Vortex Vein Varix
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Vortex Vein Varicosis (VVV) are benign dilations of the vortex vein ampullae within the eye, presenting as unilateral or bilateral pouch-like structures at oblique meridians of the equator. They may lead to changes in the retinal pigment epithelium. They are typically asymptomatic, and detected incidentaly in association with ocular examinations due to other concerns. The etiology remains uncertain, with proposed mechanisms including kinking of the vortex vein, weaknesses in vessel walls, and fluctuations in intraocular pressure. Diagnosis relies on clinical examination, with dynamic funduscopy being a key diagnostic tool. Imaging modalities such as OCT and ICGA provide confirmatory evidence. Management primarily involves observation, with associated conditions treated accordingly. While generally associated with a favorable prognosis, complications such as suprachoroidal hemorrhage may occur. Further research is needed to elucidate the pathogenesis and optimize management strategies for vortex vein varices.
Disease Entity
Vortex Vein Varicosis (VVV) are benign dilations of the vortex vein ampullae within the eye, presenting as unilateral or bilateral pouch-like structures at oblique meridians of the equator. Although typically asymptomatic, they may lead to complications such as changes in the retinal pigment epithelium. The etiology remains uncertain, with proposed mechanisms including kinking of the vortex vein, weaknesses in vessel walls, and fluctuations in intraocular pressure. Diagnosis relies on clinical examination, with dynamic funduscopy being a key diagnostic tool. Imaging modalities such as OCT and ICGA provide confirmatory evidence. Management primarily involves observation, with associated conditions treated accordingly. While generally associated with a favorable prognosis, complications such as suprachoroidal hemorrhage may occur. Further research is needed to elucidate the pathogenesis and optimize management strategies for vortex vein varices.
Disease
Vortex vein varices are characterized by the dilation of vortex vein ampullae, benign elevations within the eye. Typically, they manifest as single unilateral or multiple bilateral brownish-red to gray-colored pouches or teardrops located at oblique meridians of the equator. While most varices range from 1 to 3 disc diameters in size, larger variants have been reported, with the larger ones potentially more prevalent in superior quadrants, particularly the supratemporal region.
The prevalence of physiologic vortex vein ampullae, which are present in about 44% of individuals, provides some context for understanding the occurrence of vortex vein varices. However, the prevalence specifically of dilated vortex vein varices is less well documented, given their rare and often incidental nature.
Vortex vein varices may be incidentally discovered in patients referred for follow-up after experiencing symptoms of posterior vitreous detachment (PVD). However, it is not believed that they are directly associated with floaters or photopsia. Although vortex vein varices generally do not cause symptoms, they can exert pressure on the underlying choriocapillaris, leading to changes in the retinal pigment epithelium (RPE). Depending on the individual's ocular background pathologies or surgical history, they may be associated with other signs or symptoms. Clinically, distinguishing them from chorioretinal pathologies requiring treatment or follow-up, as well as more serious conditions like tumors, is crucial.
Diagnosis of vortex vein varices is typically straightforward and involves clinical examination. They are more readily detected in myopic and lightly pigmented eyes. Digital compression or a 3-mirror examination can result in the diminished size or disappearance of varices. In cases where prompt diagnosis is challenging, further investigation with ultrasound B-scan, fluorescein angiography (FA)/indocyanine green angiography (ICG), or optical coherence tomography (OCT) scans may be necessary to confirm the diagnosis. Factors such as weaknesses in the extracellular matrix and vessel walls, along with low intraocular pressure or high external pressure compromising vortex vein drainage, may contribute to their development.
Etiology
The etiology of ocular vortex vein varices remains uncertain, although several potential causes have been proposed. One prevalent theory suggests that kinking of the extrascleral portion of the vortex vein, often induced by changes in gaze, could lead to the development of varices. Additionally, factors such as weaknesses in the extracellular matrix and vessel walls, along with fluctuations in intraocular pressure or external pressure, such as high venous pressure, may contribute to the formation of ocular vortex vein varices.[1].
Shields et al. have speculated that partial obstruction of the vortex vein by the superior or inferior oblique muscle might also contribute to the formation of varices. Other potential contributing factors could include gaze-evoked narrowing of the scleral emissary canal or increases in ocular venous pressure, such as those occurring during the prone position or with the Valsalva maneuver.[2] [3] [4] [5] [6] [7] [8]
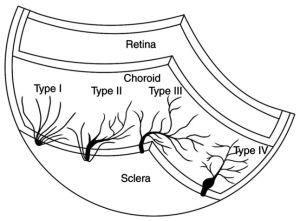
Various parameters, including the number, branch diameter, root area, location, type, and anastomosis of vortex veins, may contribute to the formation of vortex vein varices (VVV). It is speculated that type IV vortex veins (complete with ampulla) may be more prevalent in patients with VVV, but further investigation is needed to confirm this hypothesis.[9] See the image.
