Conjunctivochalasis: Difference between revisions
No edit summary |
m (Text replacement - "== Clinical diagnosis ==" to "== Clinical Diagnosis ==") |
||
| (11 intermediate revisions by 4 users not shown) | |||
| Line 2: | Line 2: | ||
|Authors=Luis.I.Larrazabal | |Authors=Luis.I.Larrazabal | ||
|Category=Cornea/External Disease | |Category=Cornea/External Disease | ||
|Assigned editor= | |Assigned editor=Sarah.Brown.Weissbart | ||
|Reviewer= | |Reviewer=Sarah.Brown.Weissbart | ||
|Date reviewed= | |Date reviewed=February 19, 2024 | ||
|Article status=Up to Date | |Article status=Up to Date | ||
}} | }} | ||
| Line 20: | Line 20: | ||
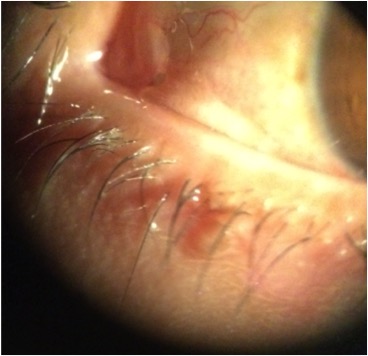
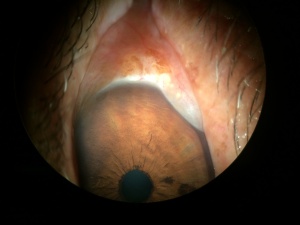
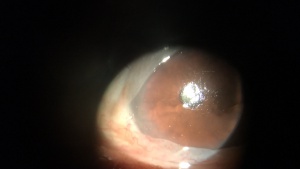
[[File:Dr.A.Ibarra.Conjunctivochalasis.JPG|thumb|Mild-Severe Conjunctivochalasis]] | [[File:Dr.A.Ibarra.Conjunctivochalasis.JPG|thumb|Mild-Severe Conjunctivochalasis]] | ||
Conjunctivochalasis is defined as a redundant, nonedematous conjunctiva that | Conjunctivochalasis (CCH) is defined as a loose, redundant, nonedematous conjunctiva that is considered to occur secondary to normal aging. At times CCH may be asymptomatic and, therefore, is sometimes overlooked by the physician. However, CCH can be a possible origin of ocular surface irritation and tearing. When severe, CCH can also lead to blurred vision, mucous discharge, dryness, ocular fatigue, and [[Subconjunctival_Hemorrhage|subconjunctival hemorrhage]]. | ||
CCH is usually bilateral and most commonly involves the inferotemporal conjunctiva. | |||
= Disease Entity = | = Disease Entity = | ||
Conjunctivochalasis | Conjunctivochalasis (CCH) | ||
== Disease == | == Disease == | ||
| Line 43: | Line 35: | ||
== Etiology == | == Etiology == | ||
Etiology is uncertain but is likely associated with age or eye rubbing (i.e. [[Allergic_Conjunctivitis|allergic conjunctivitis]]). | |||
== Risk Factors == | == Risk Factors == | ||
Risk factors for CCH include age, eye rubbing, ocular surface disease, [[Allergic_Conjunctivitis|allergic conjunctivitis]], dry eye, contact lens wear, [[Hyperopia|hyperopia]], [[Pinguecula|pinguecula]], UV exposure, eyelid disorders, and thyroid disease. <ref>Marmalidou A, Kheirkhah A, Dana R. Conjunctivochalasis: a systematic review. Surv Ophthalmol 2018;63:554-564.</ref> | |||
== General Pathology == | == General Pathology == | ||
== Pathophysiology == | == Pathophysiology == | ||
The etiology of conjunctivochalasis has not been completely elucidated. In a prospective clinical and histopathological study of 29 patients, 22 showed demonstrated normal conjunctival histology, while 4 specimens revealed inflammatory changes, and 3 specimens showed elastosis. The authors concluded and hypothesized that the etiology is multifactorial, including local trauma, UV radiation and delayed tear clearance as triggers of the disease. <ref>Chan DG, Francis IC, Filipic M, Coroneo MT, Yong J. Clinicopathologic study of conjunctivochalasis. Cornea 24(5):634, 2005.</ref> | |||
Watanabe et al. demonstrated subconjunctival microscopic telangiectasia in 4 of 39 specimens taken from patients with severe conjunctivochalasis, with no evidence of inflammation. They also noted fragmented elastic fibers and sparse assemblages of collagen fibers in 44 specimens. They concluded that mechanical forces between the lower eyelid and conjunctiva gradually impaired lymphatic flow, resulting in lymphatic dilation and clinically redundant conjunctiva. <ref name="Watanabe">Watanabe A, Yokoi N, Kinoshita S, Hino Y, Tsuchihashi Y. Clinicopathologic study of conjunctivochalasis. Cornea 23(3):294-8, 2004.</ref> | Watanabe et al. demonstrated subconjunctival microscopic telangiectasia in 4 of 39 specimens taken from patients with severe conjunctivochalasis, with no evidence of inflammation. They also noted fragmented elastic fibers and sparse assemblages of collagen fibers in 44 specimens. They concluded that mechanical forces between the lower eyelid and conjunctiva gradually impaired lymphatic flow, resulting in lymphatic dilation and clinically redundant conjunctiva. <ref name="Watanabe">Watanabe A, Yokoi N, Kinoshita S, Hino Y, Tsuchihashi Y. Clinicopathologic study of conjunctivochalasis. Cornea 23(3):294-8, 2004.</ref> | ||
