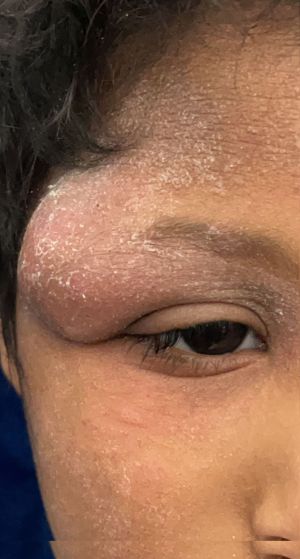
Angiolymphoid hyperplasia with eosinophilia (ALHE) is an uncommon benign neoplastic lesion. It is characterized by vascular proliferation and secondary inflammatory reaction. Wells et al.[1] were the first to describe the disease entity as persistent subcutaneous nodule and massive eosinophilic infiltration. It is unclear whether ALHE shows gender-specific trends, and previous reports in the literature lack general consensus[2]. ALHE typically presents as solitary or multiple chronic dermal nodules occurring primarily in the head and neck region. Extracutaneous involvement, such as orbital adnexa, has been also reported in the literature[3] . ALHE lesion is typically non-tender and non-pulsatile and can present as fullness of the eyelid with mechanical ptosis, proptosis, and lacrimal gland enlargement[4]. A closely related lesion known as Kimura’s disease (KD) shares some similarities with ALHE, and it was once thought a spectrum of the same disease. Some reports may be seen pointing to a close relationship between the two[5]. Published literature has shown conflicting response to the role of imaging in ALHE due to the nonspecific radiological features ALHE can present with. Therefore, the final diagnosis relies on histopathological features of this entity.
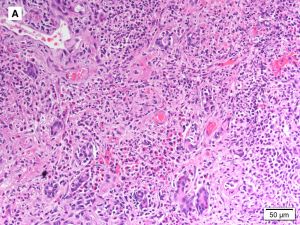
General Pathology
Light microscopic studies can accurately define the diagnosis. Histologic patterns include vascular endothelial proliferation with a variety of inflammatory cell infiltrate such as lymphocytes and eosinophils lining the vascular endothelial beds . The tumor often arises in the lumen of the capillaries, arterioles, and venules or in the wall and expands out into the surrounding soft tissue[6] . Immunostaining for vascular markers can highlight the obscurity of vessels lumen. The endothelial cells lining the vascular lumina are classically thick, plumb, and epithelial-like[7]. They also can look like a nest of epithelial cells rather than vessels with lumen. The vascular endothelium was frequently found to demonstrate cytoplasmic vacuoles and nuclear atypia[8]. However, this specific histological feature is not pathognomonic for ALHE. Proliferating vessels tend to be arranged in lobules with a brisk of lymphocytic background and germinal center formations. In addition, background eosinophils are usually abundant and robust. Yet, some cases may have sparse inflammation and a few scattered eosinophils are present.
Signs and Symptoms
ALHE should be suspected in patients with lid swelling, proptosis, ptosis, diplopia, dystopia, and/or ocular dysmotility[9]. Pain is not typically present in patients with ALHE, and this should raise the suspension of an underlying malignancy. The duration of symptoms until diagnosis can vary from few weeks[10] to 12 years[11] , and the mean duration of ALHE symptoms reported in the literature is 18 months[9]. In 75% of all reported cases of orbital ALHE, patients were more than 30 years of age, but age at diagnosis can be as early as 4 years and as late as 86 years[9]. ALHE is generally unilateral but can present as bilateral[9].
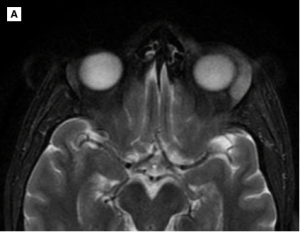
Imaging
The choice of imaging study depends on the clinical context. CT scan and MRI can help localize and define the extent of the lesion in reference to 3-dimensional anatomy. However, when iodinated contrast media cannot be performed due to patient’s allergy to iodinated contrast, MRI is recommended for exact lesion characterization. ALHE can involve the orbit, lacrimal gland, eyelids, or less commonly conjunctiva. The most common site of involvement was superotemporal orbit. CT scan shows intense enhancement of the lesion following intravenous injection of contrast media. If the lacrimal gland is to be involved, inflammatory changes are usually noted. Lacrimal gland involvement is associated with preseptal thickening and infiltration of the superolateral compartment of the extraconal fat with enlargement of the extraocular muscles. The lesion is typically well circumscribed and located in the extraconal orbital compartment, abutting the lateral orbital wall and lateral zygoma. MRI can show the lacrimal gland exhibiting high T2/FLAIR and low T1 signal intensity with homogeneous enhancement on the post-contrast images. Evidence of globe infiltration was not reported in the literature.
