Vitreous Cysts
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Vitreous cysts are rare clinical entities that can occur in a normal eye or in an eye associated with other pathologies.
Disease Entity
ICD 10- CM Code H43.89- Other disorders of vitreous body
Disease
- Floating vitreous cysts are extremely rare clinical entities that are regarded as ‘ocular curiosities’. [1]
- They can either be an incidental finding in a normal eye or associated with other ocular pathologies.
- It was first described by Tansley in 1899 as an irregular spherical cyst that showed lines of pigment on its surface. [2]
Etiology
Vitreous cysts can be congenital or acquired.
Congenital Cysts [3]
- Remnants of the hyaloid vascular system
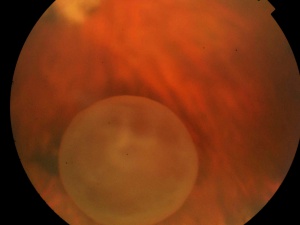
- Located at hyaloid canal and found in conjunction with a Mittendorf's dot or Bergmeister's papillae
- They are usually stable, do not progress and rarely interfere with visual acuity
- They are usually non-pigmented pearl-gray cysts with a smooth surface, can be sessile or pedunculated
- They are located anterior to the optic disc
- Some can be limited in movement due to vitreous strands attaching the cyst to the optic disc
Acquired Cysts
- They have been reported to occur secondary to or be associated with:
- Ocular trauma
- Intraocular inflammation/infection/ uveitis eg. Intermediate Uveitis, Toxoplasmosis, Echinococcus [4][5][6]
- Retinal diseases such as Retinitis pigmentosa, Choroidal atrophy, Retinoschisis, High myopia with uveal coloboma, regressed diabetic neovascularization etc. [7] [8] [9] [10]
- Retinal detachment surgeries
- They are usually symptomatic and associated with a reduction in visual acuity.[11]
Types
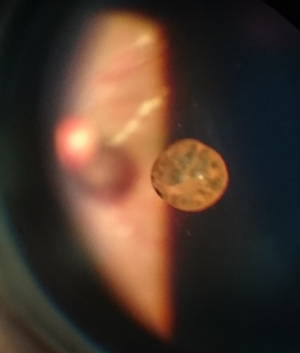
Pigmented Cysts
- Likely originate from the pigment epithelium of the iris or ciliary body and later become detached into the vitreous [12][13]
- They are brown in color
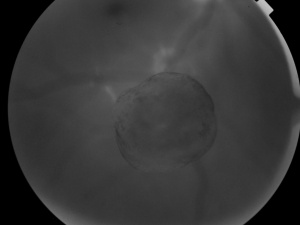
Non-Pigmented Cysts
- Congenital cysts are usually non-pigmented and originate from the hyaloidal vascular system
- They are translucent, mobile and yellow-gray in color.
General Pathology
Histopathological examination:
- Congenital cysts are choristomas (normal tissues growing in abnormal location) of the primary hyaloidal system
- Derived from the pigment epithelium of the iris or ciliary body
- Contains immature melanosomes [14]
Light & Electron Microscopy:
- Orellana et al studied aspirated pigmented cyst by light microscopy and electron microscopy. [15]
- They found that the pigmented layer of cuboidal cells contains large mature melanosomes and few immature melanosomes suggesting origin from the pigment epithelium.
- Ziu et al studied an acquired cyst removed from a patient with retinitis pigmentosa. Immunohistochemical staining of the capsule wall showed positive labeling for glial fibrillary acidic protein (GFAP), S100 (calcium binding protein), and synuclein (syn), but negative labeling for melanocyte markers (HMB45, MelanA), epithelial cell marker (cytokeratin), macrophage marker (CD68), and lymphocyte marker (CD45). These findings suggested the vitreous cyst originated from the neuroglia cell.[10]
Pathophysiology of Acquired Cysts
- Trauma can cause damage to the pigment epithelium of ciliary body and lead to pigment cysts
- Other theories have suggested the following predisposing factors: vitreous reaction to underlying retinal degeneration; ciliary adenoma breaking into the vitreous; cystic growths that occur at site of coloboma that enter the vitreous [16]
Diagnosis
These are often noted on clinical examination at the slit lamp or with funduscopy.