Even though there is little to no histopathologic evidence to support inflammation as a major contributor to conjunctivochalasis, mechanistic evidence suggests a shift in the normal balance of the conjunctival matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs). | Even though there is little to no histopathologic evidence to support inflammation as a major contributor to conjunctivochalasis, mechanistic evidence suggests a shift in the normal balance of the conjunctival matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs). | ||
Li et al. showed overexpression of MMP-1 and MMP-3 | Li et al. showed overexpression of MMP-1 and MMP-3 mRNA in tissue cultured conjunctivochalasis fibroblasts, versus normal human conjunctival fibroblasts. Further studies showed that inflammatory mediators TNF-å and IL-1ß may increase the expression of MMP-1 and MMP-3 in conjunctivochalasis fibroblasts. Other inflammatory cytokines were also found in increased amounts in tear film of patients with conjunctivochalasis (IL6 and IL8). After these observations, the authors concluded that the disrupted interaction of MMPs and their inhibitors may lead to a manifestation of a redundant and lax conjunctiva. <ref>Li DQ, Meller D, Liu Y, Tseng SC. Overexpression of MMP-1 and MMP-3 by cultured conjunctivochalasis fibroblasts. Invest Ophthalmol Vis Sci 2000;41(2):404-410.</ref> | ||
Huang et al. studied whether conjunctivochalasis interferes with tear flow from the fornix to the tear meniscus and depletes the fornix tear reservoir. | Huang et al. studied whether conjunctivochalasis interferes with tear flow from the fornix to the tear meniscus and depletes the fornix tear reservoir. In this study of 24 patients with conjunctivochalasis (8 asymptomatic and 16 symptomatic), 9 pateints underwent operative correction.<ref>Huang, Y; Sheha, H; Tseng, S. ”Conjunctivochalasis Interferes with Tear Flow from Fornix to Tear Meniscus” (2013). Ophthalmology. 120:1681-1687. Elsevier.</ref> The study found that the recovery rate of the tear meniscus was significantly slower in symptomatic than asymptomatic patients when compared to normal subjects. Deepening of the inferior fornix by removing degenerated Tenon’s and performing a fornix reconstruction with amniotic membrane improved the recovery rate in symptomatic patients. The authors concluded that the tear reservoir in the fornix rapidly replenishes the meniscus under normal circumstances, so in patients with conjunctivochalasis, there is impaired formation of the normal tear meniscus as well as limitations in normal tear movement from the fornix. | ||
== Primary | == Primary Prevention == | ||
Patients may avoid eye rubbing and UV exposure and can treat any underlying ocular surface issues. CCH occurs largely secondary to age, however, so preventative strategies are limited. | |||
= Diagnosis = | = Diagnosis = | ||
| Line 73: | Line 64: | ||
== History == | == History == | ||
Patients often describe insidious onset of [[Ocular_Discomfort|ocular discomfort]], foreign body sensation, dryness, and tearing. Some patients have been treated for dry eye with limited improvement. | |||
== Physical | == Physical Examination == | ||
Slit lamp biomiocroscopy | Slit lamp biomiocroscopy reveals a prolapse of the conjunctiva over the lower lid margin in temporal, medial or nasal regions, in some cases occluding the inferior puncta resulting in epiphora and even blurred vision. | ||
== Signs == | == Signs == | ||
Signs on examination include redundant conjunctiva that overlaps eyelid margin, especially over the inferior temporal region. Also, the conjunctiva is easily mobilized by pressing on the eyelid and moving the loose conjunctiva up and down. | |||
== Symptoms == | == Symptoms == | ||
Symptom onset can be insidious, and patients may be misdiagnosed with dry eye or other ocular surface conditions. Symptoms include foreign body sensation, burning, dry eyes and discomfort, many of which result from a disruption of the inferior tear meniscus and, thus, an unstable tear film. | |||
The diagnosis is clinical | == Clinical Diagnosis == | ||
The diagnosis is clinical. | |||
== Diagnostic procedures == | == Diagnostic procedures == | ||
| Line 96: | Line 88: | ||
== Laboratory testing == | == Laboratory testing == | ||
As a result of tear circulation | As a result of disrupted tear circulation, changes in tear osmolarity may be observed but are not necessary for the diagnosis. | ||