Despite the uncertainty surrounding the exact pathogenesis of vortex vein varices, their dynamic nature—illustrated by changes induced by gaze and pressure—can often aid in diagnosis. These changes can be further confirmed through ancillary testing methods.
Risk Factors
Risk factors for vortex vein varicosis may include a history of ocular trauma, low intraocular pressure, older age, myopia, and certain systemic conditions affecting vascular health. In addition to discussing vortex vein varicosis, a article reports on cases associated with scleritis.[10] These cases highlight a potential link between vortex vein varicosis and scleritis,[11] suggesting that scleral inflammation may contribute to or exacerbate the dilation and tortuosity of vortex veins. Further research is needed to fully understand the relationship between these two conditions and their implications for diagnosis and management.
General Pathology
Vortex vein varicosis involves structural changes in the vortex veins, leading to their abnormal dilation, tortuosity, and sometimes incompetence in draining choroidal blood.
Pathophysiology
The pathophysiology of vortex vein varicosis revolves around the impairment of normal venous drainage from the choroid, resulting in choroidal congestion, venous stasis, and potential complications such as suprachroidal choroidal hemorrhage.[12][13]
Primary Prevention
Primary prevention strategies for vortex vein varices involve minimizing factors that may contribute to their development. While the exact causes of vortex vein varices are not fully understood, maintaining stable intraocular pressure and avoiding activities that increase external pressure, such as the Valsalva maneuver, may be beneficial. Additionally, maintaining overall eye health through regular eye examinations and managing underlying conditions that may affect ocular blood flow or vessel integrity could potentially reduce the risk of developing vortex vein varices. However, specific primary prevention measures tailored specifically for vortex vein varices may require further research and investigation.
History
The history of vortex vein varices often involves the recognition of characteristic signs and symptoms during clinical evaluation. Patients may present with complaints related to visual disturbances or may be asymptomatic, with the condition discovered incidentally during routine eye examinations or evaluations for other ocular conditions.
A detailed medical history is essential to identify any underlying risk factors or associated conditions that may contribute to the development of vortex vein varices. Factors such as previous ocular surgeries, ocular trauma, or systemic conditions known to affect ocular vasculature may be relevant.
Patients may also report symptoms such as floaters or photopsia, although these symptoms are not typically associated with vortex vein varices. However, their presence may prompt further investigation to rule out other retinal or choroidal pathologies.
Additionally, documenting the duration and progression of symptoms, if present, can provide valuable insights into the course of the condition and help guide management decisions.
A thorough understanding of the patient's ocular and medical history, combined with careful clinical evaluation, contributes to the accurate diagnosis and management of vortex vein varices.
Physical examination
Diagnosis of vortex vein varices is typically straightforward and involves clinical examination. They are more readily detected in myopic and lightly pigmented eyes. Dynamic funduscopy achieved by digital compression or a 3-mirror examination can result in the diminished size or disappearance of varices. In cases where prompt diagnosis is challenging, further investigation with ultrasound B-scan, fluorescein angiography (FA)/indocyanine green angiography (ICG), or optical coherence tomography (OCT) scans may be necessary to confirm the diagnosis.
Signs
Signs of vortex vein varicosis on examination include dilated, tortuous veins in the vortex ampullae region, often appearing bluish or purplish in color.
Symptoms
Vortex vein varices typically do not cause specific symptoms, and many cases are incidentally discovered during routine eye examinations or evaluations for other ocular conditions. However, in some instances, patients may report nonspecific visual symptoms or discomfort that may or may not be directly attributable to the varices. It is essential for patients to undergo a thorough ophthalmic evaluation if they experience any visual symptoms or discomfort, as these symptoms may also be indicative of other, potentially more serious ocular conditions.
Diagnosis
Diagnosis of vortex vein varices typically involves clinical evaluation supported by imaging studies. During a comprehensive eye examination, ophthalmologists may observe characteristic signs such as unilateral or bilateral brownish-red to gray-colored pouch or teardrop subretinal structures, often located at oblique meridians of the equator. These elevations may range from 1 to 3 disc diameters in size, with larger variations reported.
