Ophthalmic Artery Pseudoaneurysm
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Ophthalmic Artery Pseudoaneurysm (OAPA) is a rapid-onset, vision and life-threatening condition that may occur in the context of trauma or post-surgical complications. Proper identification of the signs and symptoms of OAPA may help achieve optimal visual outcomes.
Disease Entity
OAPA is a rare condition characterized by the formation of a false aneurysm in the ophthalmic artery. The process of OAPA formation shares similarities with other large vessel pseudoaneurysms, wherein the shearing force resulting from trauma leads to the creation of a false lumen.[1] OAPA is uncommon due to protection from the orbital walls and surrounding orbital adipose tissue. The risk of OAPA formation is significantly heightened only in the presence of direct trauma to the orbits. Additional risk factors identified in previous literature and clinical practice include the use of anticoagulation, high-energy impact, or penetration into the orbits.[2] [3] OAPA can also result from infection or surgical procedures. [4]
Etiology
In contrast to a true aneurysm, a pseudoaneurysm is not contained by the vessel wall; instead, blood leaking through a defect in the arterial wall is contained by an out-pouching of adventitia or perivascular soft tissue.[5] The primary cause of OAPA is typically high-energy trauma, including blunt or penetrating injuries to the eye or head. However, it can also arise from inflammation, infection, or prior surgical procedures. Typically, the presentation is unilateral due to the nature of traumatic impact, but bilateral occurrence can occur if both orbits experience high-energy injuries. [6]
Diagnosis
Patients with OAPA commonly arrive at the emergency room as trauma activations following a fall or motor vehicle accident. In the context of acute trauma, patients may be unable to provide an accurate history. Diagnosing OAPA typically necessitates a comprehensive approach, including clinical evaluation, detailed eye examinations, radiological imaging studies, and additional interventional procedures.
History
The history should focus on the mechanism of facial and ocular injuries. High-energy blunt and penetrating injury can both contribute to these pseudoaneurysm formations. Common types of blunt trauma injuries identified in past literature include fist fights, motor vehicle accidents (head strike, airbag deployment, whiplash injuries, etc.), and falls. [7] [8] There have also been recordings of penetrating orbital projectile-induced OAPA formation (e.g., secondary to bullets or knives). [3]
Other risk factors, such as prior ocular infection, cellulitis, arteriovenous fistulas, and other significant orbital histories , may also be relevant. [9] Comorbidities such as diabetes and cardiovascular disease are important, as patients may be taking anti-platelets or antithrombotic medications, which increase the risk of pseudoaneurysm formation.
Pseudoaneurysm formation can be iatrogenic as well. Recent past surgical and procedural histories such as nasogastric tube placement or oculoplastic, ENT, or skull base surgeries are also helpful in identifying the source of the lesion.[4]
Physical Examination
A comprehensive physical examination of the eye and its surrounding structures is essential. The examiner should focus on visual acuity and ocular motility. Some of the common bedside findings include chemosis, subconjunctival hemorrhage, proptosis, and pulsatile mass around the orbit. Drawing from clinical experience at UMass Memorial Medical Center, the appearance of a pulsatile mass around the orbit emerges as the most indicative sign of OAPA formation.
Intraocular pressure (IOP) can spike suddenly due to an increase in OAPA volume or concomitant retrobulbar hemorrhage. Prompt reduction in IOP (with glaucoma eye drops, canthotomy/cantholysis) should be considered based on available IOP readings and physical examination findings. Communication with the neurosurgery or neuro-critical care team to determine dilation status, then obtaining a dilated funduscopic exam at the earliest convenience, will to identify potential retinal hemorrhages and ischemic injuries.
Diagnostic Procedures
Previous studies have reported using various imaging techniques such as CT, CTA, MRI, MRV, MRA, or digital subtraction angiography to aid in the diagnosis of pseudoaneurysm[3][10].