== Differential diagnosis == | == Differential diagnosis == | ||
Dry eye | [[Dry_Eye_Syndrome|Dry eye syndrome]], [[Dry_Eye_in_Sjogren%27s_Syndrome|Sjögren syndrome]], [[Meibomian_Gland_Dysfunction_(MGD)|meibomian gland dysfunction]], [[Blepharitis|blepharitis]], [[Allergic_Conjunctivitis|allergic conjunctivitis]] | ||
= Management = | = Management = | ||
== General treatment == | |||
Management should be individualized according to the severity and symptoms of each patient. No treatment is needed if the patient is asymptomatic. | |||
== Medical therapy == | == Medical therapy == | ||
Mild symptoms can be addressed with topical lubrication, blinking exercises, topical antihistamines, and topical corticosteroids. | |||
== Surgery == | == Surgery == | ||
Surgical therapy most commonly involves conjunctival excision, typically a semilunar portion of conjunctiva 5 mm posterior to the limbus. The conjunctiva can be closed with absorbable suture or with fibrin glue. Amniotic membrane can also be used to fill in the conjunctival defect. | |||
Thermal cautery can also be performed to tighten loose or redundant conjunctiva. Under topical subconjunctival anesthesia, the redundant conjunctiva is grasped gently with a forceps and thermal cautery is applied over this redundant conjunctiva to cause a contraction of the tissue. | |||
Forniceal reconstruction with amniotic membrane (discussed above) is another option for severe conjunctivochalasis in order to re-establish the forniceal tear reservoir. | |||
== Complications == | == Complications == | ||
Conjunctivochalasis can be complicated by dry eye symptoms and pain when severe. | |||
== Prognosis == | == Prognosis == | ||
Prognosis is good with proper diagnosis and treatment. | |||
= References = | = References = | ||
<references/> | <references/> | ||
<ol><li value=" | <ol><li value="6"> | ||
Holland, E; Mannis, M; Barry, W. “Ocular Surface Disease” (2013) Saunders Elsevier.</li></ol> | Holland, E; Mannis, M; Barry, W. “Ocular Surface Disease” (2013) Saunders Elsevier.</li></ol> | ||
Latest revision as of 09:10, April 3, 2025
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Conjunctivochalasis (CCH) is defined as a loose, redundant, nonedematous conjunctiva that is considered to occur secondary to normal aging. At times CCH may be asymptomatic and, therefore, is sometimes overlooked by the physician. However, CCH can be a possible origin of ocular surface irritation and tearing. When severe, CCH can also lead to blurred vision, mucous discharge, dryness, ocular fatigue, and subconjunctival hemorrhage.
CCH is usually bilateral and most commonly involves the inferotemporal conjunctiva.
Disease Entity
Conjunctivochalasis (CCH)
Disease
Conjunctivochalasis
Etiology
Etiology is uncertain but is likely associated with age or eye rubbing (i.e. allergic conjunctivitis).
Risk Factors
Risk factors for CCH include age, eye rubbing, ocular surface disease, allergic conjunctivitis, dry eye, contact lens wear, hyperopia, pinguecula, UV exposure, eyelid disorders, and thyroid disease. [1]
General Pathology
Pathophysiology
The etiology of conjunctivochalasis has not been completely elucidated. In a prospective clinical and histopathological study of 29 patients, 22 showed demonstrated normal conjunctival histology, while 4 specimens revealed inflammatory changes, and 3 specimens showed elastosis. The authors concluded and hypothesized that the etiology is multifactorial, including local trauma, UV radiation and delayed tear clearance as triggers of the disease. [2]
Watanabe et al. demonstrated subconjunctival microscopic telangiectasia in 4 of 39 specimens taken from patients with severe conjunctivochalasis, with no evidence of inflammation. They also noted fragmented elastic fibers and sparse assemblages of collagen fibers in 44 specimens. They concluded that mechanical forces between the lower eyelid and conjunctiva gradually impaired lymphatic flow, resulting in lymphatic dilation and clinically redundant conjunctiva. [3] Even though there is little to no histopathologic evidence to support inflammation as a major contributor to conjunctivochalasis, mechanistic evidence suggests a shift in the normal balance of the conjunctival matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs).
