Wavefront Testing
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Ocular refraction can be determined with a technique called "subjective refraction", which requires the patient's collaboration, and/or with the "objective refraction" technique. This method does not require any input from the patient: instead, instruments such as Retinoscopy, Auto-refractometer and Aberrometer are used to calculate objectively the refraction.
Objective refraction can be performed with static retinoscopy, which requires cycloplegia, or dynamic retinoscopy; both require the judgment of a human operator to determine the refractive error. Retinoscopy performed by an experienced clinician has been found to provide a more accurate estimation of refractive error than autorefraction[1].
The autorefractor can be employed with or without cycloplegia: the use of cycloplegic eyedrops makes the auto-refractometer a valid alternative to retinoscopy [2].
The aberrometer is a very reliable and operator-independent instrument to obtain an accurate objective refraction, which is extremely important in planning refractive surgery with some platforms. Wavefront mapping is a technology that makes custom laser eye surgery possible by precisely measuring and diagramming the aberrations of an optical system (e.g. the human eye). These aberrations are divided into lower-order aberrations (such as myopia, hyperopia, and astigmatism) and higher-order aberrations (such as trefoil, coma, and spherical aberration) that affect contrast sensitivity and night vision. The main advantage of the aberrometer, over the previously cited methods, is that it can detect both lower and higher-order aberrations, whereas retinoscopy and autorefraction techniques are based only on lower-order aberrations.
There are two different forms of wavefront mapping . Wavefront-optimized treatment ablations improve the postoperative corneal shape by taking the curvature of the cornea into account and increasing the number of peripheral pulses; this approach minimizes the induction of higher-order aberrations. Wavefront-guided ablation uses information obtained from a wavefront-sensing aberrometer (which quantifies the aberrations) that are transferred electronically to the treatment laser to program the ablation. This is distinct from conventional excimer laser and wavefront-optimized laser treatments, in which the subjective refraction is used to program the laser ablation. Wavefront-guided technology is used in CustomVue laser eye surgery to correct refractive error and mitigate symptoms previously seen with conventional excimer ablations. Results of wave-front guided compared to wave-front optimized ablations are comparable.[3]
History of Wavefront Technology
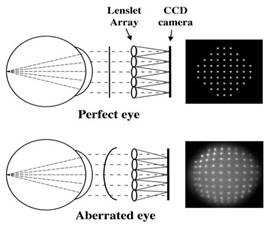
Wavefront technology was originally developed for use in astronomy. In the 1900s, an astrophysicist named Johannes Hartmann devised a method of measuring the ray aberrations of mirrors and lenses. The Hartmann test used a metal disk in which regularly spaced holes had been drilled. The disk or screen was then placed over the mirror that was to be tested and a photographic plate was placed near the focus of the mirror. When exposed to light, a perfect mirror will produce an image of regularly spaced dots. If the mirror does not produce regularly spaced dots, the irregularities, or aberrations of the mirror, can be determined.
Source: Image from the Center for Visual Sciences, University of Rochester
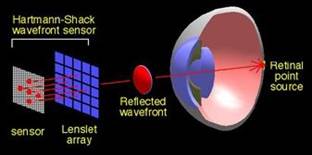
In the 1970s, Dr. Roland Shack and Dr. Ben Platt advanced the concept by replacing the screen with a sensor based on an array of tiny lenslets, thus creating the Hartmann-Shack sensor. In 1978, Dr. Josef Bille of Germany was the first person to use the Hartmann-Shack sensor in ophthalmology. Other wavefront pioneers include Dr. Junzhong Liang and Dr. David Williams who developed a wavefront device that could be used in a clinical setting.
Source: Image from ASIC Laboratory Heidelberg
In 1997, Drs. Liang and Williams presented a paper at the Association for Research in Vision and Ophthalmology that discussed the early clinical results attained with the wavefront device. At this time, ophthalmologists and major laser manufacturers, such as VISX, Bausch & Lomb, and Alcon, began to look at the possibilities of wavefront technology for correcting refractive error and to develop their own wavefront analyzers. In 2002, the FDA approved the first wavefront-guided custom LASIK application. Today, there are many integrated wavefront-guided LASIK systems that first generate a map of a patient’s unique optical aberrations, then send this information to an excimer laser that performs the wavefront-guided LASIK procedure.