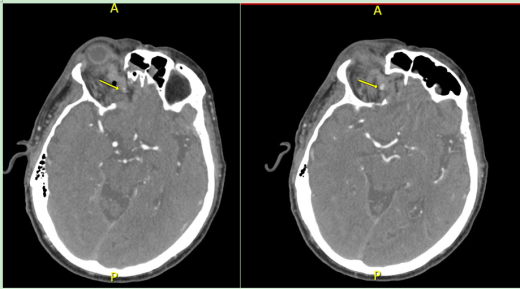
CT Head, CT Angiogram
When patient first presents to the emergency room, CT head without contrast and CT angiogram are helpful in identifying intracranial bleeding and vascular lesions. CTA of the head and the neck are also helpful in identifying vascular injuries.
Based on past literature and ED triaging experience, pseudoaneurysm may expand quickly in its early phase of development, which may mimic an expanding hematoma. [11] However, the precise timing of OAPA progression may not manifest until up to 24 hours after the initial injury. Follow-up imaging will be helpful in monitoring the size of progression and determining next step management. Unlike hematomas, pseudoaneurysms will stabilize in size without active contrast extravasation. [11]
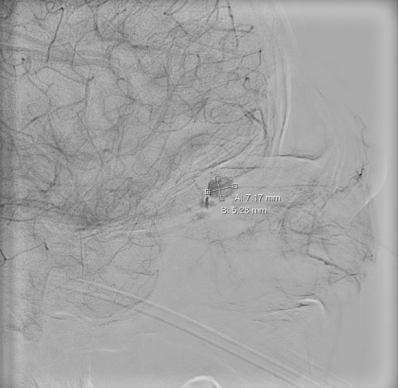
MRI, MRA, MRV, and Angiography
Patients with suspected OAPA typically require neuro-ICU level of care. Follow-up advanced imaging such as MRI, MRA, and/or MRV are helpful in confirming the diagnosis and identifying the source of the lesion. Based on past literature research, MRI, MRA, and MRV are all reasonable diagnostic imaging studies for these types of scenarios. Digital subtraction angiography is the most confirmatory imaging yet most invasive. It will help to visualize the lesion in real-time with detailed information on size and hemodynamics. Angiography can be both diagnostic and curative to OAPA. However, it is imperative to engage in thorough discussions about prognosis and complications with patients, as the location of these pseudoaneurysms is in proximity to the central retinal artery, and embolization procedures may carry the risk of permanent vision loss.
Management
Neuro-Intervention (Endovascular Occlusion)
Prompt endovascular occlusion can prevent complications such as enlargement, hemorrhage, and hematoma formation.[11] This can be achieved by microcatheterization and coil embolization.[7] The process involves navigating an endovascular wire close to the OAPA, followed by the use of a microcatheter to deliver the coil or glue for embolization. Subsequent angiography confirms the completion of coil embolization. These procedures have demonstrated considerable success in occluding OAPA and preventing vision loss, as outlined in the final literature summary table.
If the lesion site is near the origin site of the internal carotid artery, endovascular balloon embolization can be attempted, though this was mostly performed before the availability of coiling. [12] If the proximal ophthalmic artery becomes occluded, branches of the external carotid artery can potentially provide collateral blood flow to the visual system through anastomoses with the extra-orbital branches of the ophthalmic artery.[10] However, there is a risk of permanent vision loss. [13] Additionally, innovative materials have been explored in the occlusion process. One study reported a case of OAPA presenting with persistent epistaxis after removal of a nasogastric tube.[4] This patient was treated with 25% glue (NBCA) injection to embolize the lesion.
Surgery, External Approach
Other than endovascular approach, there have also been limited reported cases of external surgical approaches to surgically remove the pseudoaneurysms. There have been only two reported cases of external surgical approach completed in China and Japan [2]. The surgery in China was performed on a patient who suffered blunt trauma (punch) to the orbit. The surgeons were able to successfully remove the pseudoaneurysm by entering through right cranio-orbital approach with orbital decompression. However, due to the degree of injury to the globe and optic nerve, visual acuity remained at NLP with total ophthalmoplegia [2]. The case in Japan was also performed on a patient who sustained closed head injury from motor vehicle accident. The surgeons were successfully able to resect the pseudoaneurysm through extradural approach. However, visual acuity remained at NLP after surgery.