Li et al. showed overexpression of MMP-1 and MMP-3 mRNA in tissue cultured conjunctivochalasis fibroblasts, versus normal human conjunctival fibroblasts. Further studies showed that inflammatory mediators TNF-å and IL-1ß may increase the expression of MMP-1 and MMP-3 in conjunctivochalasis fibroblasts. Other inflammatory cytokines were also found in increased amounts in tear film of patients with conjunctivochalasis (IL6 and IL8). After these observations, the authors concluded that the disrupted interaction of MMPs and their inhibitors may lead to a manifestation of a redundant and lax conjunctiva. [4]
Huang et al. studied whether conjunctivochalasis interferes with tear flow from the fornix to the tear meniscus and depletes the fornix tear reservoir. In this study of 24 patients with conjunctivochalasis (8 asymptomatic and 16 symptomatic), 9 pateints underwent operative correction.[5] The study found that the recovery rate of the tear meniscus was significantly slower in symptomatic than asymptomatic patients when compared to normal subjects. Deepening of the inferior fornix by removing degenerated Tenon’s and performing a fornix reconstruction with amniotic membrane improved the recovery rate in symptomatic patients. The authors concluded that the tear reservoir in the fornix rapidly replenishes the meniscus under normal circumstances, so in patients with conjunctivochalasis, there is impaired formation of the normal tear meniscus as well as limitations in normal tear movement from the fornix.
Primary Prevention
Patients may avoid eye rubbing and UV exposure and can treat any underlying ocular surface issues. CCH occurs largely secondary to age, however, so preventative strategies are limited.
Diagnosis
Clinical
History
Patients often describe insidious onset of ocular discomfort, foreign body sensation, dryness, and tearing. Some patients have been treated for dry eye with limited improvement.
Physical Examination
Slit lamp biomiocroscopy reveals a prolapse of the conjunctiva over the lower lid margin in temporal, medial or nasal regions, in some cases occluding the inferior puncta resulting in epiphora and even blurred vision.
Signs
Signs on examination include redundant conjunctiva that overlaps eyelid margin, especially over the inferior temporal region. Also, the conjunctiva is easily mobilized by pressing on the eyelid and moving the loose conjunctiva up and down.
Symptoms
Symptom onset can be insidious, and patients may be misdiagnosed with dry eye or other ocular surface conditions. Symptoms include foreign body sensation, burning, dry eyes and discomfort, many of which result from a disruption of the inferior tear meniscus and, thus, an unstable tear film.
Clinical Diagnosis
The diagnosis is clinical.
Diagnostic procedures
OCT images from the anterior segment may be helpful to evaluate the tear meniscus and gross anatomy of the lateral canthus.
Laboratory testing
As a result of disrupted tear circulation, changes in tear osmolarity may be observed but are not necessary for the diagnosis.
Differential diagnosis
Dry eye syndrome, Sjögren syndrome, meibomian gland dysfunction, blepharitis, allergic conjunctivitis
Management
General treatment
Management should be individualized according to the severity and symptoms of each patient. No treatment is needed if the patient is asymptomatic.
Medical therapy
Mild symptoms can be addressed with topical lubrication, blinking exercises, topical antihistamines, and topical corticosteroids.
Surgery
Surgical therapy most commonly involves conjunctival excision, typically a semilunar portion of conjunctiva 5 mm posterior to the limbus. The conjunctiva can be closed with absorbable suture or with fibrin glue. Amniotic membrane can also be used to fill in the conjunctival defect.
Thermal cautery can also be performed to tighten loose or redundant conjunctiva. Under topical subconjunctival anesthesia, the redundant conjunctiva is grasped gently with a forceps and thermal cautery is applied over this redundant conjunctiva to cause a contraction of the tissue.
Forniceal reconstruction with amniotic membrane (discussed above) is another option for severe conjunctivochalasis in order to re-establish the forniceal tear reservoir.
Complications
Conjunctivochalasis can be complicated by dry eye symptoms and pain when severe.
Prognosis
Prognosis is good with proper diagnosis and treatment.
References
- ↑ Marmalidou A, Kheirkhah A, Dana R. Conjunctivochalasis: a systematic review. Surv Ophthalmol 2018;63:554-564.
- ↑ Chan DG, Francis IC, Filipic M, Coroneo MT, Yong J. Clinicopathologic study of conjunctivochalasis. Cornea 24(5):634, 2005.
- ↑ Watanabe A, Yokoi N, Kinoshita S, Hino Y, Tsuchihashi Y. Clinicopathologic study of conjunctivochalasis. Cornea 23(3):294-8, 2004.
- ↑ Li DQ, Meller D, Liu Y, Tseng SC. Overexpression of MMP-1 and MMP-3 by cultured conjunctivochalasis fibroblasts. Invest Ophthalmol Vis Sci 2000;41(2):404-410.
- ↑ Huang, Y; Sheha, H; Tseng, S. ”Conjunctivochalasis Interferes with Tear Flow from Fornix to Tear Meniscus” (2013). Ophthalmology. 120:1681-1687. Elsevier.
- Holland, E; Mannis, M; Barry, W. “Ocular Surface Disease” (2013) Saunders Elsevier.