Ophthalmic Artery Pseudoaneurysm
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Ophthalmic Artery Pseudoaneurysm (OAPA) is a rapid onset and vision and life-threatening condition in the setting of trauma or post-surgical complications. Proper identification of signs and symptoms of OAPA is crucial in determining management approaches to achieve optimal visual outcomes.
Disease Entity
Ophthalmic artery pseudoaneurysm is a rare condition characterized by the formation of a false aneurysm in the ophthalmic artery. The physiology of OAPA formation is similar to other large vessel pseudoaneurysms, where the shearing force from trauma causes a false lumen formation. [1] It is much rarer as the ophthalmic artery is walled off by orbital walls and cushioned by surrounding orbital adipose tissue. Only direct trauma to the orbital structures can significantly increase the risk of OAPA formation. Other risk factors identified in past literature and clinical care include anticoagulation use, high energy impact, or penetration into the orbits. [2] [3]OAPA can result from infection or surgical procedures. [4]
Etiology
In contrast to a true aneurysm, a pseudoaneurysm is not contained by the vessel wall; instead, blood leaking through a defect in the arterial wall is contained by an out-pouching of adventitia or perivascular soft tissue.[5] The most common cause of ophthalmic artery pseudoaneurysm (OAPA) is high-energy trauma, such as blunt or penetrating trauma to the eye or head. Still, it can also be caused by inflammation, infection, or previous surgical procedures. It typically presents unilaterally due to the nature of traumatic impact but can be bilateral should both orbits suffer high energy injury. [6]
Diagnosis
Patients with OAPA typically present to the emergency room as trauma activation after fall or motor vehicle accident. In the setting of acute trauma, patients may be unable to give an accurate history of the event onset. Therefore, diagnosing ophthalmic artery pseudoaneurysm (OAPA) typically involves a combination of clinical evaluation, detailed eye exams, radiological imaging studies, and additional interventional procedures.
History
Patient who presents with ophthalmic artery pseudoaneurysm already suffered high energy impact injury to the head and will most likely present with mental status change and memory loss. If available, the history-taking portion should focus on the mechanism of facial and ocular injuries. High-energy blunt and penetrating injury can both contribute to these pseudoaneurysms formations. Some of the common types of blunt trauma injuries identified in past literature include fist fight, motor vehicle accidents (head strike, airbag deployment, whiplash injuries, etc.), fall. [7] [8] There have also been recordings of penetrating orbital projectile-induced OAPA formation, such as bullets and knives. [3]
Other risk factors, such as prior history of ocular infection, cellulitis, arterial-venous fistulas, and any other significant orbital histories are also useful. [9] Comorbidities such as diabetes and cardiovascular disease are also important as patients might be taking anti-platelets or antithrombotic medications which could greatly increase the risk of pseudoaneurysm malformation.
Pseudoaneurysm formation can be iatrogenic as well. Recent past surgical and procedural histories such as nasogastric tube placement, oculoplastic surgeries, ENT surgeries, or skull-based neurosurgeries are also helpful in identifying the source of the lesion.[4]
Physical Examination
A thorough physical examination of the eye and surrounding structures should be conducted to assess visual acuity, ocular motility, and clinical signs of inflammation, swelling, proptosis, or pulsatile mass around the orbit. Increased intraocular pressure can spike suddenly due to increase in pseudoaneurysms sizes or concomitant retrobulbar hemorrhage. Prompt reduction in IOP should be considered immediately based on available IOP readings and physical examination findings.