Conservative Management
At this time there has been one recorded conservative management case in approaching OAPA, which was done at UMass Memorial Medical Center. Through a multi-disciplinary care approach involving ophthalmology, neuro-intervention, and neuro-critical care, the patient's pseudoaneurysm self-embolized 72 hours later as demonstrated by serial CT angiogram scans.
Prognosis
OAPAs are dangerous because they can enlarge over time and eventually rupture, resulting in intracranial hemorrhage or hematoma formation.[11] Pseudoaneurysm of the dural portion of the ophthalmic artery can result in subarachnoid hemorrhage with a high risk of re-hemorrhage if left untreated.[7]
Outcomes
Endovascular occlusion cases may have visual improvement with a low rate of central retinal artery occlusion. Timely management of these pseudoaneurysms may successfully reduce the rate of intracranial bleeding and mortalities. Current literature shows a 0% mortality rate among patients with OAPA managed surgically. However, should the initial trauma injury cause significant globe or optic nerve injury, visual outcome may be poor, and patients may eventually require evisceration or enucleation (please refer to the final literature summary table).
Complications
For patients who have undergone successful endovascular embolization, common complications include ptosis and vasospasm. For patients who undergo interventions, but do not recover vision, corneal edema, pain, and proptosis are the most common symptoms. [3]
Cranial nerves are also susceptible to injuries even after pseudoaneurysm embolization or self-embolization, though this effect may be transient. For the one patient who underwent serial CT angiogram monitoring at the University of Massachusetts Memorial Hospital, complete cranial nerve 3 palsy with persistent traumatic pupil of the injured eye was discovered on follow-up 1 month later. The exact etiology of the palsy was unclear but may have been related to transient compression after the traumatic injury. The CN3 palsy spontaneously resolved over about three months; however, the traumatic pupil persisted, and visual acuity only recovered to 20/70 (the unaffected eye was 20/30). Given the patient’s age and cardiovascular risk factors, the decision was made to closely monitor without any more procedural intervention.
Literature Summary
Below is the table listing past literature discussing OAPA, including treatment approaches, surgical outcomes, and complications.
| Studies/Cases | Case size | Year | Types of injury | Location of OAPA | Management | Ophthalmic Complications | Ophthalmic Outcome |
| Czyz C, et al.[3] | 1 | 2017 | Penetrating bullet intra-orbital | Right ophthalmic artery | Endovascular occlusion coiling | Corneal edema, hyphema, hemorrhagic chemosis | NLP, evisceration |
| Chun H, et al.[11] | 1 | 2007 | Motor vehicle accident, blunt head trauma | Extra-cranial, left ethmoid branch | Endovascular occlusion coiling | None | Intervention induced vasospasm, self-sealed |
| Balushi AA, et al.[6] | 1 | 2017 | Penetrating bullet intra-orbital | Bilateral ophthalmic artery | Endovascular occlusion coiling | None | Clinically stable |
| Kelly ME, et al.[8] | 1 | 2009 | Bicycle accident, blunt head trauma | Right ophthalmic artery | Endovascular occlusion coiling | Failed first attempt | Clinically stable |
| Rosssitti S, et al. [14] | 1 | 2009 | Non-trauma, progressive vision loss | Right ophthalmic artery | Endovascular occlusion coiling | None | Clinically stable |
