Amniotic Membrane Transplant
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Surgical Technique
Description
Amniotic membrane, or amnion, is the innermost layer of the placenta and consists of a thick basement membrane and an avascular stromal matrix. Amniotic membrane transplantation (AMT) has been used as a graft or as a dressing in different surgical subspecialties. In the field of ophthalmology, it is used broadly 1) to reconstruct the ocular surface after various procedures; 2) as a graft for ocular surface melts; and 3) as a bandage to promote healing in cases of persistent epithelial defects or ocular surface inflammation. All of these indications make use of amniotic membrane's ability to promote healing.[1]
History
Live fetal membrane, which included both amnion and chorion, was first documented by De Roth in 1940 for use in conjunctival reconstruction. A very low success rate was reported.[2] During the same year, Brown used rabbit peritoneum as a temporary patch for ocular surface burns which Sorsby later modified with human amniotic membrane in 1946 and 1947.[3][4] In 1995 Kim and Tseng reintroduced the idea of amniotic membrane for ophthalmic use which has since become increasingly popular.[5]
Mechanism of Action
The basement membrane component of amniotic membrane is similar in composition to the conjunctiva.[6] For this reason, current theory suggests that amniotic membrane augments support for epithelial cells, limbal stem cells, and corneal transient amplifying cells. Clonogenicity is maintained which promotes both goblet and non-goblet cell differentiation while excluding inflammatory cells and their protease activities.[7][8] Furthermore, the stromal face of amniotic membrane suppresses myofibroblast differentiation of normal fibroblasts to reduce scar and vascular formation.[9] This action assists in healing for conjunctival reconstruction, epithelial defects, and stromal ulceration.
Indications
Pterygium Excision
After surgical removal of a pterygium, a conjunctival defect remains. This defect could be left alone to heal by secondary intention, sutured directly via primary closure, grafted with a conjunctival autograft, or grafted with amniotic membrane. With intraoperative steroid injection into the surrounding tissue defect, amniotic membrane transplantation has a comparable recurrence rate to conjunctival autograft.[10] The application of mitomycin-C does not further reduce the recurrence rate according to some studies.[11][12] There are many conflicting reports regarding the rate of postoperative pterygium recurrence after the use of amniotic membrane. Amniotic membrane could be considered when the size of the operative defect would be problematic for direct closure, or when a conjunctival autograft cannot be obtained due to scarring or presence of glaucoma devices.[13][14]
Reconstruction of the Conjunctiva Surface
In addition to pterygium surgery, AMT has been used for other conjunctival reconstructive purposes. Removal of ocular surface tumors results in a defect which is often revised with amniotic membrane. Surgical use of AMT for the revision of scars and symblepharon has also been well-documented.[15][16] In cases of conjunctivochalasis that fail medical therapy, AMT has been used to reconstruct the ocular surface.[17] Scleral melts have been treated in conjunction with cadaveric sclera and overlying AMT with good success.[18] One report indicates that a leaking trabeculectomy bleb can be revised with amniotic membrane.[19]
Limbal Stem Cell Deficiency or Persistent Epithelial Defects
Amniotic membrane can be used in cases of partial and total limbal stem cell deficiency. In cases of total limbal stem cell loss, AMT alone will not suffice and needs to be used in conjunction with allogeneic stem cell transplantation.[20] For cases of partial limbal stem cell loss, and also in the case of persistent epithelial defects, amniotic membrane has shown to enhance epithelialization and improve vision with and without allogeneic limbal cell transplantation.[21]
Newer techniques include using autologous and allogeneic stem cells cultivated in the laboratory on amniotic membrane and then transplanting this combined tissue onto severely damaged corneas with no endogenous stem cells.[22][23][24][25][26][27]
Corneal Ulcer
Amniotic membrane has been used for both infectious and sterile ulcers which involve thinning and perforation. For ulcers with significant tissue loss, amniotic membrane may be applied in layers to build thickness to the defect.[28] Such an intervention is intended to retard protease activity and to provide bulk for the defect in the hopes of promoting faster healing and avoiding cornea transplantation. It can provide a temporizing measure before cornea transplantation or possibly suffice as a permanent treatment.[29] A thickened form of amniotic membrane can also be used as a patch graft in cases of infectious scleritis.
Ocular Surface Burns
Ocular surface burns may be secondary to direct heat (e.g. burns to the face) or be caused by chemicals (alkalis and acids). AMT performed immediately after an ocular surface burn has been reported to reduce the patient's pain, accelerate healing, and reduce fibrosis and neovascularization. The surgery involves securing a sheet of amniotic membrane over the entire ocular surface up to the eyelid margins.[30] AMT has efficacy in accelerating re-epithelialization in moderate burns however there is minimal proven benefit of improving re-epithelialization in severe burns[31].
