Visual Allesthesia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
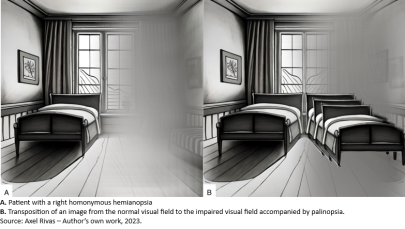
Visual allesthesia is a rare disorder of unknown pathophysiology that is characterized by transposition or rotation of the visual field.[1] Transposition as described in the literature is detection of images from an undamaged field of view to the defective/visually impaired field. [2]
The primary manifestation of visual allesthesia is perception of images/objects occurring at a position in the visual field remote from where the stimulus originated from.[3] This coincides with the pathology of palinopsia.[3] Palinopsia, or ghost images, has been commonly associated in the literature with visual allesthesia. [4] [5] [6] Allesthesia is transient, lasting 10-20 minutes[1] with the episodes occurring in periods of days to weeks.[7]
Pathophysiology
Hypothesized pathophysiology is disorganized integration of visual and in some cases vestibular excitation in the posterior parietal and occipital cortex.[1] Neuroimaging and symptoms suggest that transfer of information between hemispheres from the undamaged contralateral field to the injured cortex leads to ghost images(palinopsia) and allesthesia of images in the partially blind field.[1] Baumeler et al[3] propose that visual allesthesia and palinopsia are due to involuntary activation of contralateral homotopic visual cortex areas following unilateral activation. This activation alongside a lack of inhibitory signals following damage to the parieto-occipital cortex can lead to the phenomenon of visual allesthesia.[3]
Etiology
Few case studies can be found in the literature and are associated with lesions of the parietal and occipital lobe. [5][8] Case studies have shown visual allesthesia in patients with neurocysticercosis,[4] mitochondrial disease,[8] gunshot injury[9] and occipital lobe brain tumors.[2] The most common cause of visual allesthesia is throught to be due to an acute right parietal stroke.[9] Any lesion in this area can be the cause of visual allesthesia with the underlying mechanism hypothesized as the transfer of visual information from the right hemifield into the left hemifield with lack of inhibition.[9] Inclusion of faulty integration of visual inputs at the medulla (Wallenberg’s syndrome) or at the site of integration in occipital/parietal cortices have also been associated.[1]
Symptoms
- Patients may describe the detection of images seen in their normal visual field that are now appearing in their impaired visual field i.e. transposition.
- Symptoms include a feeling of a distorted or rotated environment.[1] Visual allesthesia and palinopsia which are described as a form of illusion are correlated in patients with focal cerebral lesions.[3]
- Disturbances in color perception have also been reported in patients with cerebral lesions; these include glioblastoma[2] and calcified cysticercus.[4] Color perception disturbances include color blindness as well as episodes of blinking colored lights in the visual field for several seconds.[2][4]
Risk Factors/Case Studies
- Arterial occlusion- Ardila et al[4] described a second case which displayed a left homonymous hemianopsia due to right posterior cerebral artery occlusion. The patient experienced the impression that objects located on the left visual field moved closer toward him, palinopsia was also present. Most cases in the literature report association with right temporo-occipital lesions; lesions on the left side are described as unconventional visual allesthesia.[4]
- Hemorrhagic stroke patients reported illusory perception of contralesional stimulus when shown on the ipsilesional side,[3] similar to other cases of visual allesthesia described in the literature. Baumeler et al[3] hypothesize this is due to an automatic response from the visual cortex to the stimulus with a lack of inhibitory feedback from the parietal lobe. Any lesion in this area can be the etiology of visual allesthesia. The underlying mechanism is the transfer of visual information from the right hemifield into the left hemifield with lack of inhibition.[9]
- A patient with an arteriovenous malformation of the right occipital lobe exhibited episodes of visual allesthesia 6 months following excision of the vascular lesion. Episodes of allesthesia were preceded by left homonymous hemianopsia post-operatively and generalized convulsions. Allesthesia in this case manifested as transpositions of images that occurred from the normal side to the affected right side. An MRI following these episodes showed a postoperative lesion which was speculated to be from irritation of the surrounding areas. This lesion affected the regions from the posterior half of the right temporal lobe to the occipital and parietal cortex.[5] Lesions in these areas have been shown to be risk factors for episodes of visual allesthesia.