| Li Y, et al.[2] | 1 | 2017 | Fist fight, blunt head trauma | Right ophthalmic artery | External surgical resection | None | NLP, ophthalmoplegia |
| Dolati-Ardejani P, et al.[13] | 1 | 2012 | Fall, blunt head trauma | Right ophthalmic artery | Endovascular embolization coiling | Failed procedure, occlusion of the proximal OphA | NLP |
| Liao Zb, et al.[9] | 1 | 2023 | Motor vehicle accident, blunt head trauma | Right ophthalmic artery | Endovascular occlusion coiling | None | Clinically stable |
| Selcuk H, et al. [4] | 1 | 2005 | Nasogastric tube placement | Left ophthalmic artery | Endovascular occlusion (NBCA-histoacryl (25%) injection) | None | Clinically stable |
| Kikkawa Y, et al. [15] | 1 | 2012 | Closed head injury | Left ophthalmic artery | External surgical resection | None | NLP |
| Kanazawa R, et al. [16] | 1 | 2011 | Fall, blunt head injury | Left ophthalmic artery | Endovascular occlusion coiling | Redo in 5 months | Clinically stable |
| Hopkins JK, et al. [17] | 1 | 2007 | Unclear | Ophthalmic artery | Endovascular occlusion coiling | Unclear | Unclear |
| Shim YS [18] | 1 | 2021 | Fall, blunt head injury | Right ophthalmic artery origin site | Endovascular occlusion coiling | None | Clinically stable |
| Deshmukh YR, et al. [19] | 1 | 2005 | Iatrogenic, endovascular coil migration | Left ophthalmic artery near aneurysm rupture site | Surgical ligation | Vasospasm, cerebral edema | Neurologically intact without focal neuro deficit |
| Colewell L, Ren Y, et al. UMass Memorial Case (case not yet published) | 1 | 2023 | Fall, blunt trauma | Right mid-ophthalmic artery | Conservative observation | Ptosis, traumatic pupil, transient CN3 palsy | Clinically stable, visual acuity 20/70 in OD |
References
- ↑ Peick AL, Nichols WK, Curtis JJ, Silver D. Aneurysms and pseudoaneurysms of the superficial temporal artery caused by trauma. J Vasc Surg. 1988;8(5):606-610.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 Li Y, Song WX, Zhang TM, Fu JD, Sun S, Zhao JZ. Intraorbital traumatic ophthalmic artery aneurysm: case report. Neurol India. 2012 Nov-Dec;60(6):657-60. doi: 10.4103/0028-3886.105213. PMID: 23287341.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 Czyz CN, Piehota PG, Strand AT, Stein M. Post-traumatic ophthalmic artery pseudoaneurysm from orbital projectile. Can J Ophthalmol. Aug 2017;52(4):e130-e132. doi:10.1016/j.jcjo.2016.12.007
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Selcuk H, Soylu N, Albayram S, et al. Endovascular treatment of persistent epistaxis due to pseudoaneurysm formation of the ophthalmic artery secondary to nasogastric tube. Cardiovasc Intervent Radiol. 2005;28(2):242-5. doi:10.1007/pl00021048
- ↑ Patil NS, Kumar AH, Pamecha V, et al. Cystic artery pseudoaneurysm-a rare complication of acute cholecystitis: review of literature. Surg Endosc. Feb 2022;36(2):871-880. doi:10.1007/s00464-021-08796-1
- ↑ Jump up to: 6.0 6.1 Al Balushi A, Kitchener J, Edgell RC. Bilateral ophthalmic artery dissecting aneurysms presenting with recurrent epistaxis. J Vasc Interv Neurol. 2017 Jan;9(3):14-16. PMID: 28243345; PMCID: PMC5317286.
- ↑ Jump up to: 7.0 7.1 7.2 Kelly ME, Fiorella D. Traumatic ophthalmic artery pseudoaneurysm coiled with a steerable microcatheter. Can J Neurol Sci. Jul 2009;36(4):496-9. doi:10.1017/s0317167100007861
- ↑ Jump up to: 8.0 8.1 Kelly ME, Fiorella D. Traumatic ophthalmic artery pseudoaneurysm coiled with a steerable microcatheter. Can J Neurol Sci. 2009 Jul;36(4):496-9. doi: 10.1017/s0317167100007861. PMID: 19650364.