Diagnostic Procedures
Studies in the literature have reported using various imaging techniques such as CT, MRI, or digital subtraction angiography to aid in the diagnosis of pseduoanyerysm[3][10]. CT and CT-Angiogram would be the ideal screening modalities, while digital subtraction angiography would be most specific in diagnosing these lesions.[4]
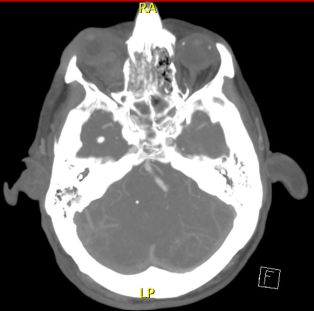
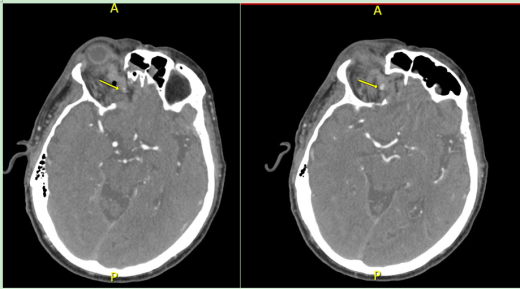
CT Head, CT angiogram
When patient first presented to the emergency room, CT head without contrast and CT angiogram are extremely helpful in identifying intracranial bleeding and vasular lesions. CT angiograms of the head and the neck are also helpful in identifying vascular injuries. Based on past literature information and ED triaging experience, pseudoaneurysm may expand quickly in the size in its early phase of development, which may mimic an expanding hematoma. However, the exact timing of OAPA progression may not occur until up to 24 hours after the initial injury. Follow up imaging will be helpful in monitoring the size of progression and determining next step management. Unlike hematoma, pseudoaneurysms will stabilize in size without active contrast extravasation.
MRI, MRA, MRV, and Angiography
Patient with suspected OAPA typically requires Neuro-ICU level of care. Follow up advanced imaging such as MRI, MRA, MRV are helpful in confirming the diagnosis and identifying the source of lesion. Based on past literature research, MRI, MRA, and MRV are all reasonable diagnostic imaging studies for these types of scenarios. Angiogram through Neuro-Intervention is the most confirmatory imaging yet most invasive. It will help to visualize the lesion in real time with detailed information on size and hemodynamics. Angiogram can be both diagnostic and curative to OAPA. However, detailed discussions on embolization prognosis should discuss in details with patients as the location of these pseudoaneurysms are in proximity to the central retinal artery and embolization procedure may potentially lead to permanent vision loss.
Management
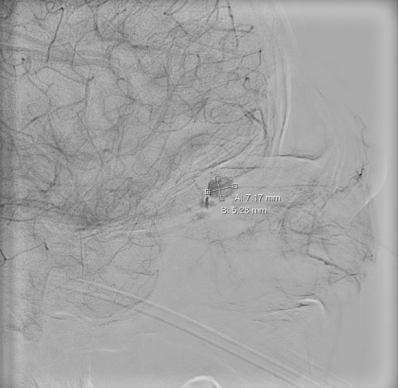
Neuro-Intervention (endovascular coiling)
Prompt endovascular occlusion can prevent complications such as enlargement, hemorrhage, and hematoma formation.[11] This can be achieved by microcatheterization and coil embolization.[7] In this procedure an endovascular wire is navigated close to the pseudoaneurysm, followed by a microcatheter which is then used to deliver the coil for embolization. Angiography is then used to confirm a complete coil embolization. If the proximal ophthalmic artery becomes occluded, branches of the external carotid artery provide collateral blood flow to the visual system through anastomoses with the extra-orbital branches of the ophthalmic artery.[10] However, the central retinal artery is also at risk of been injured and occluded if the pseudoaneurysm is in close proximity.
One study reported a case of OAPA presenting with persistent epistaxis after removal of a nasogastric tube.[4] This patient was treated with 25% NBCA injection to embolize the lesion.
Surgery, External Approach
Other than endovascular approach, there have also been recorded cases of external surgical approach to surgically remove the pseudoaneurysms. It is a much more invasive technique and the final outcomes are worse compared to endovascular embolization. There have been only 2 recorded cases of external surgical approach completed in China and Japan [2]. The surgery in China was performed on a patient who suffered blunt trauma (punch) to the orbits. The surgeons were able to successfully remove the pseudoaneurysm by entering through right cranio-orbital approach with orbital decompression. However, due to the degree of injury to the globe and optic nerve, visual acuity remained at NLP with total ophthalmoplegia [2]. The case in Japan was also performed on on a patient who sustained closed head injury from motor vehicle accident. The surgeons were successfully able to resect the psuedoanuerysm through extradural approach. However visual acuity remained at NLP.