History
- History of ocular trauma
- History of infections or inflammation of the eye
- History of ocular surgery
- History of ocular disease such as: uveitis, uveal coloboma, retinoschisis, retinitis pigmentosa, retinal detachment and ocular malignancies
Clinical Presentation
- Age of patients usually between 10-20 years, but have been reported in younger (<10 years of age) and older (>40 years of age) patients [17][18]
- Mostly unilateral, but bilateral cases have also been reported especially in retinitis pigmentosa [19]
Symptoms
- Usually asymptomatic [19]
- When a cyst floats into and obstructs the visual axis, patients can complain of transient blurring of vision, floaters, shifting visual field defects and occasionally photophobia.
Signs and Morphological appearance of the cysts
- Numbers and Positioning: Single unilateral, Single Bilateral, Multiple unilateral
- Dimensions: 0.15-12 mm
- Shapes: Spherical, Oval, Lobulated
- Surface: Smooth or Crenated
- Color: Yellow-gray (non-pigmented) or Brown (Pigmented) [20]
- Location: Confined to the region of Cloquet’s canal[14]
The cysts can move with a patient’s eye movements while examining with an indirect ophthalmoscope.
Differential diagnosis
- A detailed clinical examination is required to rule out other infectious and malignant conditions.
- Pigmented cysts can mimic pigmented ocular tumors such as malignant melanoma. [21] [22]
- Nonpigmented cysts can mimic parasitic cysts such as Cysticercosis, Echinococcus etc.
Investigations
General Investigations:
- Complete blood count
- Erythrocyte Sedimentation Rate
- Serologies for Cysticercosis, Echinoccous, Toxpoplasma gondii, Toxocara canis
- Stool examination for ova and cysts
- Chest radiography
- Abdominal Ultrasound
- Brain computer tomography [23]
Ocular Investigations:
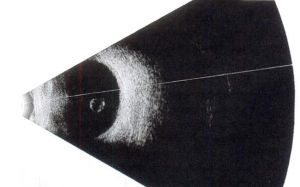
- B Scan Ultrasound to look for scolex in case of cysticercosis
- Optical coherence tomography (OCT) can also help characterize the cyst
- Ultrasound biomicroscopy (UBM) to rule out anomalies of ciliary body or posterior iris
- Fluorescein angiography – assists in characterization of intra and extra cystic vascularization [20]
Management
Asymptomatic cysts
- Observation and follow-up to determine whether there is any change in the cyst's characteristics or the patient's visual acuity.[24][25]
Symptomatic cysts
- Laser cystotomy by Argon laser or Nd:Yag laser [14] [19]
- Pars plana vitrectomy with cyst excision
- Risks of argon laser photocystotomy: Nork and Milecchia[14] reported an inadvertent retinal burn that occurred during argon green laser photocystotomy. This complication is more likely if the cyst is close to the posterior pole (due to cyst transparency) and the fovea can be damaged.
- Risks of Nd:Yag laser cystotomy: Acoustic shock waves used to mechanically breakdown the cyst wall can be transmitted to the retina. Peripheral vitreous traction can cause a retinal tear whereas perifoveal contraction can cause a macular hole.[26]
- Risks of pars plana vitrectomy with cyst excision: Associated with cataract development in young, phakic eyes.[27]
References
- ↑ Duke-Elder S. System of Ophthalmology. Vol. 3. Normal and Abnormal Development. Part 2.Congenital Deformities. London: Henry Kimpton, 1964:763
- ↑ Tansley JO. “Cyst of the vitreous”. Transactions of the American Ophthalmological Society 8 (1899): 507-509.
- ↑ Bullock JD. Developmental vitreous cysts. Arch Ophthal. 1974;91:83–84.
- ↑ Pannarale C. On a case of preretinal mobile cysts in a subject affected by congenital toxoplasmosis (in Italian) G Ital Oftalmol. 1964;17:306–317.
- ↑ Tranos PG, Ferrante P, Pavesio C. Posterior vitreous cyst and intermediate uveitis. Eye. 2010;24:1115–1116.
- ↑ Patil NS, Rayat JS. Pigmented congenital vitreous cyst in a patient with positive Echinococcus serology. Can J Ophthalmol. 2022 Dec;57(6):e195.