- Mitochondrial disease- As described in Murakami H, et al[8], a 49-year-old man presented with right visual field hemianopia following tonic-clonic convulsions, convulsions were believed to be related to mitochondrial disease. A right homonymous hemianopsia was present. Objects present on his right visual field were perceived on the contralateral left visual field.[8] This case of visual allesthesia is hypothesized to have resulted from contralateral transmission of visual information obtained by blindsight, with the overall cause being epileptic excitement.[8] Cortical blindness in the right field with hemianopsia is hypothesized to be incomplete, with concurrent epileptic excitation of the cerebral cortex, which lead to sustained transduction of neural information.[4] [8] [9]
- Neurocysticercosis- Lesions of the occipital cortex have been shown to be associated with visual allesthesia and palinopsia.[4][9] Ardila et al[4] described a case with confirmed neurocysticercosis of the left occipital and right parietal areas with intact visual fields on admission. On the 5th day of admission the patient endured generalized seizures and reported visual blackouts. The next day right sided monocular diplopia and right homonymous hemianopia with palinopsia were reported. Palinopsia reported in the right visual field lasted for 1 hour. Images crossed over to the left visual field and disappeared with this pattern occurring multiple times.[4]
- Ventriculoperitoneal shunt located in the right parieto-occipital cortex for normal pressure hydrocephalus had episodes of visual allesthesia with a 90-degree rotation of his visual field. Hypothesized pathophysiology was like other cases of disordered integration of visual stimuli and in this case vestibular excitation in the posterior parietal and occipital cortex.[1] Overall signs and symptoms suggest that transfer of information between hemispheres from the undamaged contralateral field to the injured cortex, leading to ghost images and allesthesia of images from a partially blind field.[1] This is described as a nonclassic case of visual allesthesia. The underlying pathophysiology is similar to a problem of sensory input and disordered integration leading to faulty interpretation of the environment. The right parieto-occipital cortex supports the vestibular and ocular system in the internal representation of space.[1]
Diagnosis
Diagnosis is currently based on clinical observations alongside neuroimaging including CT and MRI scans.[7] These scans aid in uncovering underlying conditions and lesions in the temporal, parietal or occipital cortex. Based on case studies, lesions in these areas can produce visual allesthesia. Neuroimaging examining cortical activation can further show activation of contralateral lesions with unilateral stimulus.[3] Electroencephalogram may be helpful to rule out an underlying epileptic focus.[8]
Management
There are no formal guidelines on the management of visual allesthesia. Treatment is supportive depending on the etiology of visual allesthesia.[7]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Girkin, Christopher A. M.D.; Perry, Julian D. M.D.; Miller, Neil R. M.D.. Visual Environmental Rotation: A Novel Disorder of Visiospatial Integration. Journal of Neuro-Ophthalmology 19(1):p 13-16, March 1999.
- ↑ 2.0 2.1 2.2 2.3 A. Reptsis, I. Demirtzoglou, A. Nikolakopoulos, D. Almaliotis, A. Cheva and V. Karampatakis, "Visual Allesthesia in a Patient with Glioblastoma Multiforme," Open Journal of Ophthalmology, Vol. 2 No. 3, 2012, pp. 97-102. doi: 10.4236/ojoph.2012.23021.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Baumeler D, Born S, Burra N, Ptak R. When Left is One and Right is Double: An Experimental Investigation of Visual Allesthesia after Right Parietal Damage. Vision (Basel). 2020 Mar 1;4(1):16. doi: 10.3390/vision4010016. PMID: 32121533; PMCID: PMC7157701.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Alfredo Ardila, Manuel Botero & Jaime Gomez (1987) Palinopsia and Visual Allesthesia, International Journal of Neuroscience, 32:3-4, 775-782, DOI: 10.3109/00207458709043332
- ↑ 5.0 5.1 5.2 Nakajima M, Yasue M, Kaito N, Kamikubo T, Sakai H. [A case of visual allesthesia]. No To Shinkei. 1991 Nov;43(11):1081-5. Japanese. PMID: 1799515.
- ↑ Lawrence Jacobs, “Visual allesthesia,” Neurology Oct 1980, 30 (10) 1059; DOI: 10.1212/WNL.30.10.1059
- ↑ 7.0 7.1 7.2 Pane A, Miller NR, Burdon MA. Chapter 7. In: The Neuro-Ophthalmology Survival Guide. 2nd ed. Amsterdam: Elsevier; 2018:Chapter 7: 253-264.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Murakami H, Ichikawa H, Sugimoto A, Futamura A, Shimizu Y, Sugie M, Miller MW, Kawamura M. Perceiving "ghost" images: a unique case of visual allesthesia with hemianopsia in mitochondrial disease. Neuropsychiatr Dis Treat. 2014 Jun 5;10:999-1002. doi: 10.2147/NDT.S61582. PMID: 24940064; PMCID: PMC4051797.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Mendez MF, Chen JW. Epilepsy partialis continua with visual allesthesia. J Neurol. 2009 Jun;256(6):1009-11. doi: 10.1007/s00415-009-5031-8. Epub 2009 Feb 25. PMID: 19240953; PMCID: PMC2698976.