Conservative Management
At this time there have been one recorded conservative management case in approaching OAPA, which was done at Umass Memorial Medical Center. Through multi-disciplinary care approach involving ophthalmology, neruo-intervention, neruo-critical care, the patient's pseudoaneurysm self-embolized as demonstrated by serial CT-Angiogram scans.
Prognosis
OAPAs are dangerous because they can enlarge over time and eventually rupture, resulting in intracranial hemorrhage or hematoma formation.[11] Pseudoaneurysm of the dural portion of the ophthalmic artery can result in subarachnoid hemorrhage with a high risk of re-hemorrhage if left untreated.[7]
Outcomes:
Visual recovery in endovascular occlusions cases have been most likely been successful with low rate of central retinal artery occlusion. Timely management of these pseudoaneurysms successfully reduced the rate of intracranial bleeding and mortalities. Current literature showed 0% of mortality rate among patients with OAPA that were managed surgically. However, should the initial trauma injury caused significant globe optic nerve injury, visual outcome may be limited and may eventually require evisceration or enucleation.
Complications:
For patient who underwent successful endovascular embolization, some of the common complications recorded include ptosis, vasospasms. For patients who underwent interventions, but were unsuccessful in recovering beyond no light perceptions in the traumatic eyes, corneal edema, pain, and proptosis are the most common symptoms and these patients eventually required eviscerations or enucleations for comfort measures.
Cranial nerves are also susceptible to injuries even after pseudoaneurysm embolization or self-embolization, though this affect may be transient. For the one patient who underwent serial CT-Angiogram monitoring without monitoring at University of Massachusetts Memorial Hospital, complete cranial nerve 3 palsy with persistent traumatic pupil of the injured eye was discovered on follow up 1 month later. The exact etiologies for the palsy were unclear but may be related to transient compression after the traumatic injury. The CN3 palsy self-resolved about 2 months follow up; however, the traumatic pupil persisted the visual acuity failed to correct to 20/70 or better (the unaffected eye been 20/30). Given patient’s age and cardiovascular risk factors, the decision was made to closely monitor without any more procedural intervention.
Literature Summary
OAPAs are dangerous because they can enlarge over time and eventually rupture, resulting in intracranial hemorrhage or hematoma formati
Below is the table listing all past literatures discussing OAPA, the team’s treatment approaches, surgical outcomes, and complications.
| Studies/Cases | Case size | Year | Types of injury | Location of OAPA | Management | Complications | Outcome |
| Czyz C, et al.[3] | 1 | 2017 | Penetrating bullet intra-orbital | Endovascular occlusion coiling | Corneal edema, hyphemia, hemorrhagic chemosis | NLP, evisceration | |
| Chun H, et al.[11] | 1 | 2007 | Motor vehicle accident, blunt head trauma | Extra-cranial, left ethmoid branch | Endovascular occlusion coiling | None | Intervention induced vasospasm, self-sealed |
| Balushi AA, et al.[6] | 1 | 2017 | Penetrating bullet intra-orbital | bilateral ophthalmic artery | Endovascular occlusion coiling | None | Clinically stable |
| Kelly ME, et al.[8] | 1 | 2009 | Bicycle accident, blunt head trauma | Right ophthalmic artery | Endovascular occlusion coiling | Failed first attempt | Clinically stable |
| Rosssitti S, et al. | 1 | 2009 | Non-trauma, progressive vision loss | Right ophthalmic artery | Endovascular occlusion coiling | None | Clinically stable |