Types of Wavefront Sensing
Outgoing wavefront aberrometry
- Hartmann-Shack sensor
Ingoing wavefront aberrometry
Retinal image aberrometry
- Tscherning aberrometer
- Tracey retinal ray tracing
Double-pass aberrometry
- Slit skialoscopy
Ingoing subjective adjustable aberrometry
- Spatially resolved Refractometry
Higher-order aberrations can have a significant impact on quality of vision and are often linked to glare and halos that may cause night vision problems. Wavefront analyzers often use a Hartmann-Shack sensor, which maps both lower and higher-order aberrations by projecting waves of light into a patient's eye and mapping the waves that bounce back through the pupil. A perfect wavefront would be completely flat. When light rays enter the eye and traverse the different refractive indices, the wavefront surface changes, taking on a shape unique to that eye. These variations are called wavefront aberrations.
Depending on the instrument, an operator can detect a corneal wavefront, an internal wavefront or a total wavefront (corneal+internal).
Wavefront Analysis
The aberration data is collected and then converted into a treatment formula by using Zernike polynomials, which are also called modes. Each mode describes a certain three-dimensional surface and the Zernike polynomials correspond with ocular aberrations. For instance, second-order Zernike polynomials represent the conventional aberrations such as defocus and astigmatism. Zernike polynomials above the second order represent the higher-order aberrations that are suspected of causing glare and decreased contrast sensitivity. Zernike polynomials help to simplify the wavefront technology by combining all aberrations into one simple map. This is called Zernike decomposition.
Zernike Polynomials Shapes
The wavefront analyzer software condenses the wavefront information into a conventional refraction in diopters as well as in Zernike form. This map is then transferred to the laser, enabling treatment of the patient’s lower and higher order aberrations.
Other software include the possibility to analyze data via a Fourier transform-based algorithm. The Fourier series is an infinite expansion that can be used to represent any complex shape (such as a wave aberration) by breaking it into its frequency components. In this case, both lower and higher-order aberrations can be decomposed in the so called "Fourier transformation".
The two methods are comparable in lower-order aberrations but disagree in higher-order aberrations[4].
Clinical Study Results
Some of the early trial results, such as the 2003 VISX multi-center clinical study, that led to FDA approval for wavefront-guided laser vision correction showed the following:
- At one year after the VISX CustomVue procedure:
- 100% of the clinical study participants could pass a state-issued driving test without glasses or contacts
- 98% of the clinical study participants could see 20/20 or better without glasses or contacts
- 70% of the clinical study participants could see 20/16 or better without glasses or contacts
- Four times as many clinical study participants were very satisfied with their night vision after the VISX CustomVue procedure compared to their night vision before with glasses or contacts.
Both wavefront-guided and wavefront-optimized treatment profiles can be used to provide excellent improvement in vision.[5]
References
- ↑ Jorge J, Queirós A, Almeida JB, Parafita MA. Retinoscopy/autorefraction: which is the best starting point for a noncycloplegic refraction? Optom Vis Sci. 2005 Jan;82(1):64-8. PMID: 15630406.
- ↑ Hashemi H, Khabazkhoob M, Asharlous A, Yekta A, Emamian MH, Fotouhi A. Overestimation of hyperopia with autorefraction compared with retinoscopy under cycloplegia in school-age children. Br J Ophthalmol. 2018 Dec;102(12):1717-1722. doi: 10.1136/bjophthalmol-2017-311594. Epub 2018 Feb 13. PMID: 29439996.
- ↑ RK Sia, DS Ryan, RD Stutzman, JF Pasternak, JB Eaddy, LA Logan, MF Torres, and KS Bower. Wavefront-guided versus wavefront-optimized photorefractive keratectomy: Clinical outcomes and patient satisfaction. J Cataract Refractive Surgery. 2015 Oct;41(10):2152-64.
- ↑ Cade F, Cruzat A, Paschalis EI, Espírito Santo L, Pineda R. Analysis of four aberrometers for evaluating lower and higher order aberrations. PLoS One. 2013;8(1):e54990. doi: 10.1371/journal.pone.0054990. Epub 2013 Jan 22. PMID: 23349995; PMCID: PMC3551914.
- ↑ He L, Manche EE. Contralateral eye-to-eye comparison of wavefront-guided and wavefront-optimized photorefractive keratectomy: a randomized clinical trial. JAMA Ophthalmol. 2015 Jan;133(1):51-9. doi: 10.1001/jamaophthalmol.2014.3876. Erratum in: JAMA Ophthalmol. 2015 May;133(5):621. PMID: 25321951.