Differential diagnosis
The differential diagnosis of ALHE primarily includes soft tissue masses of the orbit, including but not limited to:
- Kimura's disease (or eosinophilic lymphogranuloma)
- Orbital hemangioma
- Lymphangioma
- Orbital pseudotumor
- Hodgkin’s lymphoma
- Castleman’s disease
- Langerhans cell histiocytosis
- Angioimmunoblastic T cell lymphoma
- Eosinophilic granulomatosis with polyangiitis
- Drug-induced and parasitic lymphadenitis
- Thyroid Eye Disease (Graves' disease)
Management
Treatment is primarily intended to alleviate symptoms and to address aesthetic concerns. Similar to many tumors involving the orbit, surgical excision or debulking is the preferred treatment modality[12] and is often curative. Other forms of treatment, including intralesional steroid, oral propranolol, interferon therapy, and irradiation, have all been reported[13]. Observation awaiting spontaneous regression can be considered in areas where extensive surgical excision can be disfiguring[14]. Recurrences can take place in bilateral disease or after incomplete excision[15].
References
- ↑ Wells GC, Whimster IW (1969) Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 81(1):15. https://doi.org/10.1111/j.1365-2133.1969.tb15914.x
- ↑ Padilla-España L, Fernández-Morano T, Del Boz J, Fúnez-Liébana R (2013) Angiolymphoid hyperplasia with eosinophilia: analysis of 7 cases. Actas Dermosifiliogr 104(4):353–355. https://doi.org/10.1016/j.adengl.2012.04.023
- ↑ Apple D, Boniuk M, Buggage RR, Spraul CW, Wojno TH, Grossniklaus HE (1999) Clinical pathologic review kimura disease of the orbit and ocular adnexa. Surv Ophthalmol. https://doi.org/10.1016/S0039-6257(99)00064-8
- ↑ Mukherjee B, Kadaskar J, Priyadarshini O, Krishnakumar S, Biswas J (2016) Angiolymphoid hyperplasia with eosinophilia of the orbit and adnexa. Ocul Oncol Pathol 2(1):40–47. https://doi.org/10.1159/000433545
- ↑ Esmaili DD, Chang EL, O’Hearn TM, Smith RE, Rao NA (2008) Simultaneous presentation of kimura disease and angiolymphoid hyperplasia with eosinophilia. Ophthalmic Plast Reconstr Surg 24(4):310–311. https://doi.org/10.1097/IOP.0b013e31817e9bba
- ↑ Balaji Prasad TS, Suresh PS, Rodrigues G, Patel M, Moriarty AP (2000) Orbital involvement with angiolymphoid hyperplasia with eosinophilia —a benign condition for the practising ophthalmologist to be aware of. Eye 14:390–392
- ↑ Fernandes BF, Al-Mujaini A, Petrogiannis-Haliotis T, Al-Kandari A, Arthurs B, Burnier MN (2007) Epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia) of the orbit: a case report. J Med Case Rep 1:2–5. https://doi.org/10.4103/00195154.100501
- ↑ Sánchez-Acosta A, Moreno-Arredondo D, Rubio-Solornio RI, Rodríguez-Martínez HA, Rodríguez-Reyes AA (2008) Angiolymphoid hyperplasia with eosinophilia of the lacrimal gland: a case report. Orbit 27(3):195–198. https://doi.org/10.1080/01676830701804099
- ↑ Jump up to: 9.0 9.1 9.2 9.3 Alfarhan A, Maktabi A, Alofi MM, Alotaibi HM. Angiolymphoid hyperplasia with eosinophilia: a case series and literature review. Int Ophthalmol. 2023 Jul;43(7):2457-2467. doi: 10.1007/s10792-023-02644-y. Epub 2023 Mar 4. PMID: 36869976.
- ↑ Galindo-Ferreiro A, Alkatan HM, Elkhamary SM, Maktabi A, Schellini S, Cruz AAV (2016) Orbital and adnexal involvement in angiolymphoid hyperplasia with eosinophilia (ALHE): a case series. Clin Case Rep Rev 2:579–583
- ↑ Mukherjee B, Kadaskar J, Priyadarshini O, Krishnakumar S, Biswas J (2016) Angiolymphoid hyperplasia with eosinophilia of the orbit and adnexa. Ocul Oncol Pathol 2(1):40–47. https://doi.org/10.1159/000433545
- ↑ Cunniffe G, Alonso T, Dinarès C, Medina FJ, Medel R (2014) Angiolymphoid hyperplasia with eosinophilia of the eyelid and orbit: the Western cousin of Kimura’s disease? Int Ophthalmol 34(1):107–110. https://doi.org/10.1007/s10792-013-9741-7
- ↑ Wolff D, Andree H, Hilgendorf I, Casper J, Freund M, Junghanss C (2008) Sirolimus in combination with tacrolimus in allogeneic stem cell transplantation-timing and conditioning regimen may be crucial. Biol Blood Marrow Transpl 14(8):942–943. https://doi.org/10.1016/j.bbmt.2008.05.004
- ↑ Lin B, Tan SH, Looi A (2008) Angiolymphoid hyperplasia with eosinophilia of the eyelid with spontaneous regression. Ophthal Plast Reconstr Surg 24(4):308–310. https://doi.org/10.1097/IOP.0b013e31817d8765
- ↑ Sheren SB, Custer PL, Smith ME (1989) Angiolymphoid hyperplasia with eosinophilia of the orbit associated with obstructive airway disease. Am J Ophthalmol 108(2):167–169. https://doi.org/10.1016/0002-9394(89)90012-3