- ↑ Tuncer S, Bayramoglu S. Pigmented free-floating vitreous cyst in a patient with high myopia and uveal coloboma simulating choroidal melanoma. Ophthalmic Surg Lasers Imaging. 2011;42(Online):e49–e52
- ↑ Asiyo-Vogel MN, el-Hifnawiel-S, Laqua H. Ultrastructural features of a solitary vitreous cyst. Retina. 1996;16:250–254.
- ↑ Mannino G, Malagola R, Abdolrahimzadeh S, Villani GM, Recupero SM. Ultrasound biomicroscopy of the peripheral retina and the ciliary body in degenerative retinoschisis associated with pars plana cysts. Br J Ophthalmol. 2001;85:976–982.
- ↑ 10.0 10.1 Tao Z, Liu N, Duan G, Wu N. Neuroglia Cell-Originated Vitreous Cyst in a Retinitis Pigmentosa Patient. Asia Pac J Ophthalmol (Phila). 2022. Epub ahead of print.
- ↑ Bayraktar Z, Kapran Z, Ozdogan S. Pigmented Congenital Vitreous Cyst. Eur J Ophthalmol. 2004;14(2):156-158.
- ↑ Lisch W, Rochels R. Pathogenesis of congenital vitreous cysts (in German) Klin Monbl Augenheilkd. 1989;195:375–378.
- ↑ Bullock J. Developmental Vitreous Cysts. Archives of Ophthalmology. 1974;91(1):83-84.
- ↑ 14.0 14.1 14.2 14.3 Nork TM, Millecchia LL. Treatment and histopathology of a congenital vitreous cyst. Ophthalmology. 1998;105:825–830.
- ↑ Orellana J, O'Malley RE, McPherson AR, Font RL. Pigmented free-floating vitreous cysts in two young adults. Electron microscopic observations. Ophthalmology. 1985;92:297–302
- ↑ Lavric A, Urbancic M. Floating vitreous cyst: two clinical cases. Case Rep Ophthalmol. 2013;4(3):243–247. doi: 10.1159/000356569.
- ↑ Guo X, Lei B, Gao Y. A Pigmented Vitreous Cyst Within the Posterior Precortical Vitreous Pocket. JAMA Ophthalmol. 2022 Jan 1;140(1):e214681.
- ↑ Cao JA, Dubovy SR, Fan KC, Parvus MN, Fortun JA, Wykoff CC. Free-Floating Pigmented Vitreous Cysts: Clinical-Histopathologic Correlation. Ophthalmic Surg Lasers Imaging Retina. 2024 Jan;55(1):55-58. doi: 10.3928/23258160-20231108-03. Epub 2024 Jan 1. PMID: 38189800.
- ↑ 19.0 19.1 19.2 Jones WL. Free-floating vitreous cyst. Optom Vis Sci. 1998;75:171–173.
- ↑ 20.0 20.1 Cruciani F., et al. “Monolateral idiopathic cyst of the vitreous”. Acta Ophthalmologica Scandinavica 77.5 (1999): 601-603.
- ↑ Wood TR, Binder PS. Intravitreal and intracameral cysticercosis. Ann Ophthalmol. 1979;11:1033–1036.
- ↑ Tuncer S, Bayramoglu S. Pigmented free-floating vitreous cyst in a patient with high myopia and uveal coloboma simulating choroidal melanoma. Ophthalmic Surg Lasers Imaging. 2011;42(Online):e49–e52.
- ↑ Gupta SR, Gupta N, Anand R & Dhawan S (2012): Idiopathic pigmented vitreous cyst. Arch Ophthalmol 130: 1494–1496.
- ↑ Kumar DA, Balarman P, & Agarwal A. Persistent asymptomatic vitreous cyst with ten years follow-up: A case report. Indian J Ophthalmol. 2020; 68(10): 2286-2287.
- ↑ Zhu C, Liu C, Wang J. Four-Year Follow-Up of a Pigmented Vitreous Cyst. JAMA Ophthalmol. 2023;141(12):e232964. doi:10.1001/jamaophthalmol.2023.2964
- ↑ Ruby AJ, Jampol LM. Nd:YAG treatment of a posterior vitreous cyst. Am J Ophthalmol. 1990 Oct 15;110(4):428-9.
- ↑ Gulkilik G, Odabasi M, Erdur SK, Ozsutcu M, Eliacik M, Demirci G, Kocabora MS. A case of pigmented, free-floating vitreous cyst treated with micropulse diode laser. Clin Exp Optom. 2016 Jan;99(1):90-2.