Periorbital Thermal Burns
Periorbital thermal burns are challenging to repair to ensure adequate cosmesis and function. AMT in conjunction with full-thickness skin grafting has shown healthy re-epithelialization over previously burned areas and reduced scarring.[32]
Macular Hole Closure
There is no ideal treatment for failed macular hole closure that provides complete closure and visual recovery. The use of amniotic tissue for macular hole repair has demonstrated complete anatomical closure and remarkable functional results.[33]
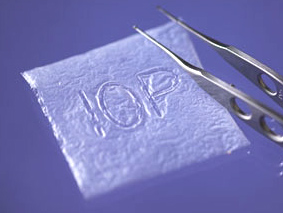
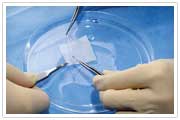
Procedure
Many reports in the literature illustrate the use of human amniotic membrane harvested from placenta at the time of caesarean section and preserved until use on the ocular surface. Cryopreserved amniotic membrane is available and commonly used, and it retains the histological and morphological properties of fresh tissue.[34] Amniotic membrane can be surgically attached to the ocular surface by absorbable or non-absorbable sutures. Biological tissue adhesives have also been used to attach amniotic membrane to the ocular surface.[35]
Risks
Allogeneic tissue has an implicit risk of infectious disease transmission. In general, amniotic membrane is procured from potential donors undergoing caesarean section who have been screened for communicable diseases such as HIV, hepatitis, and syphilis. The placenta is cleaned with a mixture of balanced salt solution, penicillin, streptomycin, neomycin, and amphotericin B. The amnion is separated from the chorion by blunt dissection under sterile conditions, attached to nitrocellulose paper strips, and stored in glycerol solution. The tissue is either stored in that solution for fresh use or cryopreserved at a temperature of -80 degrees Celsius.[36] Currently, there are no published reports of communicable disease transmission from AMT. One report exists of a sterile hypopyon after repeated transplantation of human amniotic membrane onto the corneal surface.[37]
Additional Resources
- Amniograft & Prokera: http://www.biotissue.com/
- Ambiodry2 & 5: http://www.iopinc.com/surgeons_and_medical_professionals/ambiodry2/
- Boyd K, McKinney JK. Transplantation and the Eye. American Academy of Ophthalmology. EyeSmart/Eye Health. https://www.aao.org/eye-health/treatments/transplantation-eye-list. Accessed March 25, 2019.
References
- ↑ Tseng SCG. Amniotic Membrane Transplantation for Ocular Surface Reconstruction. Bioscience Reports 2001;21(4):481-489.
- ↑ de Rotth, A. Plastic repair of conjunctival defects with fetal membrane. Arch Ophthalmol. 1940;23:522-522.
- ↑ Brown, AL. Lime burns of the eye: Use of rabbit peritoneum to prevent severe delayed effects. Arch Ophthalmol. 1941;26:754-769.
- ↑ Sorsby A, Symons HM. Amniotic membrane grafts in caustic burns of the eye. Br J Ophthalmol. 1946;30:337-345.
- ↑ Kim JC, Tseng SCG. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995;14:473-484.
- ↑ Fukuda K, Chikama T, Nakamura M, Nishida T. Differential distribution of subchains of the basement membrane components type IV collagen and laminin among the amniotic membrane, cornea, and conjunctiva. Cornea. 199;18:73-79.
- ↑ Meller D, Tseng SCG. Conjunctival epithelial cell differentiation on amniotic membrane Invest Ophthalmol Vis Sci 1999;40:879-886.
- ↑ Koizumi N, Inatomi T, Quantock AJ, Fullwood NJ, Dota A, Kinoshita S. Amniotic membrane as a substrate for cultivating limbal corneal epithelial cells for autologous transplantation in rabbits. Cornea. 2000;19:65-71.
- ↑ Tseng SCG, Li D-Q, Ma X. Suppression of Transforming Growth Factor isoforms TGF-B receptor II, and myofibroblast differentiation in cultured human corneal and limbal fibroblasts by amniotic membrane matrix. J Cell Physiol. 1999;179:325-335.
- ↑ Solomon A, Pires RTF, Tseng SCG. Amniotic membrane transplantation after extensive removal of primary and recurrent pterygia. Ophthalmology. 2001;108:449-460.
- ↑ Ma DH-K, See L-C, Liau S-B, Tsai RJF. Amniotic membrane graft for primary pterygium: comparison with conjunctival autograft and topical mitomycin C treatment. Br J of Ophthalmol. 2000;84:973-978.
- ↑ Fallah MR, Golabdar MR, Amozadeh J, et al. Transplantation of conjunctival limbal autograft and amniotic membrane vs mitomycin C and amniotic membrane in treatment of recurrent pterygium. Eye (Lond) 2008;22(3):420-424.
- ↑ Prabhasawat P, Barton K, Burkett G, Tseng SCG. Comparison of conjunctival autografts, amniotic membrane grafts and primary closure for pterygium excision. Ophthalmology. 1997;104:974-985.
- ↑ Shimazaki J, Sinozaki N, Tsubota K. Transplantation of amniotic membrane and limbal autograft for patients with recurrent pterygium associated with symblepharon. Br J Ophthalmol 1998;82:235-240.