| Li Y, et al.[2] | 1 | 2017 | Fist fight, blunt head trauma | Right ophthalmic artery | External surgical resection | None | NLP, ophthalmoplegia |
| Dolati-Ardejani P, et al.[12] | 1 | 2012 | Fall, blunt head trauma | Right ophthalmic artery | Endovascular embolization coiling | Failed procedure, occlusion of the proximal OphA | NLP |
| Liao Zb, et al[9] | 1 | 2023 | Motor vehicle accident, blunt head trauma | Right ophthalmic artery | Endovascular occlusion coiling | None | None |
| Seluck H, et al | 1 | 2005 | Nasogastric tube placement | Left ophthalmic artery | Endovascular occlusion (NBCA-histoacryl (25%) injection) | None | None |
| Kikkawa Y, et al. | 1 | 2012 | Closed head injury | Left ophthalmic artery | External surgical resection | None | NLP |
| Kanazawa R, et al. | 1 | 2011 | Fall, blunt head injury | Left ophthalmic artery | Endovascular occlusion coiling | Redo in 5 months | None |
| Ren Y, et al. UMass Memorial Case | 1 | 2023 | Fall, blunt trauma | Right mid-ophthalmic artery | Conservative watch | Ptosis, traumatic pupil | Clinically stable, visual acuity 20/70 in OD |
References
- ↑ Peick AL, Nichols WK, Curtis JJ, Silver D. Aneurysms and pseudoaneurysms of the superficial temporal artery caused by trauma. J Vasc Surg. 1988;8(5):606-610.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 Li Y, Song WX, Zhang TM, Fu JD, Sun S, Zhao JZ. Intraorbital traumatic ophthalmic artery aneurysm: case report. Neurol India. 2012 Nov-Dec;60(6):657-60. doi: 10.4103/0028-3886.105213. PMID: 23287341.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 Czyz CN, Piehota PG, Strand AT, Stein M. Post-traumatic ophthalmic artery pseudoaneurysm from orbital projectile. Can J Ophthalmol. Aug 2017;52(4):e130-e132. doi:10.1016/j.jcjo.2016.12.007
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Selcuk H, Soylu N, Albayram S, et al. Endovascular treatment of persistent epistaxis due to pseudoaneurysm formation of the ophthalmic artery secondary to nasogastric tube. Cardiovasc Intervent Radiol. 2005;28(2):242-5. doi:10.1007/pl00021048
- ↑ Patil NS, Kumar AH, Pamecha V, et al. Cystic artery pseudoaneurysm-a rare complication of acute cholecystitis: review of literature. Surg Endosc. Feb 2022;36(2):871-880. doi:10.1007/s00464-021-08796-1
- ↑ Jump up to: 6.0 6.1 Al Balushi A, Kitchener J, Edgell RC. Bilateral ophthalmic artery dissecting aneurysms presenting with recurrent epistaxis. J Vasc Interv Neurol. 2017 Jan;9(3):14-16. PMID: 28243345; PMCID: PMC5317286.
- ↑ Jump up to: 7.0 7.1 7.2 Kelly ME, Fiorella D. Traumatic ophthalmic artery pseudoaneurysm coiled with a steerable microcatheter. Can J Neurol Sci. Jul 2009;36(4):496-9. doi:10.1017/s0317167100007861
- ↑ Jump up to: 8.0 8.1 Kelly ME, Fiorella D. Traumatic ophthalmic artery pseudoaneurysm coiled with a steerable microcatheter. Can J Neurol Sci. 2009 Jul;36(4):496-9. doi: 10.1017/s0317167100007861. PMID: 19650364.
- ↑ Jump up to: 9.0 9.1 Liao, Z., Long, X., & Li, J. (2023). Endovascular treatment of pseudoaneurysm of ophthalmic artery with carotid-cavernous fistula: A case report. Interdisciplinary Neurosurgery, 101889.
- ↑ Jump up to: 10.0 10.1 Hopkins JK, Shaibani A, Ali S, et al. Coil embolization of posttraumatic pseudoaneurysm of the ophthalmic artery causing subarachnoid hemorrhage. Case report. J Neurosurg. Nov 2007;107(5):1043-6. doi:10.3171/JNS-07/11/1043
- ↑ Jump up to: 11.0 11.1 11.2 Chun HJ, Yi HJ. Traumatic extracranial pseudoaneurysm on the peripheral ophthalmic artery presenting as delayed intraparenchymal hematoma: case report. Surg Neurol. 2009 Jun;71(6):701-704. doi:10.1016/j.surneu.2007.11.018.
- ↑ Dolati-Ardejani, P., Morrish, W. F., & Wong, J. H. (2012). Posttraumatic Ophthalmic Artery Pseudoaneurysm Presenting Epistaxis: Case Report and Review of the Literature. Journal of Neurological Surgery Part B: Skull Base, 73(S 01), A286.