- ↑ Jump up to: 9.0 9.1 Liao, Z., Long, X., & Li, J. (2023). Endovascular treatment of pseudoaneurysm of ophthalmic artery with carotid-cavernous fistula: A case report. Interdisciplinary Neurosurgery, 101889.
- ↑ Jump up to: 10.0 10.1 Hopkins JK, Shaibani A, Ali S, et al. Coil embolization of posttraumatic pseudoaneurysm of the ophthalmic artery causing subarachnoid hemorrhage. Case report. J Neurosurg. Nov 2007;107(5):1043-6. doi:10.3171/JNS-07/11/1043
- ↑ Jump up to: 11.0 11.1 11.2 11.3 11.4 Chun HJ, Yi HJ. Traumatic extracranial pseudoaneurysm on the peripheral ophthalmic artery presenting as delayed intraparenchymal hematoma: case report. Surg Neurol. 2009 Jun;71(6):701-704. doi:10.1016/j.surneu.2007.11.018.
- ↑ Tantana S, Pilla TJ, Awwad EE, Smith KR. Balloon embolization of a traumatic carotid-ophthalmic pseudoaneurysm with control of the epistaxis and preservation of the internal carotid artery. AJNR Am J Neuroradiol. 1987 Sep-Oct;8(5):923-924. PMID: 3118688; PMCID: PMC8334483.
- ↑ Jump up to: 13.0 13.1 Dolati-Ardejani, P., Morrish, W. F., & Wong, J. H. (2012). Posttraumatic Ophthalmic Artery Pseudoaneurysm Presenting Epistaxis: Case Report and Review of the Literature. Journal of Neurological Surgery Part B: Skull Base, 73(S 01), A286.
- ↑ Rossitti S, Radzinska R, Vigren P, Hillman J. Postoperative ophthalmic artery pseudoaneurysm presenting as monocular blindness: successful endovascular treatment. Klin Neuroradiol. 2009 Aug;19(3):230-234. doi: 10.1007/s00062-009-9003-2. Epub 2009 Jun 19. PMID: 19727584.
- ↑ Kikkawa Y, Natori Y, Sasaki T. Delayed post-traumatic pseudoaneurysmal formation of the intracranial ophthalmic artery after closed head injury. Case report. Neurol Med Chir (Tokyo). 2012;52(1):41-43. doi: 10.2176/nmc.52.41. PMID: 22278026.
- ↑ Kanazawa R, Ishihara S, Neki H, Okawara M, Ishihara H, Kohyama S, et al. Embolization Using Endovascular Technique in Acute and Chronic Stages of Traumatic Ophthalmic Artery Aneurysm—Case Report—. Neurol Med Chir (Tokyo). 2011;51(4):289-292.
- ↑ Hopkins JK, Shaibani A, Ali S, Khawar S, Parkinson R, Futterer S, Russell EJ, Getch C. Coil embolization of posttraumatic pseudoaneurysm of the ophthalmic artery causing subarachnoid hemorrhage. Case report. J Neurosurg. 2007 Nov;107(5):1043-1046. doi: 10.3171/JNS-07/11/1043. PMID: 17977280.
- ↑ Shim YS. Coil Embolization of Traumatic Ophthalmic Artery Aneurysm: Case Report. Korean J Neurotrauma. 2021 Nov 12;18(1):98-102. doi: 10.13004/kjnt.2022.18.e2. PMID: 35557629; PMCID: PMC9064747.
- ↑ Deshmukh VR, Klopfenstein JM, Albuquerque FC, Kim LJ, Spetzler RF. Surgical Management of Distal Coil Migration and Arterial Perforation after Attempted Coil Embolization of a Ruptured Ophthalmic Artery Aneurysm: Technical Case Report. Oper Neurosurg. 2006 Apr;58(4):ONS-E379. doi: 10.1227/01.NEU.0000205317.27820.35.