Digital compression or examination with a 3-mirror lens may result in the reduction or disappearance of these elevations, which is a key feature for diagnosis. This dynamic funduscopic finding, coupled with patient history and clinical presentation, provides valuable diagnostic information. Once the diagnosis is confirmed, further unnecessary investigations should be avoided.
However, in cases where clinical examination alone is inconclusive or further assessment is necessary, additional imaging modalities such as optical coherence tomography (OCT), indocyanine green angiography (ICGA), or ultrasound imaging may be utilized.
On spectral-domain OCT (SD-OCT), vortex vein varices typically appear as crescent-shaped elevations with larger choroidal veins merging towards the elevation. These imaging findings help confirm the diagnosis and provide valuable information about the morphology and extent of the varices.
Overall, the combination of clinical evaluation, dynamic funduscopy, and imaging studies allows for accurate diagnosis and assessment of vortex vein varices, facilitating appropriate management and follow-up care.
Diagnostic procedures
Diagnostic procedures for vortex vein varicosis may include indocyanine green angiography (ICGA), optical coherence tomography (OCT), or ultrasound imaging to visualize the dilated vortex veins and assess choroidal circulation.
- Dynamic Funduscopy:
- Dynamic funduscopy involves observing changes in the appearance of varices with alterations in gaze direction or external pressure. Varices may diminish or disappear entirely upon digital compression or during examination with a 3-mirror lens. This dynamic behavior aids in distinguishing vortex vein varices from other ocular lesions. The dynamic nature of varices, such as changes in size with Valsalva maneuver, pressure on the globe, and different gaze and body posture, along with a predominant nasal location, assists in accurate identification.
- Dynamic Ultrasound Imaging:
- B-scan ultrasonography reveals dome-shaped, acoustically solid choroidal lesions with no extrascleral extension. Applying external pressure to the globe results in flattening of the vortex varix, aiding in diagnosis.
- Optical Coherence Tomography (OCT):
- On spectral-domain OCT (SD-OCT), vortex vein varices appear as crescent-shaped elevations with larger choroidal veins merging towards the elevation. OCT imaging provides detailed cross-sectional visualization of the varices and surrounding structures.
- Indocyanine Green Angiography (ICG):
- ICG angiography confirms the diagnosis by showing pooling of the dye in the conglomerate of ampullary veins. Fluctuations in the size of the varix with changing gaze positions and pressure on the globe can be observed on ICGA imaging.
These diagnostic procedures, utilized in combination, facilitate accurate identification and characterization of vortex vein varices, guiding appropriate management strategies.[14][15]
Laboratory test
Laboratory tests are not typically used for the diagnosis of vortex vein varicosis.
Differential diagnosis
When considering a diagnosis of vortex vein varicosis, it's essential to differentiate it from various other conditions presenting with similar manifestations. The following are differential diagnoses to consider:
- Posterior exudative hemorrhagic chorioretinopathy (PEHCR) or Peripheral AMD or PCV
- Choroidal hemangioma
- Choroidal tumors including melanoma or metastases
- Suprachoroidal hemorrhage
- Subretinal hemorrhage
- Abnormalities of the chorioretinal vasculature
- Choroidal congestion or effusion
- Central serous chorioretinopathy (CSCR)
- Vogt-Koyanagi-Harada (VKH) syndrome
Considering these differential diagnoses is crucial for accurate diagnosis and appropriate management of patients presenting with features suggestive of vortex vein varicosis.
Management
Management of vortex vein varicosis aims to alleviate symptoms, prevent complications, and address underlying causes when possible.
General treatment
No specific treatment: Generally, no specific treatment is available for vortex vein varicosis itself.
- Management of associated conditions: Any associated or background diseases should be treated accordingly. For example, if there are underlying conditions such as high myopia or other ocular pathologies like scleritis, these may require specific management.
Medical therapy
Medical therapy for vortex vein varicosis may involve medications to reduce choroidal congestion, control intraocular pressure, or manage associated systemic vascular diseases.
Medical follow up
NA
Surgery
NA
Surgical follow up
NA
Complications
Generally not associated with any complications. Spontaneous resolution has been reported.[16] Complications of vortex vein varicosis may include suprachoroidal hemorrhage, reported in highly myopic patients. [13]
Prognosis
The prognosis for vortex vein varicosis is generally favorable, as it typically does not cause significant symptoms or complications. Spontaneous resolution of the varices has been reported in some cases. However, in highly myopic patients, there may be a risk of complications such as suprachoroidal hemorrhage. Overall, with appropriate monitoring and management of any associated conditions, the prognosis is typically good.