- ↑ Tseng SCG, Prabhasawat P, Lee SH. Amniotic membrane transplantation for conjunctival surface reconstruction. Am J Ophthalmol 1997;124: 765-774.
- ↑ Azuara-Blanco A, Pillai CT, Dua HS. Amniotic membrane transplantation for ocular surface reconstruction. Br J Ophthalmol 1999;8339:399-402.
- ↑ Meller D, Maskin SL, Pires RTF, Tseng SCG. Amniotic membrane transplantation for symptomatic conjunctivochalasis refractory to medical treatments. Cornea 2000;19:796-803.
- ↑ OH JH, Kim JC. Repari of scleromalacia using preserved scleral graft with amniotic membrane transplantation. Cornea 2003;22(4):288-293.
- ↑ Budenz DL, Barton K, Tseng SCG. Amniotic membrane transplantation for repair of leaking glaucoma filterinb blebs. Am J Ophthalmol 2000;130:580-588.
- ↑ Pires RTF, Chokshi A, Tseng SCG. Amniotic membrane transplantation or limbal conjunctival autograft for limbal stem cell deficiency induced by 5-flourouracil in glaucoma surgeries. Cornea. 1999;19:284-287.
- ↑ Tseng SCG, Prabhasawat P, Barton K, Gray T, Meller D. Amniotic membrane transplantation with or without limbal allografts for cornea surface reconstruction in patients with limbal stem cell deficiency. Arch Ophthalmol. 1998;116:431-441.
- ↑ Pellegrini G, Traverso CE, Franzi AT. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet 1997;349:990-993.
- ↑ Tsai RJ, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med 2000;343:86-93.
- ↑ Schwab IR, Reyes M, Isseroff RR. Successful transplantation of bioengineered tissue replacement in patients with ocular surface disease. Cornea 2000;19:421-426.
- ↑ Koizumi N, Inatomi T, Suzuki T. Cultivated corneal epithelial transplantation for ocular surface reconstruction in acute phase of Stevens-Johnson syndrome. Arch Ophthalmol 2001;119:298-300.
- ↑ Koizumi N, Inatomi T, Suzuki T. Cultivated corneal epithelial stem cell transplantation in ocular surface disorders. Ophthalmology 2001;108:1569-1574.
- ↑ Kinoshita S. Ocular surface reconstruction by tissue engineering. J Jap Ophthalmol Soc 2002;106:837-869.
- ↑ Kruse FE, Rohrschneider K, Volcker HE. Multilayer amniotic membrane transplantation for reconstruction of deep corneal ulcers. Ophthalmology. 1999;106:1504-1511.
- ↑ Solomon A, Meller, D, Prabhasawat P. Amniotic membrane grafts for nontraumatic corneal perforations, descemetoceles, and deep ulcers. Ophthalmology 2002;109:694-703.
- ↑ Clare G, Suleman H, Bunce C, Dua H. Amniotic membrane transplantation for acute ocular burns. Cochrane Database Syst Rev. 2012;(9):CD009379.
- ↑ Veldman PB, Greiner MA, Cortina MS, Kuo AN, Li JY, Miller DD, Shtein RM, Weikert MP, Yin J, Kim SJ, Shen JF. Efficacy of Amniotic Membrane Grafting for the Treatment of Chemical and Thermal Ocular Surface Injuries: A Report by the American Academy of Ophthalmology. Ophthalmology. 2024 Oct 9:S0161-6420(24)00514-1. doi: 10.1016/j.ophtha.2024.08.021. PMID: 39387749.
- ↑ Reed DS, Plaster AL, Mehta A, Hill MD, Zanganeh TS, Soeken TA, DeMartelaere SL, Davies BW. Acute And Sub-Acute Reconstruction Of Periorbital Thermal Burns Involving The Anterior Lamella Of The Eyelid With Simultaneous Fullthickness Skin Grafting And Amniotic Membrane Grafting. Ann Burns Fire Disasters. 2020 Dec 31;33(4):323-328. PMID: 33708023; PMCID: PMC7894844.
- ↑ Caporossi, T., Pacini, B., Bacherini, D. et al. Human amniotic membrane plug to promote failed macular hole closure. Sci Rep 10, 18264 (2020). https://doi.org/10.1038/s41598-020-75292-2
- ↑ Kruse FE, Joussen AM, Rohrschneider K, You L. Cryopreserved human amniotic membrane for ocular surface reconstruction. Graefe’s Arch Clin Exp Ophthalmol 2000;238(1):68-75.
- ↑ Tseng SCG, Elizondo A, Casas V. Amniotic membrane suturing techniques. 2007. Springer Berlin Heidelberg.
- ↑ Sangwan, VS, Burman S, Tejwani S, Mahesh SP, Murthy R. Amniotic membrane transplantation: A review of current indications in the management of ophthalmic disorders. Current Ophthalmology 2007;55:251-260.
- ↑ Gabler B, Lohmann CP. Hypopyon after repeated transplantation of human amniotic membrane onto the corneal surface. Ophthalmology 2000;107:1344-1346.