Additional Resources
- EyeWiki. (n.d.). Vortex Vein Varix. https://eyewiki.aao.org/Vortex_Vein_Varix
References
- ↑ Weidmayer SL, Demirci H. The spontaneous resolution of a vortex vein varix: case report. BMC Ophthalmol. 2021 Feb 24;21(1):101. doi: 10.1186/s12886-021-01861-2. PMID: 33627084; PMCID: PMC7903696
- ↑ Shields JA, Shields CL. Non-neoplastic conditions that can simulate posterior uveal melanoma and other intraocular neoplasms. In: Shields JA, Shields CL, eds. Intraocular Tumors: An Atlas and Textbook. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:177-195.
- ↑ Shields JA, Mashayekhi A, Ra S, Shields CL. Pseudomelanomas of the posterior uveal tract: The 2006 Taylor R. Smith lecture. Retina. 2005;25(6):767-771.
- ↑ Gunduz K, Shields CL, Shields JA. Varix of the vortex vein ampulla simulating choroidal melanoma: report of four cases. Retina. 1998;18(4):343-347.
- ↑ Osher RH, Abrams GW, Yarian D, Armao D. Varix of the vortex ampulla. Am J Ophthalmol. 1981;92(5):653-660.
- ↑ Buettner H. Varix of the vortex ampulla simulating a choroidal melanoma. Am J Ophthalmol. 1990;109(5):607-608.
- ↑ Vahdani K, Kapoor B, Raman VS. Multiple vortex vein ampulla varicosities. BMJ Case Rep. doi: 0.1136/ bcr.08.2010.3223.
- ↑ Lim MC, Bateman JB, Glasgow BJ. Vortex vein exit sites. Scleral coordinates. Ophthalmology. 1995;102(6):942-946.
- ↑ Jump up to: 9.0 9.1 Cai CX, Xiong XM, Li T, Liu BQ, Huang XH, Yu SS, Lin ZQ, Wang Q, Cui JL, Lu L, Lin Y. Vortex vein engorgement and different shapes of venous drainage systems in polypoid choroidal vasculopathy vs. age‑related macular degeneration on indocyanine green angiography. Exp Ther Med. 2023 Feb 23;25(4):162. doi: 10.3892/etm.2023.11861. PMID: 36911383; PMCID: PMC9996084.
- ↑ Zhang X, Olson DJ, DiBernardo C, Davis RM, Gordon KGB. Scleritis-associated vortex vein varix masquerading as choroidal melanoma. Can J Ophthalmol. 2018 Dec;53(6):e260-e262. doi: 10.1016/j.jcjo.2018.02.002. Epub 2018 Apr 2. PMID: 30503012.
- ↑ Cabral, Diogo MD*,†; Nogueira, Vanda MD*. VARIX OF A VORTEX VEIN AMPULLA INDUCED BY NODULAR SCLERITIS. Retinal Cases & Brief Reports 16(3):p 325-328, May 2022. | DOI: 10.1097/ICB.0000000000000968
- ↑ Doi N, Uemura A, Nakao K. Complications associated with vortex vein damage in scleral buckling surgery for rhegmatogenous retinal detachment. Jpn J Ophthalmol. 1999 May-Jun;43(3):232-8. doi: 10.1016/s0021-5155(99)00009-x. PMID: 10413259.
- ↑ Jump up to: 13.0 13.1 Milani P, Mazzola M, Bergamini F. Suprachoroidal haemhorrage and vortex vein varix: A potential association. Eur J Ophthalmol. 2022 Jan;32(1):NP130-NP133. doi: 10.1177/1120672120964033. Epub 2020 Nov 2. PMID: 33135428.
- ↑ Verma A, Bacci T, Sarraf D, Freund KB, Sadda SR. Vortex Vein Imaging: What Can It Tell Us? Clin Ophthalmol. 2021 Aug 10;15:3321-3331. doi: 10.2147/OPTH.S324245. PMID: 34408390; PMCID: PMC8364369.
- ↑ Cabral, Diogo MD*,†; Nogueira, Vanda MD*. VARIX OF A VORTEX VEIN AMPULLA INDUCED BY NODULAR SCLERITIS. Retinal Cases & Brief Reports 16(3):p 325-328, May 2022. | DOI: 10.1097/ICB.0000000000000968
- ↑ Weidmayer SL, Demirci H. The spontaneous resolution of a vortex vein varix: case report. BMC Ophthalmol. 2021 Feb 24;21(1):101. doi: 10.1186/s12886-021-01861-2. PMID: 33627084; PMCID: PMC7903696.

